- home
- Articles about cholelithiasis
- This is useful to know
- About the structure of the human body
- Catalog of useful medical articles
›
›
›
›
You will learn from this article about where bile is formed, its composition, the role of bile in digestion, and bile enzymes.
But the main thing you will learn is the functions of bile. Why is it needed in the human body, what is the role of this liquid in the life of the human body. Sections of the article
What is bile
Where does bile formation occur?
What is the composition of bile
What are the functions of bile
Bile enzymes
Where does bile accumulate?
The gallbladder is a storage reservoir for bile. During the active phase of digestion, when partially digested food enters the duodenum from the stomach, the maximum amount of it is released there. The main functions of human bile are participation in digestion and stimulation of secretory activity and motility of the small intestine, which also ensures the processing of the bolus of food.
Bile that is secreted into the digestive tract from the gallbladder is called mature, and that secreted directly by the liver is called young, or hepatic.
Digestion in the small and large intestines. The role of bile in digestion.
Digestion in the duodenum. Chyme is at 12-. intestine for a very short time, so it is impossible to talk about any processing of it in the cavity of the 12-point intestine. The food mass (chyme) entering the duodenum is exposed to the action of pancreatic juice, bile, as well as the juice of the Brunner and Lieberkühn glands of the 12th intestine. Outside of digestion, the contents of the 12-point intestine have a weakly alkaline reaction (pH 7.2-8.0). When portions of acidic gastric contents pass into it, the reaction in the intestine becomes acidic and then gradually normalizes. In humans, in this regard, the reaction in the intestine ranges from 4.0 to 8.5 pH.
Methods for studying pancreatic secretion - removal of the duct to the outside according to Pavlov, Orlov (better). It is difficult to obtain pure juice from humans; by probing, a mixture of juices is obtained. With endoscopic examination, it is possible to penetrate the duct, but this is not always possible.
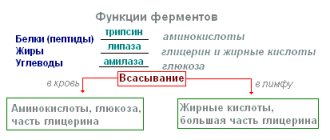
Composition and properties of pancreatic juice . The juice secreted by the pancreas is a clear liquid of an alkaline reaction (pH 7.8-8.4), which is due to the presence of bicarbonates in the juice. The juice is rich in enzymes. It contains trypsin, chymotrypsin, carboxypolypetidase, aminopolypeptidase, lipase, amylase, maltase, lactase, nucleases, etc.
The gland secretes trypsin and chymotrypsin in an inactive state. When they come into contact with intestinal juice, they are activated. Activation of trypsinogen and its transition to active trypsin occurs under the action of enterokinase in intestinal juice. Chymotrypsin is activated by trypsin. The activation process involves the cleavage of a 6 amino acid peptide from the inactive enzyme.
Under the influence of trypsin and chymotrypsin, the alkaline reaction of the environment causes the breakdown of both the proteins themselves and the products of their breakdown - high-molecular polypeptides. In this case, a large number of low molecular weight peptides and a small amount of amino acids are formed. Trypsin and chymotrypsin act on different chemical bonds in the protein molecule. Pancreatic lipase breaks down fats, its effect is enhanced in the presence of bile.
The secretion of pancreatic juice begins 2-3 minutes after eating and lasts 6-14 hours, depending on the composition of the food. On an empty stomach, pancreatic juice is secreted only in small quantities during periodic activity of the digestive tract. The amount of juice and its enzyme composition depend on the quality of the incoming chyme.
The largest amount of juice is released for meat in the second hour, for bread - in the first hour, for milk - in the third hour, i.e. the same as gastric juice. With meat foods containing little fat, a person will secrete 2.5 times more juice than with foods rich in fat. When the nature of nutrition changes, the enzyme composition of the juice also changes.
Regulation of pancreatic secretion is carried out by nervous and humoral mechanisms. The secretory nerve is the vagus. Its irritation is caused by the secretion of pancreatic juice with high enzymatic activity. The sympathetic nerve inhibits the secretion of pancreatic juice.
Reflex triggers for the secretion of pancreatic juice are irritation of taste and olfactory receptors, chewing, and swallowing. Conditioned reflex influences are also distinct.
