Composition, dosage forms of the drug
The active substance of the drug is famotidine. The compound reduces the secretion of hydrochloric acid and increases the mucus content in gastric juice. The drug has two pharmaceutical forms:
- Tablets for oral use: in dosages of 20 and 40 mg, coated with soluble film. Auxiliary components: talc, starch, silicon dioxide, magnesium stearate. Sold in packs of 10–50 pcs.
- Lyophilized powder for the preparation of injection solutions: white or yellowish free-flowing substrate in ampoules. Available complete with solvent. Cardboard packages of the drug contain 5 ampoules, each containing 20 mg of Famotidine and excipients: mannitol, aspartic acid.
How does Famotidine work?
This is an antiulcer drug. It affects the functions of the gastric mucosa, comprehensively suppressing the production of hydrochloric acid:
- basal;
- stimulated by the enzymes gastrin, pepsin and acetylcholine.
As a result of acid neutralization, the pH level increases, and at the same time the protective effect of gastric secretions increases. Thanks to the production of glycoproteins, alkaline components and prostaglandins, the mucous membrane experiences less irritation, recovers and heals faster. In addition, the drug has a moderate effect on liver enzymes. This helps stop internal bleeding, prevents its development, and accelerates the scarring of ulcerative lesions.
The product dissolves in the stomach cavity within 10–15 minutes. The therapeutic effect of the drug develops over 1 hour and lasts up to 0.5–1 day. One dose of Famotidine significantly reduces the synthesis of hydrochloric acid for up to 12 hours, eliminating characteristic symptoms: stomach pain, heartburn.
Pharmacological properties of the drug Famotidine
Famotidine is an antisecretory agent, an H2 receptor blocker. Suppresses the production of hydrochloric acid, both basal and stimulated by histamine, gastrin and acetylcholine. Simultaneously with a decrease in the production of hydrochloric acid and an increase in pH, the activity of pepsin decreases. The duration of action after a single dose depends on the dose and ranges from 12 to 24 hours. After oral administration, bioavailability is 40–45%, the effect develops after 1 hour and lasts for 10–12 hours. After intravenous administration, the maximum effect develops within 30 minutes, half-life is 2.3–3.5 hours. With creatinine clearance less than 10 ml/min, the half-life of famotidine from blood plasma increases and can reach 20 hours. After oral administration, 30–35% of famotidine is excreted unchanged in the urine , and after intravenous administration - 65–70%.
Indications for use of Famotidine
The drug is prescribed for increased acidity of gastric juice and associated pathologies of the gastrointestinal tract:
- gastritis;
- attacks of heartburn, sour belching and other dyspeptic disorders;
- peptic ulcer disease, including stress ulcers;
- stomach bleeding;
- erosive lesions of the intestinal mucosa;
- Zollinger-Ellison syndrome;
- reflux esophagitis.
Famotidine is also used to prevent internal bleeding after abdominal surgery on the stomach, as a preventive measure against aspiration of digestive secretions before using endotracheal general anesthesia. In complex therapy, it is indicated to improve the condition of polyendocrine adenomatosis and mascytosis.
Journal "Emergency Medicine" 5 (36) 2011
Introduction
In medicine, as in any other creative process, one must not slide into platitudes.
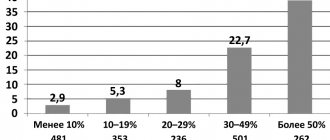
Perhaps for you, thoughtful reader, the question of the need to prescribe famotidine for acute pancreatitis has already been completely clarified, understandable and devoid of any meaning. In this case, you can skip this text and move on to other topics. On the other hand, you may have encountered a couple of meticulous patients, and perhaps even unpleasant “reasoned” complaints, the authors of which thoughtfully and in detail studied the instructions for use of this pharmacological drug. To such a meticulous patient or his relative, you can demonstrate Order of the Ministry of Health No. 297 of 04/02/2010 “On the approval of standards and clinical protocols for the provision of medical care in the specialty “surgery”, which specifically regulates the use of H2-blockers in acute pancreatitis. And then you calmly continue to engage in medical, scientific or organizational work, depending on the specialty you have chosen, sluggishly scolding the authors of the instructions in your heart and thanking the creators of the order. And if something in your soul makes you think rather than blindly follow instructions, try to find out (at least for yourself) whether it makes sense to prescribe this drug. So - risk and benefit. Eternal questions from financiers and, oddly enough, doctors. The only stake in this decision may be someone’s health, and perhaps even life. As for the risk, according to a study by IA Eland et al., the results of which were published in 2000 in the British Journal of Clinical Pharmacology and were based on data from a study of more than 180,000 patients, cases of acute pancreatitis associated with the use of famotidine (as well as nizatidine and lansoprazole), not registered. At the same time, such complications occurred when prescribing cimetidine, ranitidine and omeprazole. Their incidence ranged from 13.9 to 7.8 cases per 100,000 patients per year [1]. According to the eHealthMe website as of July 18, 2011, out of 30 million reported cases of side effects, 14,826 cases of side effects were observed with the use of famotidine [2]. Thus, overall the risk can be assessed as low.
