What it is
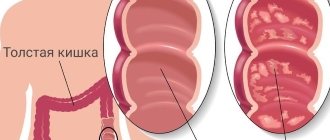
Chronic intestinal colitis is an inflammatory process that affects the mucous membrane and submucosal layer of this organ. The disorder is equally common in both women and men, but in the latter it manifests itself at a later age.
The chronic form of colitis involves phases of exacerbation and remission phases, when there are no signs. Symptoms with this form are less pronounced than with acute colitis. The pathology is diagnosed simply and treated comprehensively.
Risk factors
Risk factors for the occurrence of colitis are as follows:
- reduced immunity;
- poor nutrition;
- frequent stress;
- alcohol abuse;
- a history of autoimmune diseases;
- abnormal structure of blood vessels in the intestine.
Enteral nutrition for ulcerative colitis
Ulcerative colitis (ICD-10 code K51) is a chronic inflammatory disease of the colon of unknown etiology, characterized by ulcerative-necrotic changes in the mucous membrane and a continuous inflammatory process.
The peak incidence of ulcerative colitis occurs at a young age, the prevalence of the disease is about 40 cases per 100 thousand population.
The disease can affect the entire colon - total colitis (18% of cases), left-sided lesions occur in 28% of cases and proctosigmoiditis occurs in 54% of cases.
The main symptoms of ulcerative colitis include primarily intestinal bleeding and constant loss of blood in the stool, diarrhea and abdominal pain. Extraintestinal manifestations of the disease are also common - fever, arthralgia, erythema nodosum, changes in the visual organs, and the development of anemia is typical.
The severity of ulcerative colitis is assessed by stool frequency, degree of blood loss, fever and laboratory parameters (ESR, albumin level).
For ulcerative colitis, various classes of drugs are used in therapy, primarily 5-aminosalicylic acid drugs (mesalazine, sulfasalazine), systemic and topical glucocorticoids (prednisolone, budesonide), immunosuppressants (azathioprine). Treatment tactics depend both on the severity of the disease and on the extent of damage to the large intestine.
Nutrition for patients with ulcerative colitis
Nutrition for patients suffering from ulcerative colitis presents significant difficulties for both the doctor and the patient. There is no clear formula for dietary nutrition for this disease. Patients are advised to avoid spicy, fatty, fried foods, give up rough foods, eat vegetables and fruits, limit simple carbohydrates and fats in their diet and focus on the protein component of the diet.
In practice, it can be difficult for patients to adhere to dietary recommendations, which is especially typical at the onset of the disease, when the patient has to reconsider most of his food preferences and permanently give up a number of favorite foods. Over time, each patient is forced to carefully expand his diet and introduce new foods into it, and this is often done by trial and error, often provoking an exacerbation of the disease. Over time, the patient develops his own diet and, provided he regularly takes the prescribed medications, does not experience any serious inconveniences associated with the disease, and his quality of life remains at a fairly high level.
Types of malnutrition in ulcerative colitis
Malnutrition is common both during exacerbation of ulcerative colitis and during remission. Loss of body weight is observed in more than half of the patients, hypoalbuminemia occurs in 25–50% of cases, anemia in 66% of patients, the vast majority have iron deficiency, there is clear evidence of insufficiency in this group of patients of folic acid, cyanocobalamin, calcium, magnesium, potassium, vitamin D, copper and zinc.
The main types of malnutrition that occur in ulcerative colitis are:
- depletion of muscle protein and fat reserves while maintaining the visceral protein pool (marasmus, ICD-10 code E41);
- depletion of the visceral protein pool while maintaining fat reserves and muscle protein, while body weight can remain normal (kwashiorkor, code E40 according to ICD-10);
- depletion of both visceral and somatic protein reserves (mixed type of malnutrition - marasmic kwashiorkor, code E42 according to ICD-10).