Humoral regulation of pancreatic secretion is carried out due to the formation by cells of the 12-gut and pyloric part of the stomach of several hormones that activate pancreatic secretion. In 1902, secretin was discovered (by Baylis and Starling). This was actually the first hormone discovered. Secretin is formed from inactive prosecretin when the intestinal mucosa is exposed to acid, peptones and hypertonic solutions. As a result, the entry of acidic gastric contents into the 12-unit stomach is a powerful irritant of pancreatic secretion. The intensity of the secretory reaction of pancreatic cells and the introduction of secretin is regulated by the nervous system.
In addition to secretin, pancreozymin, which stimulates the formation of enzymes in the pancreas, was also found in the composition of the 12-point intestine extracts. The irritants that cause the formation of pancreozymin are peptones, amino acids, fats and fatty acids.
It has been shown that during humoral stimulation, predominantly inactive trypsinogen is released, and when the vagus is irritated, active trypsin is released, capable of digesting proteins without prior activation by enterokinase.
The reflex mechanism of pancreatic juice secretion is the same as gastric juice. There are two phases of pancreatic juice secretion - cerebral (complex - reflex) and intestinal (neurohumoral).
Bile, its formation and participation in digestion . Bile is a product of the secretory work of liver cells. It takes a very diverse part in the digestive processes, ensuring the absorption of fats:
1) activates lipase of pancreatic and intestinal juices;
2) emulsifies fats, thereby promoting their breakdown;
3) promotes the absorption of fats;
4) enhances intestinal motility.
Violation of the flow of bile into the intestines leads to a decrease in the absorption of fats.
The formation of bile in liver cells is continuous, but its release from the common bile duct occurs only after food enters the stomach and intestines. Outside of digestion, bile enters the gallbladder. In the bubble it concentrates 7-10 times, becomes thicker and darker.
The specific substances that make up bile are bile acids and bilirubin. In addition, bile contains lecithin, cholesterol, fats, soaps, mucin, and inorganic salts. The reaction of bile is slightly alkaline. A person secretes 500-700 ml of bile per day.
Fatty acids are formed in the liver from cholic and chenodeoxycholic acids and glycol with taurine. Bilirubin is from the breakdown products of hemoglobin in red blood cells, partly by the liver, and also in the bone marrow, spleen, lymph nodes, i.e. in RES cells.
The formation of bile is stimulated by gastrin, secretin, meat extractives, and bile itself.
Bile secretion . They are examined using fistulas, probing, endoscopically, radiographically, and ultrasound. The entry of bile into the 12-point intestine occurs a short time (5-10 minutes) after eating. The bile secretion curve is different after eating different foods. The most powerful triggers for the release of bile into the intestine are egg yolks, milk, meat and fats. Bile secretion continues for several hours and stops with the release of the last portion of food from the stomach. The first portions are cystic bile, the last portions are hepatic bile.
Bile secretion is caused by the coordinated activity of the gallbladder and the sphincter of the common bile duct.
The release of bile into the intestine occurs under the influence of reflex and humoral mechanisms. The reflex mechanism of bile secretion manifests itself during unconditioned reflex irritations of the stomach, intestines, oral cavity, pharynx and esophagus, as well as during conditioned reflex influences.
The influence of the nervous system on the biliary apparatus is carried out through the vagus and sympathetic nerves. Under the influence of impulses flowing through these nerves, the sphincter of the common bile duct opens or closes and the gallbladder contracts or relaxes. Weak irritation of the vagus causes relaxation of the sphincter of the common bile duct and contraction of the bladder, strong irritation of the vagus causes the opposite effect.
In the mucous membrane of the 12-point intestine, under the influence of the digestion products of proteins and fats, a special chemical causative agent of gallbladder movements is formed - cholecystokinin. It increases the contractions of the gallbladder and causes it to empty during digestion. Used in the clinic. Recently it turned out that it is similar to the previously described pancreozymin.
The role of the duodenum in digestion. Glands 12-p. intestines . In the mucous membrane there are 12-p. The intestines contain a large number of Brunner's and Lieberkühn's glands. In their structure and function, Brunner's glands are similar to the glands of the pyloric part of the stomach and are located in the upper part of the intestine. The juice of the Brunner's glands is a thick, colorless liquid of an alkaline reaction, contains a lot of mucus, an enzyme similar to pepsin and acting in an acidic environment, has a weak effect on starch and fat and activates the action of pancreatic enzymes. Lieberkühn's glands are typical intestinal glands that secrete intestinal juice, which complements the action of stomach enzymes and pancreatic juice.