The following question arises: why does famotidine have effects that deserve attention in the treatment of acute and exacerbation of chronic pancreatitis?
Here it is appropriate to return to the physiology of the pancreas and the pathological physiology of acute pancreatitis. In a living organism, the regulation of the production of secretions by almost all glands is carried out by the neurohumoral pathway. Moreover, the most frequently implemented mechanism is the feedback principle.
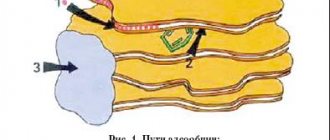
This mechanism is realized primarily by cholinergic and humoral mechanisms, including secretin and cholecystokinin. The first hormone discovered was secretin, which stimulates the production of juices and the secretion of bicarbonates. This hormone is released into the blood by S-cells of the duodenum when acidic gastric contents act on its mucous membrane. Stimulation of secretion occurs through membrane receptors and secondary messengers AC - cAMP, centroacinous and ductal cells, and, to a lesser extent, acinar cells. In this case, a secretion with a high concentration of bicarbonates and low enzymatic activity is released.
Another hormone that enhances pancreatic secretion is cholecystokininopancreozymine (CCCP). The release of the hormone into the blood from CCK cells of the mucous membrane of the duodenum and jejunum occurs under the influence of dietary chyme. The release of CCPP is enhanced in the presence of Ca2+ ions and with a decrease in pH in the duodenum (acidification).
CCK acts mainly on the acini of the pancreas. At the same time, the released juice is rich in enzymes. Secondary messengers are Ca2+ ions and the GC-cGMP complex. The simultaneous effect of secretin and CCK on the gland (with food intake) enhances the effect.
To emphasize the complexity of humoral regulation, let us recall that pancreatic secretion is also enhanced by gastrin, serotonin, insulin, bombesin, and bile salts. The secretion of pancreatic juice is inhibited by glucagon, somatostatin, vasopressin, substance P, ACTH, enkephalin, calcitonin, GIP, PP, UL. VIP can both stimulate and inhibit pancreatic secretion.
Thus, if we return to the enzymatic drama that occurs during acute pancreatitis, we should understand that with all the variety of provoking (etiological) factors, the pathogenetic mechanism is realized alone. This is autodigestion of the gland and surrounding tissues due to the phenomenon of evasion of active enzymes from the ductal system and the lumen of the digestive tract, where they should perform their main function - digestion. Therefore, with all the disputes about the effectiveness of certain drugs, with all the successful and unsuccessful searches for the “magic bullet”, the main goal of drug therapy remains the same - interruption of this process at the earliest possible stage and the most complete functional rest of the organ. This is the meaning of the classic triad: “cold, hunger and peace.” The absence of simple, safe and reliable devices that would make it possible, using hypothermia, to reversibly stop or significantly reduce the activity of secreting tissue, does not at all mean that this principle is absurd. Hunger, which is counteracted by early enteral tube feeding, has not lost its relevance in the first day of the disease and is an attempt to launch a life-saving negative feedback mechanism. No food - no need to digest it. Our trouble is that patients often do not turn to doctors in the first hours of illness, and are not able to provide rest to the gland on their own, since they continue to eat, and many drink (which is typical, not only water, but also higher-strength drinks) even with very severe pain. And sometimes only uncontrollable vomiting forces such originals to interrupt their drinking bout and appear in the emergency department. Their condition is often far from ideal.