Depletion of both the visceral and somatic pools of protein occurs, as a rule, with severe exacerbations that cannot be stopped for a long time.
Causes of malnutrition in patients with ulcerative colitis
There are several causes of malnutrition in ulcerative colitis. First of all, in patients, together with discharged mucus and as a result of bleeding, there is a large loss of proteins, electrolytes and microelements in the stool, especially pronounced with repeated non-fecal bloody and mucous stools, and this leads to a decrease in the amount of transport albumin, which leads to disruption of the delivery of nutrients to tissues. On the other hand, acute and chronic inflammation leads to a change in metabolism towards catabolism and, as a result, increases the body's needs for energy and building material. At the same time, quite often in this category of patients there is a sharp decrease in appetite, up to anorexia. Patients often deliberately limit the amount of food they eat, since an increase in the amount of content in the large intestine causes increased pain. It should also be noted that systemic glucocorticoids used in standard therapy for ulcerative colitis further increase the body's needs for energy and proteins. And the gentle nutrition traditionally used in the clinic is not always able to satisfy all the demands that the body makes.
Result of malnutrition
Malnutrition leads to a decrease in the body's adaptive capabilities and thereby complicates the treatment of the patient and leads to prolongation of the exacerbation of the disease.
This problem is most significant in the surgical treatment of ulcerative colitis, when the body's adaptive capabilities can determine the prognosis and outcome of surgical treatment and greatly affect the patient's condition in the postoperative period.
Malnutrition significantly complicates the treatment of young patients, who need energy and nutrients not only for the functioning of the body, but also for growth and development.
Enteral and parenteral nutrition for ulcerative colitis
Adequate intake of nutrients and energy can be achieved through parenteral and enteral nutrition.
At the same time, the possibility of widespread use of parenteral nutrition is limited by technical difficulties in implementation, the need for careful monitoring of nutritional support, and the high cost of such treatment. In this regard, parenteral nutrition is used, as a rule, in severe exacerbations, when, against the background of moderate or severe malnutrition, there is a need for complete functional rest of the large intestine and the entry of any nutrients into the lumen of the colon should be excluded in order to avoid provoking a deterioration of the condition patient. Parenteral nutrition should also be used when the degree of malnutrition becomes more severe in the absence of the ability to meet the body's needs naturally through the gastrointestinal tract.
The most appropriate way to adequately provide this category of patients with nutrients and energy is nutritional support in the form of enteral nutrition. Enteral nutrition mixtures contain all the necessary macro- and micronutrients and, due to this, can act as the only source of nutrition for a long time.
Nutritional support in the form of enteral nutrition has several important effects. First of all, the functional load on the large intestine is reduced, additional trauma to the inflamed mucosa is reduced and a rest regime is created for the distal parts of the gastrointestinal tract, since the absorption of the components of the mixtures occurs in the small intestine. In contrast to enteral nutrition, the intake of regular food causes the formation of feces, the movement of which in the affected colon leads to additional trauma to the mucous membrane, which contributes to prolonging the exacerbation of the disease. Secondly, food antigens that may contribute to the maintenance of inflammation are removed from the lumen of the digestive tract. It is important to note that enteral nutrition formulas do not contain lactose or gluten, which cause diarrhea.
Thus, when using enteral nutrition, two main tasks are solved: it ensures the replenishment of the energy and plastic needs of the body, as well as a rest regime for the large intestine, which helps reduce the inflammatory process.
But, despite the advantages of using enteral nutrition, at present there is not yet a sufficient evidence base regarding the effect of enteral nutrition on the course of the inflammatory process in ulcerative colitis. Recent guidelines from the European Society for Parenteral and Enteral Nutrition (ESPEN) recommend the use of enteral nutrition in ulcerative colitis if the patient is nutritionally deficient.
There are two ways to use enteral nutrition formulas. Firstly, they can serve as an additional source of nutrition and be used in addition to the diet being used. Secondly, they can act as the main source of nutrition in patients with severe exacerbation of ulcerative colitis.