Due to the short residence time of chyme in 12-p. There is virtually no real chemical processing going on here in the gut. The chyme is only moistened with the juices of the pancreas and the intestine itself, with bile and goes further into the small intestine, where the main chemical processing of food by these juices occurs.
However, the role of the 12-point intestine in digestion does not end there. It is the most important endocrine organ , secreting up to 20 so-called into the blood. digestive hormones that affect the activity of all parts of the ECT (secretin, panreosimin, cholecystokinin, villikinin, substance P, etc.).
Finally, 12-p. the intestine is a reflexogenic zone from which reflexes begin, regulating not only bile excretion and evacuation of food from the stomach, but also the functioning of the intestines, salivary glands, and the entire gastrointestinal apparatus as a whole.
Digestion in the small intestines . Along the entire mucous membrane of the small intestine are Lieberkühn's glands, which secrete intestinal juice, which by its action complements the digestive effect of gastric and pancreatic juice. Intestinal juice is a colorless liquid, cloudy from mucus, epithelial cells, and cholesterol crystals. This juice contains sodium chloride and a small amount of carbon dioxide salts and has an alkaline reaction.
In addition to enterokinase, intestinal juice contains proteolytic enzymes (carboxypolypeptidase, aminopolypeptidase, dipetidase, etc.), nucleases, lipases, amylase, maltase, invertase, lactase, acid and alkaline phosphatases, etc. This complex of enzymes was previously called erepsin. Enzymes of intestinal juice are capable of breaking down any food substances into final products, but they act especially well not on whole molecules, but on their fragments.
Mechanical and some chemical irritants of the intestinal mucosa (gastric juice, protein digestion products, soaps, milk sugar, etc.) cause an increase in the secretion of juice. The secretion of intestinal glands during such irritation is caused by a peripheral reflex, which is carried out due to the intra-wall reflex arcs (enteric autonomic nervous system).
It has been shown that only 20-30% of intestinal enzymes enter the intestinal cavity and, along with enzymes of the stomach and pancreas, participate in cavity digestion. Most of the intestinal enzymes remain on the surface of the membrane of epithelial cells and provide parietal, membrane digestion, the object of which is mainly oligomers (di- and trimers). They are broken down into monomers, which are immediately absorbed by the intestinal membrane into the blood.
Motor function of the small intestines . Movements of the small intestines occur as a result of coordinated contractions of transverse and longitudinal muscle fibers. This coordination is carried out by the enterin autonomic nervous system, which includes three nerve plexuses - submucosal, intermuscular and subserous.
There are three types of movements - rhythmic, pendulum-like and peristaltic, or propulsive .
The physiological significance of pendulum-like movements is to mix the intestinal contents with digestive juices and regulate absorption. In this case, alternating contractions of longitudinal and circular muscle fibers occur. Their rhythm reaches up to 20 per minute.
During peristalsis, the contents of the intestine move only in the caudal direction. The organization of propulsion has several biomechanical methods, proven x-ray and experimentally: movement of a narrow band of contraction; “water pistol” (first, the pressure increases in the segment between the two contraction stripes, then it opens and the contents are, as it were, shot out in the caudal direction); pendulum-like contractions with constant forward movement (one step back, two steps forward); “moving spindle”, when a segment, while moving through the intestine, retains its shape (two waves of contraction occur at the same speed).
Rhythmic contractions of the intestinal muscles occur against the background of constant tone of the intestinal muscles.
Smooth muscle fibers of the intestine have automaticity of myogenic origin. Pacemakers are located in the initial sections of the small and jejunal intestines. The role of the Auerbach and Meissner plexuses is only to coordinate the contractions of the longitudinal and circular muscles. The extra organ autonomic nervous system only modulates its own automation, with the parasympatheticus enhancing it and the sympathicus inhibiting it.
Humoral stimuli that stimulate intestinal movements, in addition to acetylcholine and choline, are enterocrinin and serotonin (12-gut hormones). Meat extracts, cabbage broth, bile, and salts also affect motor skills.
Reflex changes in the contractions of the smooth muscles of the intestinal wall occur as a result of mechanical and chemical irritations of the intestinal mucosa.
