Eosinophilic diseases occur when eosinophil levels are above 450 in different parts of the body. When the body is attacked by substances that cause allergies (through the digestive or respiratory organs). This group of diseases is based on increased formation of eosinophils. Eosinophils are specialized cells of the immune system. They form exclusively in the bone marrow, where they remain for about eight days, undergoing a maturation process before moving into the blood vessels. These cells move through the blood vessels for approximately eight to 12 hours until they reach their target tissues of the spleen, lymph nodes, thymus gland and submucosal areas of the gastrointestinal, respiratory and genitourinary tracts. There they remain for one to two weeks.
The normal number of eosinophils per cubic millimeter of blood is from 0 to 450. Eosinophilic diseases occur when eosinophil levels are above 450 in different parts of the body. When the body is attacked by substances that cause allergies (through the digestive or respiratory organs), eosinophils move to the part of the body that is threatened and release certain toxins. However, when the body produces an excess of eosinophils, they cause chronic tissue inflammation, leading to tissue destruction. Eosinophilic diseases are diagnosed by the location of elevated levels of eosinophils: eosinophilic esophagitis (esophagus), eosinophilic gastritis (stomach), eosinophilic gastroenteritis (stomach and small intestine), eosinophilic enteritis (small intestine), eosinophilic colitis (colon), hypereosinophilic syndrome (blood and any organ).
Elevated levels of eosinophils in the blood or other organs characterize many disorders, from allergic diseases to endocrine disorders.
I will try to describe a typical baby with allergic proctocolitis.
Usually this is a well-developed, well-fed baby with excellent health, in whom, from the age of 2-3 months, parents began to notice a slight increase in stool (may or not) and streaks of scarlet blood in the stool.
Often there is also a lot of mucus in the stool.
Typically, with typical proctocolitis there is no obvious colic, but there may be restlessness when passing stool
Allergic proctocolitis can develop both in a breastfed and artificially fed child.
In a general stool analysis, you can find a large number of leukocytes in the stool (although this sign is nonspecific), and there may be a completely normal analysis.
In a general blood test, hemoglobin may be slightly reduced and the number of eosinophils may be increased, but everything may be fine.
It is with this picture that one should think about allergic proctocolitis.
Which allergen to exclude?
The most common allergen is cow's milk protein.
Cow's milk is the basis for the preparation of standard milk formulas for babies, but dairy products can also be present in the diet of a nursing mother, later penetrating into breast milk.
By the way: Back in 1921 (almost a hundred years ago!) the possibility of allergens from the mother’s diet entering breast milk was proven.
There are about 25 different allergen proteins in cow's milk, some of which are found in the milk of other animals - goats, sheep, and so on.
The most significant allergens are beta-lactoglobulin and casein.
Therefore, to check the breastfeeding of children, the mother switches to a dairy-free diet, and bottle-fed children are transferred to a special formula, where milk protein is broken down to the smallest fragments (deep hydrolysates) or absent (a solution of amino acids instead).
Amino acid mixtures are the most non-allergenic and safe even for severe allergy sufferers, but are much more expensive than hydrolysates.
During the trial diet, mothers often exclude beef/veal for a while - 10% of children have a chance of cross-allergy.
What to do if a trial diet excluding cow's milk protein does not work?
- if the child is breastfed, reconsider the mother’s diet (what if hidden milk protein still appears) or try to exclude other, rarer allergens - soy, chicken eggs, wheat
- if the child is on hydrolyzate, switch to an amino acid mixture
Please note - soy is also a common allergen in itself (up to 0.5% of the population), and in people with an existing allergy to milk protein, the frequency of cross-allergy to soy is from 15% to 50%.
We also take into account other reasons for the periodic appearance of blood in the stool:
- Dermatitis around the anus
- Fissure of the anus - usually in the presence of dense stool in a baby, usually on artificial feeding. A visible fissure in the anus in the presence of soft stool does not exclude allergic proctocolitis.
- Infections. Usually, if a child has such classic intestinal infections as salmonellosis or dysentery, the child has obvious signs of intoxication, and with campylobacteriosis, the baby’s well-being may be relatively good.
- Blood clotting disorders (very rare, usually there are other manifestations of bleeding)
Eosinophilic gastroenteritis. Treatment
Treatment of patients with eosinophilic gastroenteritis is very difficult, it is carried out individually with adherence to antiallergic nutrition and nutrition recommended for chronic enteritis, the use of hormonal therapy with a gradual reduction in the dose of glucocorticoids (according to the scheme) for a long time, the use of drugs in accordance with the clinical manifestations of the disease.