Enteral nutrition is divided into oral and tube feeding. In the case of oral nutrition, the sip feeding method is recommended, when the patient takes the prescribed volume of the mixture in small sips throughout the day.
There is a wide range of enteral nutrition formulas available that can be used to provide nutritional support to patients with ulcerative colitis. The choice of a particular mixture can be determined both by the characteristics of its composition and by the economic capabilities and taste preferences of the patient himself, which also plays an important role. The mixtures most often used in clinical practice are “Clinutren”, “Nutrizon”, “Nutricomp standard”, “Nutrien standard”, “MD mil Clinipit” and others.
Both balanced and semi-element mixtures can be used. In the complex therapy of nutritional deficiency in ulcerative colitis, the semi-element mixture “Peptamen” has proven itself well. The advantage of this mixture is that the proteins in its composition are broken down into peptides, are easily digested and absorbed in the upper parts of the small intestine, and fats are medium-chain (50–80%) and are digested without lipase.
Some mixtures contain dietary fiber, which makes it possible to correct dysbiotic changes that always occur with ulcerative colitis (Nutricomp Fiber).
In most cases, enteral nutrition formulas should not replace the patient’s overall diet, but should serve as an additional source of nutrients and energy. According to the latest ESPEN recommendations, those patients with ulcerative colitis who have nutritional deficiency are advised to receive additional enteral nutrition with an energy value of 500–600 kcal per day.
In practice, it is possible to quickly teach the patient how to prepare the mixture and how to take it. The sipping method, when the patient consumes the formula, is the most effective, since it first of all helps to avoid diarrhea, a fairly common complication of enteral nutrition. For the same purpose, it is advisable to gradually introduce the mixture into the patient’s diet in such a way that the required energy value of 500–600 kcal per day is achieved within several days.
Enteral nutrition as a “drug”
Enteral nutrition can act not only as a source of nutrients and energy, but also as a therapeutic option. For this purpose, the enteral nutrition mixture “Modulen IBD” is used, specially developed for the treatment of inflammatory bowel diseases.
“Modulen IBD” is a dry, complete, balanced mixture based on casein; it contains proteins, fats and carbohydrates in an optimal ratio, as well as all the necessary vitamins, macro- and microelements.
A feature of this mixture, due to which its therapeutic properties are realized, is the presence in its composition of a natural anti-inflammatory growth factor (TGF-beta2). The anti-inflammatory activity of this factor is realized by reducing the level of pro-inflammatory cytokines in the intestinal mucosa - primarily interleukin-1, interleukin-8 and interferon gamma.
Modulen IBD has demonstrated high effectiveness in the treatment of Crohn's disease and is used in pediatric practice as a monotherapy for this disease. In accordance with the ECCO statement 10B of the European Consensus on the Diagnosis and Treatment of Crohn's Disease adopted by the European Association of Crohn's and Colitis, this enteral nutrition in Crohn's disease is effective in achieving remission, regardless of the activity of the process and the location of the lesion.
While the effectiveness of using Modulen IBD in the treatment of Crohn's disease has been studied quite well, the effectiveness of this mixture in the treatment of ulcerative colitis has not yet been sufficiently studied. Our clinic has experience using the Modulen IBD mixture in the complex treatment of patients with ulcerative colitis and is currently conducting a pilot study of the effectiveness of Modulen IBD in patients with moderate forms of the disease.
According to preliminary data, the period of relief of exacerbation when using this mixture is shorter than with standard therapy, which indicates the influence of therapy with the Modulen IBD mixture on the course of the inflammatory process. There is a positive dynamics in body weight and indicators of the nutritional status of patients: an increase in the total thickness of skin-fat folds, albumin levels, and the absolute number of lymphocytes. In the case where patients lost weight quickly enough during the last weeks, the use of the mixture significantly reduced the rate of progression of malnutrition, and in the future, after the disease went into remission, there was a tendency to increase body weight. Additional enteral nutrition with the Modulen IBD mixture was well tolerated by patients; some patients experienced flatulence, which was quickly eliminated by adjusting the volume of the mixture taken.