Digestion in the large intestine . From the small intestines, the unabsorbed part of the food passes into the cecum through the so-called. ileocecal sphincter, which acts as a valve that prevents the passage of chyme from the large intestines to the small intestines. It opens periodically (every 1-4 minutes) and lets through up to 15 ml at a time. The opening of the sphincter is the result of reflexes from the stomach and intestines.
For the digestion of food, the human colon is of little importance, since food is almost completely digested and absorbed in the small intestine, with the exception of fiber. However, digestion continues in it due to the juices coming from above.
The large intestines contain a rich bacterial flora that causes the fermentation of carbohydrates and the putrefaction of proteins. As a result of microbial fermentation in the large intestines, part of the plant fiber is broken down. This is especially important for herbivores. Their large intestines are longer. Under the influence of putrefactive bacteria in the large intestines, unabsorbed amino acids and other products of protein digestion are destroyed. In this case, a number of toxic compounds are formed (indole, skatole, phenol, etc., which are normally neutralized in the liver.
The large intestines absorb water and form feces. It contains mucus, remnants of dead epithelium of the mucous membrane, cholesterol, products of changes in bile pigments, insoluble salts, bacteria (up to 30-40% of weight), plant fiber, keratins, collagen. When digestive processes are disrupted, undigested food remains, proteins, fats, and carbohydrates are found in the stool.
In general, the entire digestion process lasts about 1-2 days in humans, of which more than half of the time is spent moving food debris through the large intestines. Motor activity is excited mainly by mechanical irritations of the mucous membrane.
Defecation . The sphincters of the rectum (internal and external) are located
in a state of continuous tonic contraction. Emptying the large intestines and releasing them from feces occurs as a result of irritation of the sensory nerves of the rectal mucosa by feces. As a result of reflex relaxation of the sphincters, the exit from the intestine opens and feces are expelled by peristaltic movements of the colon and rectum. This is facilitated by contraction of the abdominal muscles.
The reflex center is in the sacral region. The external sphincter is subject to voluntary control from the cortex. The voluntary opening of the external sphincter excites the center of defecation and it can occur at a convenient moment for the person.
Suction. Absorption is the penetration from the external environment and
body cavities into the blood and lymph of various substances through one or more layers of cells that form complex biological membranes. The latter include the epithelium of the skin, mucous membranes, endothelium of the serous membranes and capillaries, epithelium of the renal tubules, etc. All biological membranes, single-layer or multilayer, are semi-permeable, since they have one-way permeability to many substances. Through absorption in the digestive canal, the body receives the nutrients it needs.
Absorption can occur throughout the gastrointestinal tract, starting from the oral cavity, but its volume depends on the time the food remains in this section. In the stomach, absorption occurs only to a small extent. Mineral salts, monosaccharides, alcohol and water are absorbed here very slowly. Few substances are absorbed in the 12-gut.
The most intense absorption occurs in the jejunum and ileum. It is believed that absorption in the intestine can reach 2-3 liters. at one o'clock. This is possible only because, due to the presence of folds and villi, the absorption surface of the intestine greatly increases. The membrane through which absorption occurs is formed by the so-called marginal epithelium. The border is formed by microvilli, on the surface of which contact digestion occurs. Nutrient absorption in the large intestine is low under normal physiological conditions, since most nutrients are absorbed in the small intestine. Normally, the large intestines absorb about 1 liter of water per day.
The suction mechanism is complex. In this process the following are important:
1. Filtration, which occurs along a pressure gradient in the intestine-blood or lymph system. Increasing the pressure in the intestine to 8-10 mmHg accelerates the absorption of table salt solution by half. But if the pressure increases to 30-50 mm, then absorption stops due to compression of the villi and blood vessels of the intestinal walls.
2. Diffusion of substances along a concentration gradient.
3. Osmosis of water with dissolved substances along the osmotic pressure gradient. 4. Active absorption using special mechanisms of transport of substances against concentration and osmotic gradients.
Among the factors involved in the absorption process, it should be noted the contractions of the smooth muscle fibers of the villi, due to which the cavity of the lacteal vessels is compressed and the lymph is squeezed out. The lymph does not flow back because of the valves. The movement of the villus creates a suction action of the central lymphatic duct of the villus. The villi shrink in fed animals. Irritants are food substances - peptides, alanine, leucine, extractives, bile acids, glucose. In the 12-point intestine, a special hormone is formed - villikinin, which stimulates the movement of the villi. The contraction of the villous muscles is regulated by the Meissnerian plexus.