The arsenal of pharmacological drugs and points of application of agents to ensure the rest of acinar cells is wide. This is also the long-standing heavy artillery of “desperation” - antitumor cytostatics (5-FU, ftorafur), whose effect on the body and especially on its ability to regenerate is more reminiscent of “carpet bombing”. This is also a synthetic analogue of somatostatin that has been used for quite a long time - an intellectual “toy”, a chemically reproduced regulatory hormone. Unfortunately, it never played the role of a saving “magic bullet,” either due to its weak ability to penetrate into the lesion in the required concentration, or as an example of the fact that our view of the nature of what is happening is mosaic in nature and does not reflect the full complexity of regulatory connections. Both the exotic ribonuclease and the little-understood dalargin are all used in attempts to stop secretion.
Among the more traditional drugs, along with anticholinergics (ancient atropine, progressive gastrocepin), a place is also given to drugs that reduce the acidity of gastric juice - Na / K-pump blockers and H2 blockers. This is where we meet famotidine. It should be noted that nizatidine and roxatidine are the fourth and fifth generation of histamine receptor blockers, but they are practically little different from famotidine and have no advantages over it. Therefore, famotidine (Quamatel) remains the most popular drug.
According to S.F. Bagnenko, A.D. Tolstoy et al., published in 2002, the antisecretory activity of famotidine is not inferior to octreotide, while famotidine (Kvamatel) was 8 times cheaper at that time [11].
It is generally accepted that the mechanism of action of famotidine on the pancreatocyte is double and is realized due to the fact that the histamine-dependent adenylate cyclase associated with histamine receptors is located on the pancreatocyte. The same adenylate cyclase is also present in acid-forming parietal cells of the stomach. Therefore, H2-blockers of histamine receptors inhibit histamine receptors in the pancreas, creating rest for the pancreatic cell and leading to regression of autolytic processes in the pancreas and stomach, reducing acid formation. A decrease in the acidity of gastric juice causes a less pronounced shift to the acidic side of the intraluminal environment of the duodenum, as a result of which the release of secretin, the main hormone that stimulates the function of the pancreas, decreases. However, there is an important physiological nuance: secretin, released by hydrochloric acid, stimulates hydrokinetic secretion, which leads to the release of the bicarbonate rather than the enzymatic fraction of pancreatic juice. Moreover, suppression of hydrokinetic secretion can worsen the conditions for the outflow of pancreatic juice due to an increase in its viscosity with the formation of protein plugs. That is why it is necessary to prescribe a sufficient volume of infusion therapy, aimed, among other things, at reducing the viscosity of the secretion.
Now the influence on secretory mechanisms has become clearer. What other beneficial properties are characteristic and harmful ones are not characteristic of the action of famotidine?
First of all, this is the high selectivity of its effect. Moreover, famotidine does not interact with the cytochrome P450 system during metabolism, due to this, it essentially does not have a toxic effect on the liver, in addition, because of this, there are no cross-reactions with other medications, which are almost all metabolized with the participation of cytochrome [ 3]. According to a number of researchers, famotidine has an antioxidant effect, reducing the production of reactive oxygen species by neutrophils [6, 13] and reducing platelet aggregation [3–5]. This is due to the fact that H2 blockers enhance the activity of the most important antioxidant enzyme, superoxide dismutase. It is most likely that these unique properties of H2 blockers explain the rapid positive systemic effect in the treatment of diseases of the digestive system [4, 13]. Unlike cimetidine and ranitidine, famotidine does not inhibit the activity of alcohol dehydrogenase, so it can be used in alcoholics and moderate alcohol drinkers [12]. Famotidine does not affect the level of prolactin in the blood and does not cause gynecomastia, does not have an antiandrogenic effect and does not cause impotence, unlike its predecessors. Although these qualities do not play a decisive role in short-term use [3]. And finally, last but not least, there is a form of the drug that allows it to be administered parenterally, which is especially important in intensive care, when taking drugs by mouth is impossible or dangerous.
conclusions
Having carefully analyzed all the benefits and risks of using famotidine (Kvamatel) for acute pancreatitis, it should be recognized that its use is appropriate and justified. Complex therapy aimed at stopping the process at the slightest suspicion of acute pancreatitis should be started as early as possible. The complex of therapeutic agents should include an infusion of famotidine in an adequate (40 mg) dosage. The process of further examination and clarification of the diagnosis in the case of pain in the upper abdomen should be carried out in parallel with such therapy, since the speed of development of severe and sometimes irreversible processes during autodigestion does not leave us time to think, but requires quick and decisive action.