Thus, the use of Modulen IBD in the treatment of patients with ulcerative colitis allows us to solve three problems:
- ensure adequate energy supply;
- replenish nutrient deficiencies;
- reduce inflammation in the intestinal mucosa.
To summarize, it should be said that, despite the fact that at present there is no strict evidence base showing a decrease in inflammation in the colon through enteral nutrition, the feasibility of its widespread use in the complex treatment of ulcerative colitis is obvious. Currently, Modulen IBD is one of the most promising mixtures for nutritional support of patients with ulcerative colitis.
For questions regarding literature, please contact the editor.
E. I. Tkachenko , Doctor of Medical Sciences, Professor S. V. Ivanov T. N. Zhigalova , Candidate of Medical Sciences, Associate Professor S. I. Sitkin , Candidate of Medical Sciences, Associate Professor of St. Petersburg State Medical Academy named after. I. I. Mechnikova , St. Petersburg
Causes
According to statistics, when visiting a gastroenterologist, 40% of patients are diagnosed with a chronic form of the disease. In approximately 30% of patients, intestinal inflammation is a consequence of intestinal infections (dysentery, salmonellosis). Less commonly, the reason is long-term treatment with antibiotics, which disrupt the normal balance of intestinal microflora.
Causes may also be related to alcohol abuse and poor diet, which contribute to inflammation. In some cases, chronic colitis is a complication of other gastrointestinal diseases, such as chronic gastritis , hepatitis, pancreatitis, as well as a consequence of abnormalities in the development or functional insufficiency of the intestine.
Prevention of enterocolitis
Photo: alluneed / freepik.com
Basic hygiene rules will help prevent intestinal infections:
- washing hands thoroughly after using the toilet and before eating;
- eating only washed vegetables and fruits;
- personal set of dishes and towels for the patient;
- do not visit cafes, restaurants and canteens with questionable levels of hygiene;
- Drink water only from proven sources.
Prevention methods have not been developed for inflammatory bowel diseases, necrotizing and pseudomembranous enterocolitis.
Forms of chronic colitis
The disease comes in several types:
- Spastic. It manifests itself as severe pain that occurs in various parts of the intestine, so the dislocation of pain sensations changes.
- Nonspecific ulcerative colitis. This disease is characterized by the spread of pain throughout the intestines. Ulcers and bleeding are also possible.
Depending on the cause, chronic colitis can be allergic, infectious, ischemic, radiation, toxic, or combined. In the latter case, several etiological factors are combined.
According to the prevalence of the lesion, colitis is:
- segmental - when only a specific part of the intestine is involved in the pathological process;
- total - the entire colon is affected.
By severity:
- mild degree - when it is easy to achieve remission;
- moderate severity - to ensure long-term relief of symptoms, medications and diet are needed;
- severe degree - exacerbation prevails over remission, and it is difficult to achieve the latter.
Variants of localization of the inflammatory process in chronic colitis.
Symptoms
Since in a chronic course the phase of retreat of symptoms and exacerbation alternate, most often patients turn to the doctor precisely when the symptoms acutely make themselves felt. During remission, they are absent altogether or are expressed very weakly.
The main symptoms of chronic colitis are as follows:
- pain that manifests itself in the lateral parts of the abdomen (the nature of the pain can be either acute or aching);
Manifestations of chronic colitis. - rumbling in the intestines;
- belching, often with an unpleasant odor;
- measuring the abdomen in size;
- increased gas formation;
- false urge to defecate, which can occur every few days;
- nausea and weakness;
- unpleasant taste in the mouth;
- increased fatigue;
- sleep disorder;
- pale skin;
- brittle nails and hair loss;
- change in eating habits.