Proteins are absorbed in the form of amino acids. This occurs actively through their phosphorylation in the intestinal wall. Blockade of carbohydrate-phosphorus metabolism by 2,4-dinitrophenol inhibits the absorption of amino acids. Adding ATP and inorganic phosphate to amino acid solutions enhances their absorption. When feeding on proteins of animal origin, 95-99% of the introduced protein is digested and absorbed, and when feeding on proteins of plant origin - 75-80%.
Carbohydrates are absorbed in the form of glucose and galactose. Unlike other substances, monosaccharides are absorbed most intensively at the beginning of the small intestine. Glucose absorption is an active process, since monosaccharides with smaller weight and molecular size (pentose and fructose) are absorbed more slowly than glucose. During the absorption of carbohydrates, their enzymatic phosphorylation occurs. Insulin enhances the absorption of glucose in the intestine.
Absorption of fats is the most complex process of all absorption. Fats in the digestive tract are broken down by lipases into fatty acids and mono and diglycerides. However, not all fats that enter the digestive tract are broken down, but only a part (from 35 to 70% according to various authors). It turned out that unsplit triglycerides are able to be absorbed in the digestive tract. Absorption of neutral fat begins after its emulsification, which results in the formation of a finely dispersed emulsion consisting of tiny droplets of fat, the so-called. chylomicrons.
Emulsification occurs under the influence of a complex complex consisting of bile salts and fat breakdown products (monoglycerides and fatty acid salts). Emulsified neutral fat is absorbed by the intestinal villi (via the mechanism of pinocytosis) and enters the lymphatic vessels. Fatty acids, glycerol and diglycerides, released during the breakdown of fat, passing through the epithelial layer of the intestine, are partially resynthesized into neutral fat, and partially used for the synthesis of phospholipids. Bile acids play a major role in the absorption of fatty acids, which are unique carriers of fatty acids across the membrane. Neutral fat is absorbed mainly into the lymph.
Absorption of water and mineral salts . Water enters the intestinal cavity with food and digestive juices, as well as during the filtration of blood plasma. The intestines receive about 1 liter of saliva, 1.5-2 liters of gastric juice, 1 liter of bile, 1-2 liters of pancreatic juice and 1-2 liters of intestinal gland juice - a total of 7-8 liters, not counting plasma. To this is added 2-3 liters of exogenous water. Only about 150 ml of water is excreted from the intestines with feces; the rest of the water is absorbed into the blood. Absorption of water begins in the stomach, intensively in the small intestines and less in the large intestines.
Sodium, potassium, and calcium salts dissolved in water are absorbed primarily in the small intestine. The absorption of these salts is affected by their content in the body. The motor function of the intestine takes an active part in the rate of absorption. We have already said that the villous epithelium has a brush border. Polymer products do not pass through it. They undergo cavity digestion, breaking down to fragments less than 200 angstroms in size (the distance between microvilli). The brush border contains enzymes that break down tri- and dimers of nutrients. The degree of cavity digestion depends on motility, and vice versa, since if the fragments are not removed from the cavity, they will begin to be broken down by cavity enzymes, but polymers will not (competition), and then the process of breakdown of nutrients will slow down and absorption will slow down. This means that the entire rate of absorption depends on the rate of entry of fragments into the brush border. The release of fragments from the lumen into the border is a limiting factor. This output is provided by mixing contractions of the gastrointestinal tract. The transport of fragments into the border increases.
Hence, with paralysis of the gastrointestinal tract, there is a blockade of splitting and absorption. There is a certain optimum speed of propulsion, because the speed of suction depends on the surface involved at the moment, and with peristaltic movements a new surface is brought into play. However, if the propulsion speed is high, then suction does not have time to occur. Thus, with intestinal denervation, the rate of chyme evacuation increases 8 times, and at the same time 70% of food does not have time to be digested and absorbed in the intestine. The nervous system (especially the sympathicus) inhibits automatic propulsion and enhances segmentation and mixing movements.