Precautions and contraindications
The drug requires careful use in hepatosis, cirrhosis and other liver diseases, inflammation of the gallbladder, renal failure, nephritis. These pathologies increase the risk of side effects. Famotidine contraindications include:
- individual intolerance to any of its components;
- oncological diseases of the gastrointestinal tract;
- pregnancy at all stages;
- lactation period.
In pediatrics, the medication is used with caution, in doses strictly determined by the doctor, with constant monitoring of the well-being of children.
Famotidine slows down the breakdown of indirect anticoagulants, antidepressants, caffeine, drugs based on lidocaine, theophylline, metronidazole, phenytoin, buformin. This must be taken into account during simultaneous courses of treatment.
Famotidine
Famotidine
(lat.
famotidine
) - an antiulcer drug, a blocker of histamine H2 receptors.
Chemical compound:
3-[[[2-[(Aminoiminomethyl)amino]-4-thiazolyl]methyl]thio]-N-(aminosulfonyl)propanimidamide. Empirical formula: C8H15N7O2S3.
Famotidine is the international nonproprietary name (INN) of the drug. According to the pharmacological index, it belongs to the group “III generation H2-histamine receptor blockers”. According to ATC, it belongs to the group “H2-histamine receptor blockers” and has the code A02BA03. "Famotidine" is also the trade name of the drug.
Characteristic.
White or pale yellow crystalline powder. It is highly soluble in acetic acid, slightly soluble in methanol and water, and practically insoluble in ethanol.
Pharmacology
Pharmacological action
- antiulcer. Blocks histamine H2 receptors, inhibits basal and stimulated secretion of hydrochloric acid; inhibits pepsin activity.
Famotidine is not completely absorbed from the gastrointestinal tract, bioavailability is 40–45%, increases under the influence of food and decreases when using antacids. Plasma protein binding is 15–20%. Cmax is reached after 1–3 hours. 30–35% is metabolized in the liver to form S-oxide and excreted by the kidneys by glomerular filtration and tubular secretion. 25–30% of the dose taken orally and 65–70% of the dose administered intravenously are found unchanged in the urine. T½ - 2.5–3 hours. In patients with severe renal failure (creatinine Cl below 10 ml/min), it increases to 20 hours (dose adjustment required). After oral administration, the effect begins within 1 hour, reaches a maximum within 3 hours and lasts 10–12 hours. Under conditions of intravenous administration, the maximum effect develops after 30 minutes. A single dose (10 and 20 mg) suppresses secretion for 10–12 hours.
Use of famotidine.
Peptic ulcer of the stomach and duodenum (treatment and prevention of exacerbations), symptomatic ulcers, erosive esophagitis, reflux esophagitis, Zollinger-Ellison syndrome, bleeding from the upper gastrointestinal tract (iv), prevention of erosive and ulcerative lesions of the gastrointestinal tract while taking NSAIDs and aspiration of gastric contents during general anesthesia.
One of the significant disadvantages of famotidine, common to all H2-blockers, is the effect of tachyphylaxis - the patient’s addiction to the drug, when the effect of the drug noticeably decreases with repeated use.
Famotidine tachyphylaxis.
Intragastric pH during therapy with proton pump inhibitor omeprazole and famotidine (Gostishchev V.K., Evseev M.A.). A decrease in the antisecretory effectiveness of famotidine is clearly visible upon repeated administration . Contraindications.
Hypersensitivity, pregnancy, breastfeeding.
Side effects.
Dry mouth, loss of appetite, nausea, vomiting, abdominal discomfort, increased levels of transaminases in the blood serum, cholestatic jaundice, increased fatigue, tinnitus, headache, rarely hallucinations, fever, arrhythmias, muscle pain, arthralgia, dry skin, allergic reactions: angioedema, itching, urticaria, conjunctivitis, bronchospasm; irritation at the injection site.
Interaction.