With nonspecific ulcerative colitis, the following symptoms are possible:
- impurities of pus or blood in the stool;
- frequent diarrhea;
- mild tingling pain in the lower abdomen;
- loss of appetite;
- inflammation of the organs of vision (extremely rare);
- pain in the joints;
- muscle weakness.
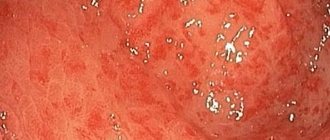
With an exacerbation of the symptoms of this form, changes in the intestinal mucosa are possible, such as swelling, bleeding, the appearance of small ulcers and formations similar to polyps.
Chronic colitis of a spastic nature manifests itself as follows:
- painful spasms that worsen with hunger or at night;
- bloating;
- flatulence;
- alternating diarrhea and constipation;
- insomnia and, as a result, constant fatigue;
- headache of varying intensity;
- complete bowel movement is often possible only the second or third time, and the process of excreting feces occurs only once a few days;
- rumbling in the stomach.
To reduce the symptoms, a constant diet is needed, but it must be taken into account that certain foods can cause constipation.
Symptoms and signs of enterocolitis in children
The main difference in the course of enterocolitis in adults and children is the severity of the disease. Babies under one year old become dehydrated very quickly due to severe loss of fluid and electrolytes with vomiting and diarrhea. Severe dehydration can very quickly lead to shock, coma or death. Diseases associated with diarrhea and vomiting are among the leading causes of death among young children.
How can you tell if your child is severely dehydrated?
- he is irritable, capricious, but at the same time weak;
- dry mouth;
- urination is not profuse.
Symptoms that indicate severe, life-threatening dehydration that requires emergency medical attention include:
- drowsiness;
- dry or slightly wet diaper throughout the day;
- cold hands and feet;
- sunken fontanel;
- fast shallow breathing.
With necrotic enteritis the most typical are:
- swollen, red, painful tummy;
- poor appetite;
- constipation or diarrhea with black/bloody stool;
- low or unstable temperature;
- rarely – vomiting of green contents.
Diagnostics
To diagnose chronic colitis, you will need to consult a therapist and gastroenterologist. Its measures are as follows:
Results of irrigoscopy. conversation with the patient, during which he must talk about all the symptoms he has;- examination of the patient: palpation of the abdomen and eye examination. In the presence of inflammation of the latter, diagnosis is also carried out by an ophthalmologist;
- blood test (acute and biochemical);
- immunological analysis;
- stool analysis;
- colonoscopy (helps distinguish exacerbation from remission);
- X-ray using a contrast agent;
- Ultrasound.
Treatment of chronic colitis
Treatment for chronic colitis differs depending on the phase of the disease. At the remission stage, following a diet is sufficient; in case of exacerbation, drug therapy is needed. Treatment should be individualized, taking into account the type of disorder, severity of symptoms and general condition of the patient
Drug treatment
Typically, the following groups of medications are used for chronic colitis:
Antibacterial therapy and abuse of laxatives can lead to exacerbation of chronic colitis. Antibiotics;- probiotics - aimed at restoring the number of beneficial microorganisms in the intestinal microflora;
- antispasmodics - reduce pain;
- laxatives or fastening agents depending on the symptoms (diarrhea or constipation);
- medications containing enzymes;
- corticosteroids, immunosuppressants (for nonspecific ulcerative colitis);
- enveloping medications and sedatives (for spastic colitis).
Non-drug treatments
Among non-drug methods for chronic colitis, sanatorium-resort treatment may be indicated. Mineral waters, baths, microenemas, and intestinal lavage are useful.
Sometimes doctors recommend courses of physiotherapeutic procedures, such as magnetic therapy, acupuncture, and mud applications. Surgical intervention may be required if there are urgent indications in case of complicated colitis.
Some folk recipes can also be used:
- A decoction of sage, St. John's wort, caraway, and mint helps to cope with inflammation.