The process of bile formation and bile excretion
The process of producing hepatocyte secretion (choleresis) occurs continuously. They filter a number of substances from the blood into the bile capillaries. Further, due to the reabsorption of water and mineral salts, the final formation of the composition of this secretory fluid occurs. This process takes place in the bile ducts and gallbladder. Part of the bile immediately enters the intestines; it is called hepatic, or young. But the bulk of it accumulates in the gallbladder, where it moves along the bile ducts. Cystic bile accumulates, becomes thick and concentrated. It is darker than liver.
During the day, liver cells in an adult produce about two liters of secretion. On an empty stomach, it practically does not enter the intestines. After eating, bile secretion (cholekinesis) occurs into the duodenum. There, bile performs digestive, as well as bacteriostatic and regulatory functions. That is, it itself is a regulator of the process of bile formation and bile excretion.
Thus, the more bile acids are released into the portal bloodstream (portal vein), the higher their concentration in the bile composition and, accordingly, the less they are synthesized by hepatocytes. The functions of bile and pancreatic juice are basic in digestion.
Where does bile formation occur?
Bile formation occurs in the liver. Tiny liver cells cleverly extract all the necessary components from the blood, and then, using them, form this peculiar liquid or solution.
Hardworking liver cells synthesize about 500–700 ml of this fluid per day. The process of bile formation occurs continuously in the liver, although its rate fluctuates throughout the day.
Its formation occurs most intensively during the day, and at night it slows down.
The entire liver consists of tiny, but surprisingly well-organized complexes. Each such complex consists of liver cells, bile camillaries and blood vessels. This complex is called the hepatic lobule. It is here, in the hepatic lobule, that bile formation occurs.
The hepatic lobule contains everything needed for the formation of bile:
- liver cells arranged in even rows
- the thinnest bile capillaries between the rows of cells
- feeding vessels
- nerve endings
Liver cells catch the necessary substances from the blood, convert them and secrete them into the bile capillary.
The bile capillary collects the solution formed by hepatocytes and serves as the beginning of the biliary tract.
Vessels and nerve endings nourish the cells of the liver and ducts and regulate their work.
As soon as the liver cells have synthesized bile, it enters the bile capillaries and begins its movement. Ultimately, having passed its difficult path through the bile ducts, it enters the duodenum, where it takes part in digestion.
So, if we give an exact answer to the question of where bile is formed, then we must say that its formation occurs in the hepatic lobule.
A diagram that shows where bile formation occurs and how it subsequently progresses in the human body.
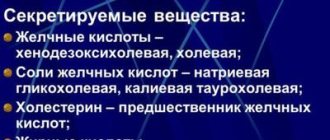
Composition of bile
The main component of bile is bile acids. The majority (67%) are cholic acid and chenodeoxycholic acid. The remaining acids are secondary, i.e. derivatives of these two acids: deoxycholic, allocholic, lithocholic and ursodeoxycholic.
All bile acids are found in this secretion in the form of compounds with taurine and glycine. The content of a large number of sodium and potassium ions gives the bile an alkaline reaction.
In addition, bile contains some organic substances:
- Phospholipids.
- Protein compounds, namely immunoglobulins A and M.
- Bilirubin and biliverdin (bile pigments).
- Cholesterol.
- Mucin.
- Lecithin.
As well as ions of some metals (zinc, copper, lead, magnesium, indium, mercury), vitamins A, B, C.
All of the listed components are included in both hepatic and bladder bile, but in the first their concentration is approximately 5 times lower than in the second.
Bile
Bile
or
bile
(Latin
bilis
, other Greek
chole
) is a fluid produced by the liver and accumulated in the gallbladder. It has a yellow, brown or greenish color, a bitter taste and a specific smell. Bile ensures the change from gastric digestion to intestinal digestion, eliminates the effect of pepsin, which is dangerous for pancreatic juice enzymes, and creates favorable conditions for these enzymes.
The bile acids contained in bile emulsify fats, activate the motility of the small intestine, stimulate the production of mucus and the gastrointensinal hormones cholecystokinin and secretin, and prevent the adhesion of bacteria and protein aggregates.
Bile is also involved in the excretion of a number of substances from the body, such as cholesterol, bilirubin, steroids, glutathione and others that are not filtered by the kidneys.
Bile production is produced by liver hepatocytes. Bile is concentrated in the bile ducts of the liver, and from there, through the common hepatic and cystic ducts, it is sent to the gallbladder and duodenum, where it participates in the digestive processes. The gallbladder acts as a container, the use of which allows the small intestine to be supplied with the maximum amount of bile during digestion, when the duodenum is filled with chyme.