When taking famotidine and ketoconazole simultaneously, the absorption of ketoconazole may be reduced. When using famotidine with antacids, the interval between taking them should be at least 1-2 hours.
Overdose
.
- Symptoms: worsening side effects.
- Treatment: gastric lavage, symptomatic or supportive therapy.
Method of administration and dose. Inside
. For exacerbation of gastric and duodenal ulcers, 40 mg at night or 20 mg 2 times a day (morning and evening), course duration - 4-8 weeks; to prevent exacerbations - 20 mg 1 time per day at night for 6 months. For reflux esophagitis - 20 mg 1-2 times/day for 6-12 weeks, Zollinger-Ellison syndrome - 20-40 mg 4 times/day (if necessary, increase the dose of the drug).
Intravenously (stream or drip).
The average dose is 12 mg every 12 hours. For Zollinger-Ellison syndrome: initial dose - 12 mg every 6 hours, subsequently the dose is adjusted; to prevent aspiration of gastric contents before general anesthesia: 20 mg on the day of surgery or at least 2 hours before surgery.
Precautionary measures.
For patients with impaired renal function (creatinine clearance below 30 ml/min), the daily dose is reduced to 20 mg. It is not recommended to prescribe the drug to children. When treating gastric and duodenal ulcers, it is necessary to exclude the presence of a malignant tumor in the patient (examination of a biopsy from the area of the ulcer). Use with caution in case of liver dysfunction.
Use during pregnancy and breastfeeding.
Famotidine is contraindicated for use during pregnancy and lactation. The FDA category of risk for the fetus when used by pregnant women is B (animal studies have not revealed the risk of negative effects on the fetus; there have been no adequate studies in pregnant women).
Famotidine is generally a prescription drug
.
However, drugs containing small doses (10 mg) of famotidine are available over the counter
(Kvamatel mini).
By Decree of the Government of the Russian Federation of December 30, 2009 No. 2135-r, famotidine (lyophilisate for the preparation of a solution for intravenous administration; film-coated tablets; film-coated tablets) is included in the List of vital and essential medicines.
Famotidine and coronavirus.
There are studies indicating a link between proton pump inhibitors and the risk of COVID-19. They indicate the importance of deprescribing proton pump inhibitors in conditions of increased risk of COVID-19. The preferred antisecretory drug is famotidine, which improves the condition of patients infected with SARS-CoV-2. The high therapeutic effectiveness of H2-blockers, in particular famotidine, in such patients is due not only to the mild suppression of acidic gastric secretion, but also to pronounced antioxidant properties (Khomeriki N.M.).
Trade names of drugs with active ingredients
famotidine: Antodin, Blockacid, Gasterogen, Gastrosidin, Kvamatel, Kvamatel mini, Lecedil, Pepsidin, Ulfamid, Ulceran, Famonit, Fampopsin, Famosan, Famotel, Famotidine, Famotidine-ICN, Famotidine-OBL, Famotidine-AKOS, Famotidine-Acri, Famotidine -Apo, Famotidine-STADA, Famocid.
Manufacturer
: Biocom, Stavropol Russia; ZiO-Zdorovye, Russia; Makis-Pharma, Russia; Obolensk Pharmaceutical Enterprise, Russia; Serena Pharma/Shreya Life Sciences, India; Pharmstandard-Leksredstva, Russia; Hemofarm D.D., Yugoslavia; Hemofarm concern A.D., Yugoslavia; Yaka-80, Macedonia.
Brands of famotidine are registered in the USA: prescription (Pepcid, Duexis) and over-the-counter (over-the-counter), characterized by a reduced content of famotidine and intended for the relief of heartburn (Pepcid AC).
In addition to famotidine, Pepcid Complete and Double Action Complete, registered in the United States, contain the antacids calcium magnesium carbonate hydroxide. Tums Double Action has a similar composition, as well as Gastromax, which has Ukrainian registration.
Descriptions of drugs and instructions
from different manufacturers (pdf):
- For Russia
- official instructions of Akrikhin OJSC: “Instructions for medical use of the drug Famotidine-Akri”, film-coated tablets, 20 mg, dated September 17, 2008.