In the future, patients with an established diagnosis of eosinophilic gastroenteritis should be under the supervision of a gastroenterologist with consultations of allergists, pulmonologists and other specialists.
Eosinophilic gastroenteritis is a serious disease that can cause complications that are life-threatening for the patient.
Eosinophilic gastroenteritis is a difficult and rarely diagnosed disease and requires doctors of various specialties to conduct an in-depth examination of the patient, taking into account possible concomitant pathologies (gastrointestinal tract, bronchial asthma, allergies, food allergies).
What if the complaints disappeared during the diet, but doubts remained?
It is possible to reintroduce the allergen protein: the previous complaints have reappeared - doubts have been resolved.
Important: this should not be done in case of acute and severe allergic conditions; anaphylactic shock is possible!
But proctocolitis is not an acute, not serious condition, so the experiment is possible.
The prognosis for non-IgE conditions is usually good.
Complaints will disappear even if you do nothing at all... but it’s better not to do that!
Often, when discussing complaints from a baby, parents remember that older children also had blood in the stool in the first months of life, but then disappeared on their own. With hindsight we understand that most likely they also had allergic proctocolitis.
In most children with proctocolitis, complaints disappear before the age of one year, with FPE between the ages of 1 and 3 years, with FPIES between the ages of 1 and 5 years.
Very rarely, allergic proctocolitis persists into older age or occurs for the first time in older children or adults.
In these cases, it is very difficult to exclude a certain trigger food product; drug treatment is often required - corticosteroids, aminosalicylates. The range of conditions for a differential diagnosis by a doctor is also different.
9, total, today
Clinical observation
Patient S., 17 years old, resident of the Republic of Kazakhstan, was hospitalized at the clinic of the European Medical Center on February 27, 2020 with complaints of decreased appetite, general weakness, vomiting of eaten food up to 3 times a day, unformed stools up to 7 times a day.
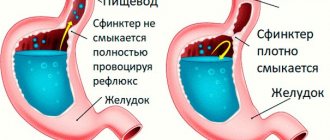
He has not been seen by doctors before and denies allergic reactions. In January 2022, for the first time, against the background of complete well-being, vomiting of eaten food occurred, which did not bring relief, diarrhea up to 10–12 times a day, spasmodic abdominal pain, mainly in the epigastrium. Body temperature did not increase. The patient was examined at the place of residence, esophagogastroduodenoscopy (EGD) was performed, which revealed signs of reflux esophagitis of the 1st degree, a picture of catarrhal gastritis, bulbitis, and ulcers of the antrum of the stomach. The urease test is positive. Treatment was carried out: amoxicillin 1 g 2 times / day, clarithromycin 500 mg 2 times / day, tripotassium bismuth dicitrate 240 mg 2 times / day, omeprazole 20 mg / day for 14 days. During therapy, positive dynamics were noted: vomiting and diarrhea stopped. The deterioration of the condition occurred in July 2022, when the above symptoms returned.
During an examination on July 20, 2019, a clinical blood test revealed leukocytosis of 12×109/l and eosinophilia of up to 24.9% for the first time. IgG antibodies to Giardia were detected. No antibodies to helminths were detected. The patient was treated with nifuratel 400 mg 2 times a day for 7 days, during which vomiting and diarrhea stopped again.
In February 2022, a resumption of symptoms was noted. When examined on February 13, 2020, a clinical blood test showed leukocytosis 15.3×109/l with eosinophilia 44.2% (absolute number - 6.77×109/l). These and subsequent laboratory data are presented in Table 1. Hospitalized in the hospital of the European Medical Center on February 27, 2020.
Upon admission, upon examination, it was noted that the abdomen was slightly painful in the epigastrium; otherwise, the physical examination findings were unremarkable. Clinical blood test dated February 27, 2020: leukocytosis 49.8×109/l, eosinophilia 82.7%, ESR 5 mm/h. Levels of mannan antigen and antimannan antibodies (signs of invasive candidiasis) are within reference values. There was an increase in the level of C-reactive protein (CRP) to 83.6 mg/l, IgE - to 352 (normal - up to 87 IU/ml). Therapy was prescribed: ketotifen 1 mg 2 times a day, omeprazole.
On computed tomography of the abdominal cavity with intravenous contrast, the walls of the lower third of the esophagus are uniformly thickened circularly to 0.9 cm, and there is gas in the lumen of the esophagus (Fig. 1A). Uniform circular thickening of the walls of the antrum of the stomach up to 1.1 cm (Fig. 1B). The walls of the small intestine and proximal colon are uniformly thickened circularly up to 1.1 cm, with early contrast of the inner layer (Fig. 1B, 1C). A positive halo sign is noted (Figure 1D). The fatty tissue of the abdominal cavity is compacted due to edema. There is a small amount of effusion in the abdominal cavity - along the lateral canals and in the pelvic cavity. Lymph nodes are not enlarged.