Bile performs the following functions (Makhov V.M.):
- emulsification of fats
- hydrolysis and absorption of fats
- activation of pancreatic and intestinal enzymes
- participation in hydrolysis and absorption
- participation in the assimilation of fat-soluble vitamins, cholesterol, calcium salts.
Bile is a stimulant of intestinal motility, and its deficiency contributes to the development of constipation. Bile is a powerful bacteriostatic; it promotes the proliferation and desquamation of enterocytes. The alkaline pH of bile is important, and its entry into the duodenum helps neutralize hydrochloric acid and inactivate pepsin. The presence of bile in the intestine leads to stimulation of bile formation and bile excretion (Makhov V.M.).
Composition of bile
Bile has a complex composition.
This ensures that it performs various functions related to, but not limited to, the digestive process. Bile acids (primary: cholic and chenodeoxycholic; secondary and tertiary: deoxycholic, lithocholic, ursodeoxycholic and sulfolitocholic) promote lipid solubilization (emulsification, emulsion stabilization, micellization), activate the motor function of the digestive tract, stimulate the release of gastrointestinal hormones (cholecystokinin or cholecystokinin-pancreozymin , secretin), mucus secretion. The absorption of fat-soluble vitamins (A, A, E, K) depends on the presence of bile acids. Phospholipids perform a protective function in the biliary tract and provide cholesterol solubilization. The bacteriostatic properties of bile are associated with immunoglobulins. Mucus prevents bacterial adhesion. The presence of cholesterol, bilirubin, metals and organic anions (glutathione and plant steroids) is due to their excretion in the bile. Bile enhances the activity of pancreatic enzymes (mainly lipase), maintaining an optimum of =6.0 for its functioning. The acid-base properties of bile are less important for trypsin and amylase, although enterokinase, which activates trypsinogen, is active only in an alkaline environment. Bile participates in cavity digestion due to its own amylase and proteases, which it contains in small quantities.
Bile contains detergent components for mucous membranes, the damaging effect of which is reduced in the presence of lecithin. The absence of bile acids, as well as excessive acidification of the duodenum and bacterial contamination, reduce the absorption of hydrophobic substances to almost zero (Serebrova S.Yu.).
See also:
- Microscopic examination of bile / Section in the book. Polikarpov L.S., Balashova E.V., Karpukhina E.O. and others. Additional methods of examining a patient in therapeutic practice (in two parts): a textbook for students of medical universities. – Krasnoyarsk: Krasnoyarsk State Medical University printing house. – 2010. – Part 2. – 156 p. .
- Study of bile / Chapter 8 in the book. Ishmanov M.Yu., Sertakova A.V., Solovyov A.M., Fedyashina N.A., Shcherbakova E.V. 250 health indicators. Directory. From “Scientific Book”, 2013
Bile in children
Bile is secreted by the liver from the first day after birth. During this period, bile has a maximum concentration of bile acids (2.0–26.7 mEq/l). By the age of one year, the concentration of bile acids decreases to 2.2–19.7 mEq/L. The concentration of bile acids in the bile of 4–10 year old children is even lower - 2.4–5.2 mEq/L. In adults - 2.8–20.0 mEq/l. The biochemical composition of bile of children and adolescents is presented in the table (Kozlov V.I., Farber et al., 1983):
| Indicators, mEq/l | Cystic bile | Liver bile | ||
| 5–10 years | 11–15 years | 5–10 years | 11–15 years | |
| Lipids | 1583 ± 569 | 1182 ± 284 | 594 ± 188 | 366 ± 144 |
| Cholic acid | 1601 ± 215 | 1209 ± 529 | 328 ± 148 | 355 ± 131 |
| Cholesterol | 337 ± 240 | 183 ± 97 | 61 ± 32 | 56 ± 39 |
Patient Materials
The GastroScan.ru website contains materials for patients on various aspects of gastroenterology:
- “Advice from doctors” in the “Patients” section of the site
- “Popular gastroenterology” in the “Literature” section
- “Popular gastroenterology” in the “Video” section
Resources for Healthcare Professionals
On the website GastroScan.ru in the “Literature” section there is a subsection “Diseases of the hepatopancreatobiliary system”, containing publications for healthcare professionals on this topic.