- “Information about the drugs Kvamatel and Kvamatel mini for medical workers and specialists”, film-coated tablets, 10 mg (Kvamatel mini) and 20 and 40 mg (Kvamatel), lyophilisate for the preparation of a solution for intravenous administration (Kvamatel) Gedeon Richter
- “Instructions for medical use of the drug Famotidine”, tablets, 20 mg, OJSC “Kievmedpreparat”
Materials for healthcare professionals regarding the use of famotidine in the treatment of diseases of the gastrointestinal tract
Articles and reports
- Khomeriki N.M. Features of the treatment of acid-related diseases during the COVID-19 pandemic. Therapeutic archive. T.93, 2.2021. Application. P.55-56.
- Chernov Yu.N., Batishcheva G.A., Alekhin S.M., Zorina M.S. Daily monitoring of intragastric pH in patients with duodenal ulcer and comparative effectiveness of the antisecretory effect of quamatel with various methods of administration // Applied information aspects of medicine. 2015. T. 18, No. 5.
- Dorofeev A.E., Afanasyev M.V. The use of famotidine in patients with gastroesophageal reflux disease in combination with functional dyspepsia // Medical newspaper “Health of Ukraine”. – 2008. – No. 6/1. - With. 33.
- Minushkin O.N., Maslovsky L.V. Report on clinical trials of the drug famocid (India) at the Department of Gastroenterology of the Educational and Scientific Center of the Medical Center of the Administration of the President of the Russian Federation.
- Zatevakhin I.I., Shchegolev A.A., Titkov B.E. Famotidine in the treatment of surgical patients with acid-dependent diseases of the stomach and duodenum // Russian Journal of Gastroenterology, Hepatology, Coloproctology. – 1999. – No. 4. - With. 84–87.
- Deineko N.F., Shargorod I.I., Garsali R.B. Famotidine in the treatment of patients with chronic recurrent pancreatitis // Pharmacist. – 1999. – No. 15.
- Okhlobystin A.V. The use of famotidine for the treatment of acute ulcer bleeding // Russian Medical Journal. – 2002. – T. 10. – No. 8–9.
On the website GastroScan.ru in the “Literature” section there is a subsection “H2-blockers” containing articles devoted to the treatment of diseases of the gastrointestinal tract using H2-blockers of histamine receptors, including the use of famotidine.
Video
Still from video Vovk E.I.
Medicines for the treatment of heartburn and diseases associated with hyperacidity. Clinical pharmacology On the website GastroScan.ru in the “Video” section there is a subsection for patients “Popular Gastroenterology” and subsections “For doctors” and “For medical students and residents”, containing video recordings of reports, lectures, webinars in various areas of gastroenterology for healthcare professionals and medical students.
Famotidine has contraindications, side effects and application features; consultation with a specialist is necessary. Back to section
How to use Famotidine: instructions
The medication in tablets is taken 1-2 times a day:
- 1 tablet 20 or 40 mg once: to reduce the acidity of gastric juice, to prevent relapses of gastric diseases, for reflux esophagitis;
- 20–40 mg up to 4 times a day: for Zollinger-Ellison syndrome and the risk of internal bleeding;
- 20 mg - 2 hours before surgery.
The maximum daily dose of the drug is 160 mg. The duration of treatment is 4–8 weeks. The exact treatment regimen depends on the type of disease and is adjusted by the doctor. The tablets should be taken before or after meals, without chewing, with water at room temperature. If necessary, the drug can be taken before bedtime.
Before administration, the lyophilisate is diluted in saline solution: 5–10 ml of sodium chloride 0.9%. Injections are given intravenously:
- 20 mg once: before surgery;
- repeating injections every 12 hours: for diseases of the digestive system, internal bleeding.
It is necessary to reduce the dosage of the drug gradually to avoid a possible reactive increase in the synthesis of hydrochloric acid. During the treatment period, it is important to follow a special diet: exclude foods that stimulate the secretion of gastric juice.