- For increased gas formation, mint, motherwort, and nettle are useful.
- To eliminate spasms in the intestines, microenemas with a decoction of calendula or chamomile can be performed.
- For ulcerative colitis, a microenema with sea buckthorn oil at night is useful.
Additional treatment methods are carried out in courses. It is recommended to consult a doctor before using them.
Diet for chronic colitis
Therapy will not be effective if the patient does not comply with a special diet. The rules of the diet for chronic colitis are as follows:
- The diet should contain a lot of fiber. It is found in vegetables, cereals, and bread.
- Food should be consumed 4-6 times a day.
- Lean fish and meat are consumed boiled. You can also eat boiled eggs.
- The diet should include many first courses cooked in vegetable broths.
- Seafood is healthy.
- Fruits and vegetables must be peeled.
- Foods that irritate the intestines should be eliminated from the diet. These include dairy and fermented milk products, legumes, spicy and salty foods, nuts, and alcohol.
Nutrition should be high in calories and include a large amount of substances needed by the body: vitamins, proteins, etc.
Diet for colitis is one of the measures included in the complex treatment of the disease
Treatment of acute enterocolitis
Acute enterocolitis is treated differently. Viral diseases rarely require treatment. It is enough to drink plenty of fluids and in most cases, complete recovery occurs within 1-3 days. Bacterial enterocolitis is treated with antibiotics and drinking plenty of fluids. Also, the treatment regimen may include drugs that help relieve unpleasant symptoms: antipyretics, sorbents, antidiarrheals. Hospitalization is indicated only in the most severe cases. For pseudomembranous colitis, therapy begins with stopping the use of antibiotics or other medications that could trigger the development of the disease. Instead, other drugs are prescribed that are effective specifically against clostridia. In severe cases, the patient may need a fecal microbiota transplant - the introduction of diluted stool from a healthy patient during a colonoscopy, using a tube or by swallowing a capsule. This is done in order to restore normal intestinal microflora. Despite its unattractive nature, fecal microbiota transplantation is the most effective and safest treatment option.
Necrotizing enterocolitis requires rapid response. If there is no peritonitis or perforation, conservative therapy is sufficient: intravenous administration of antibiotics, solutions, nutrients. To remove gas, a tube is inserted into the stomach. If drug treatment does not help, surgery is indicated. The surgeon removes the problem area of the intestine. Sometimes surgery is not performed immediately, but after several weeks or months, when the underlying infection has been cured.
Possible complications and consequences
If the disease is not treated, it can cause a number of complications. This mainly concerns ulcerative colitis. The consequences may be as follows:
- Perforation of the ulcer, which often results in peritonitis. In this case, the symptoms will be manifested by severe bloating and tension in the abdominal muscles, high fever, chills, a coating on the tongue, and general weakness.
- Gangrene of the colon and affected areas of the intestine. In this case, you may feel weakness, high temperature, and decreased blood pressure.
- Blood poisoning or spread of infection to other organs.
- Bleeding in the intestines (with chronic ulcerative colitis).
- The appearance of an oncological tumor is also possible.
Video - Chronic intestinal colitis: causes, symptoms, treatment of colitis.
Causes and risk factors for developing ulcerative colitis
The causes of UC are unknown. Most researchers are inclined to think that this is an autoimmune problem. Risk factors identified:
- genetic. Ulcerative colitis often affects people who have blood relatives with the same diagnosis. To be precise, this pattern is observed in 1 out of 4 cases. Also, UC is particularly common among certain ethnic groups (for example, Jews), which also suggests the heritable nature of the disease;
- environmental factors. Most cases are registered among residents of the northern regions of Eastern Europe and America. The prevalence of ulcerative colitis is influenced by air pollution and diet. It has also been noted that in countries with a high level of hygiene, UC is more common;
- taking non-steroidal anti-inflammatory drugs.