Video for healthcare professionals
Still from video: Volynets G.V. Functional and inflammatory diseases of the upper digestive tract in children
Still from video: Shumkov Yu.P. Biliary reflux
On the website in the “Video” section there is a subsection “For Doctors”, containing video recordings of reports, lectures, webinars in various areas of gastroenterology for healthcare professionals.
Back to section
Functions of bile
They are mainly related to the functioning of the gastrointestinal tract. The functions of bile in digestion are associated with a number of enzymatic reactions.
- Under its influence, fats are emulsified, thereby facilitating their absorption.
- It neutralizes the harmful effects of pepsin (the main component of gastric juice), which can destroy pancreatic enzymes.
- Activates small intestinal motility.
- Stimulates mucus production.
- Activates the production of gastrointestinal hormones: secretin and cholecystokinin, which are produced by the cells of the small intestine and contribute to the regulation of the secretory function of the pancreas.
- Prevents adhesion (cohesion) of bacteria and protein components.
- It has an antiseptic effect on the intestines and takes part in the formation of feces.
Thus, the functions of bile in digestion cannot be overestimated. It is thanks to bile that the digestive process, begun in the stomach, continues and ends safely in the intestines.
Bile in the gallbladder
The substance that is located in the gallbladder is endowed with antibacterial properties. This component does not remain in the bladder for long, and therefore cannot cause any harm to the body.
In addition, during the time that the bile is located in the bladder, certain changes occur to it. Bile acids accumulate, but the bilirubin content, on the contrary, decreases. There is an accumulation of the volume that will be needed to digest the food lump.
It is very important that the ratio of all substances in bile corresponds to the norm. Poor nutrition and lifestyle cannot but affect the functioning of all organs, including the liver. As a result, the bile changes its composition and a suspension begins to form in it. In the future, disturbances in the functioning of the gallbladder can lead to the formation of stones. Read about the reasons for this here
What role does bile play in digestion?
5 (100%) 1 vote .
As soon as the food mass is in the duodenum, active secretion of bile occurs. If there is little of it, then the digestion process slows down, and therefore the breakdown of fats and some proteins is difficult. This fact easily explains that patients suffering from chronic diseases related to stagnant bile processes or insufficient bile production often face the problem of excess weight and pain in the gallbladder and liver.
Cholelithiasis
This pathology may occur due to an unbalanced composition of bile. This bile is called lithogenic. It can acquire such properties due to regular errors in the diet, namely if animal fats predominate in the food. The functions of liver bile can be impaired as a result of endocrine diseases. In addition, this liver secretion can acquire lithogenic properties as a result of lipid metabolism disorders, which, as a rule, are accompanied by an increase in the patient’s body weight. Changes in the composition of bile can also be caused by infectious and toxic liver damage or an insufficiently active lifestyle (physical inactivity).
Steatorrhea
As mentioned above, the functions of bile are related to the emulsification of fats. If for some reason bile stops flowing into the small intestine, fat absorption does not occur, and they begin to be excreted in the feces. The same thing can happen if there is a lack of bile acids in this liver secretion (a change in its composition). In this case, the feces acquire a white or gray color and a greasy consistency. This pathology is called steatorrhea. With this disease, the body lacks vital fats, fatty acids and some vitamins. As a result of steatorrhea, the lower intestines suffer, because they are not adapted to such chyme.
How is bile examined?
In order to study the composition and functions of bile, the method of fractional multi-stage duodenal intubation is used. This procedure consists of five steps:
- Basal secretion of bile - secretion of the secretion of the common bile duct and duodenum occurs. Lasts about 15 minutes.
- The phase of the secretory pause or closed sphincter of Oddi. The duration of this phase is 3 minutes.
- The phase of excretion of residual bile of portion A. Lasts about 5 minutes.
- Phase of the release of gallbladder bile portion B. This period lasts about 30 minutes.
- Hepatic bile secretion - portion C. This phase lasts approximately 20 minutes.
Thus, 3 servings of bile are obtained. They all differ in composition. The most concentrated gallbladder bile is portion B. It contains the largest amount of fatty acids, bilirubin and other bile components.
This research method allows you to determine the physical properties of bile, its composition, the volume of the gallbladder, the condition of the biliary tract and identify the localization of the pathological process.