Buy Famotidine Hemofarm film-coated tablets 40 mg No. 20 in pharmacies
Active ingredients Famotidine
Latin name Famotidine
Release form Film-coated tablets
Pharmacological action Famotidine has an antiulcer effect. III generation H2-histamine receptor blocker. Suppresses basal and histamine, gastrin and acetylcholine-stimulated production of hydrochloric acid. Reduces pepsin activity. Strengthens the protective mechanisms of the gastric mucosa, promotes the healing of damage associated with the effects of hydrochloric acid (including scarring of stress ulcers) and the cessation of gastrointestinal bleeding by increasing the formation of gastric mucus, the content of glycoproteins in it, stimulating the secretion of bicarbonate by the gastric mucosa, endogenous synthesis of prostaglandins in it and the rate of regeneration. Does not significantly change plasma gastrin levels. Weakly inhibits the cytochrome P450 oxidase system in the liver. After oral administration, the effect begins within 1 hour and reaches a maximum within 3 hours. The duration of action of the drug after a single dose depends on the dose and ranges from 12 to 24 hours.
Pharmacokinetics After oral administration, it is quickly absorbed from the gastrointestinal tract, the maximum concentration in the blood plasma is reached within 1-3.5 hours. Bioavailability is 40-45%, increases when taken with food and decreases when taking antacids. Bonding with plasma proteins is 15-20%. 30-35% of famotidine is metabolized in the liver (to form S-oxide). Penetrates into the cerebrospinal fluid, through the placental barrier, and is excreted in breast milk. Elimination mainly occurs through the kidneys: 27-40% of the drug is excreted unchanged in the urine. The half-life is 2.5-4 hours, in patients with creatinine clearance below 30 ml per minute it increases to 10-12 hours. In patients with severe renal failure (creatinine clearance below 10 ml/min), the half-life increases to 20 hours.
Indications Peptic ulcer of the stomach and duodenum (including prevention of exacerbations); symptomatic ulcers, erosive and reflux esophagitis; Zollinger-Ellison syndrome.
Contraindications Hypersensitivity, pregnancy, lactation.
Use during pregnancy and breastfeeding Contraindicated.
Special instructions Before treatment, it is necessary to exclude the presence of a malignant process in the gastrointestinal tract.
Composition 1 tablet contains: Active substance: famotidine 40 mg; Excipients: corn starch, microcrystalline cellulose, silicon dioxide, talc, magnesium stearate, croscarmellose sodium; Shell composition: hypromellose, macrogol 6000, titanium dioxide (E171), talc, brown iron oxide dye.
Method of administration and dosage: Orally, swallow whole (without chewing), with a sufficient amount of water. For gastric and duodenal ulcers in the acute phase, symptomatic ulcers, erosive gastroduodenitis - usually 20 mg 2 times a day or 40 mg 1 time a day at night. If necessary, the daily dose can be increased to 80–160 mg. The course of treatment is 4–8 weeks. For dyspepsia associated with increased secretory function of the stomach - 20 mg 1-2 times a day. To prevent recurrence of peptic ulcer - 20 mg 1 time per day before bedtime. For reflux esophagitis - 20-40 mg 2 times a day for 6-12 weeks. For Zollinger-Ellison syndrome, the dose of the drug and the duration of treatment are determined individually. The initial dose is usually 20 mg every 6 hours and can be increased to 160 mg every 6 hours. To prevent aspiration of gastric juice during general anesthesia, 40 mg in the evening and/or morning before surgery. In case of renal failure (with creatinine Cl <30>3 mg/100 ml), the daily dose of the drug should be reduced to 20 mg.
Side effects Rarely - headache, dizziness, fatigue, dry mouth, lack of appetite, diarrhea or constipation, skin rash.
Drug interactions Antacids interfere with absorption (a break of at least 1–2 hours between taking antacids and famotidine is recommended).
Overdose Symptoms: possible worsening side effects. Treatment: gastric lavage, symptomatic therapy.
Storage conditions Store at a temperature of 15 to 25° C.
Shelf life: 3 years.
The appearance of the product may differ from the product shown in the photo.
Side effects
According to the instructions for Famotidine, the following are possible with its use:
- reactions from the digestive system: dry mouth, loss of appetite, nausea, feeling of fullness in the stomach;
- from the central nervous system: tinnitus, dizziness, decreased vision, tremor;
- from the genitourinary system: delayed diuresis, disruption of the menstrual cycle, decreased libido;
- from the heart and blood vessels: changes in heart rate, bradycardia, decreased blood pressure.
In case of overdose, vascular collapse, vomiting, loss of coordination, confusion, acute pancreatitis, drug-induced hepatitis, bronchospasm, and myalgia are likely.