According to endoscopy and colonoscopy, esophageal candidiasis, focal esophagitis, severe diffuse gastritis, erosion in the antrum of the stomach, ulcer of the antrum in the subacute phase, diffuse erosive bulbitis and duodenitis were revealed; lymphofollicular hyperplasia of the mucous membrane of the terminal ileum against the background of erosive terminal ileitis, focal erosive typhlitis, diffuse colitis with single erosions (Fig. 2).
According to histological examination in biopsy specimens of the lamina propria of the small intestine
— moderately expressed lymphoplasmacytic, eosinophilic-cellular infiltration, with mild atrophy, focal lymphoid hyperplasia, without dysplasia (Fig. 3A);
in biopsy samples of the lamina propria of the mucous membrane of the colon
, with the adjacent lamina of the mucous membrane - moderately pronounced lymphoplasmacytic and eosinophilic cell infiltration, with mild atrophy, focal lymphoid hyperplasia;
in a biopsy of the lamina propria of the mucous membrane of the antrum of the stomach
there is moderately pronounced lymphoplasmacytic and eosinophilic cell infiltration, with focal lymphoid hyperplasia, severe atrophy (Fig. 3B);
in a biopsy of the mucous membrane of the esophagus
, lined with stratified squamous epithelium, without atypia, with an adjacent muscular layer, moderately pronounced lymphoplasmacytic and eosinophilic cell infiltration was noted throughout the fragment.
The patient was diagnosed with Eosinophilic esophagitis. Eosinophilic gastroduodenitis. Eosinophilic colitis. Candidiasis of the esophagus. Ascites. Chronic stomach ulcer. A diet that eliminates soy, wheat, eggs, milk, peanuts, nuts, fish, and shellfish is recommended. Therapy was started: ketotifen 1 mg 3 times / day, fexofenadine 180 mg 1 time / day, famotidine 20 mg 2 times / day before meals, bismuth tripotassium dicitrate 120 mg 3 times / day before meals for 10 days, fluconazole 200 mg intravenous drip 1 time /day 7 days.
During therapy, positive dynamics were noted: abdominal pain completely regressed, stool returned to normal, there was no vomiting, leukocytosis and eosinophilia with a downward trend as of 03/05/2020 (Table 1).
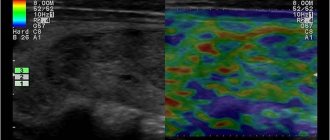
However, despite the clinical improvement and subsidence of gastrointestinal symptoms, on 03/06/2020 the patient developed an episode of fever up to 38 °C, without chills, visible swelling of the left cervical region, an increase in the level of CRP to 174 mg/l was noted, the level of procalcitonin was 0 .06 ng/ml (normal is less than 0.1 ng/ml). During physical examination, a painful soft elastic node of supraclavicular localization was palpated. According to ultrasound data, against the background of pronounced swelling of the soft tissues of the supraclavicular region and neck on the left, multiple lymph nodes of a hypoechoic heterogeneous structure from 5×4 mm to 11×18 mm were located, signs of organized occlusive thrombosis of the distal segment of the internal jugular and subclavian vein with transition to the brachiocephalic vein on the left with periphlebitis.
The condition was assessed as lymphadenitis, complicated by regional phlebitis. Enoxaparin 60 mg subcutaneously every 12 hours and ceftriaxone 1 g 2 times a day were added to the treatment. During therapy, neck swelling regressed, temperature returned to normal, and CRP decreased to normal.
However, as the symptoms of lymphadenitis subsided on 03/08/2020, an increase in leukocytosis and the absolute number of eosinophils was again noted (20.1×109/l and 15.1×109/l, respectively). The proportion of eosinophils was 74.7%. Therapy with methylprednisolone 16 mg/day orally was started.
After 2 days (03/10/2020), the number of leukocytes decreased to normal (5.32×109/l, eosinophilia completely regressed - 0.3×109/l (5.7%). The patient was discharged for outpatient treatment with a recommendation for subsequent gradual reducing the dose of methylprednisolone (by 2 mg/day every week).
At the outpatient stage of treatment, pronounced positive dynamics remained: abdominal pain completely stopped, stools formed once a day, brown in color, stable normothermia. Thrombosis of the internal jugular vein with signs of recanalization. A clinical blood test revealed moderate leukocytosis without eosinophilia (see Table 1).