Author:
- Nikonov Mikhail Yurievich
3.00 (Votes: 4)
Many of us begin to think about the state of our health only when we hear an alarm bell from it, or even several. This also applies to the liver, the hottest organ of our body, which bears special responsibility for numerous and very important processes occurring in it.
For example, our liver courageously takes on the first “blow” of toxic substances, allergens and other substances that are unsafe for us (including metabolic products), practically transforming them into safer ones and ready for elimination from the body. It also comes with an excess of hormones, vitamins and other elements that are beneficial to us in normal doses.
On the other hand, the liver accumulates reserves of useful substances (for example, glycogen, vitamins and microelements) to regulate carbohydrate metabolism and a large amount of blood (in case of emergency compensation for blood loss). The liver also synthesizes hormones and enzymes, blood plasma proteins, cholesterol and lipids, bile (including the specific pigment bilirubin), without which our body simply could not exist.
During our lives, the liver copes with such a huge amount of work that if the load on it is too great, sooner or later it itself may need our help. Therefore, assessing the condition of our liver and nearby organs in time by undergoing a comprehensive ultrasound of the abdominal organs and kidneys with the adrenal glands means noticing alarming changes and starting the necessary treatment as early as possible!
What is jaundice
First of all, by jaundice we should not mean a specific disease (for example, hepatitis, as many people think), but a whole symptomatic complex that arises as a result of pathological processes in the liver and some organs. Essentially, jaundice is an excess amount of bilirubin in the body, which is externally manifested by the sclera, mucous membranes and skin becoming yellow.
Normally, bilirubin is formed in the liver and spleen from hemoglobin as a result of the breakdown of red blood cells, after which it is converted by the liver into bile and excreted from the body. With jaundice, the normal process of conversion and excretion of bilirubin is disrupted, so it remains almost completely in the blood, slightly excreted through the kidneys and skin.
People with:
- neoplasms in the liver;
- congenital anomalies of the bile ducts;
- pathological processes in the liver and gall bladder;
- the presence of parasitic organisms;
- postoperative complications;
- post-reaction to certain medications.
Types of jaundice
Depending on the reasons that caused jaundice, it is divided into forms:
- physiological (neonatal) - usually occurring in newborns (more often in weakened or premature infants) due to the adaptation of an immature enzyme system to new environmental conditions;
- parenchymal (liver) - usually occurring when the structure and function of liver cells (hepatocytes) are disrupted due to neoplasms and drug effects on the liver, or hepatitis or cirrhosis;
- hemolytic (suprahepatic) - usually occurring when red blood cells are destroyed and indirect bilirubin increases in anemia, lymphocytic leukemia, lymphosarcoma or tropical malaria;
- conjugation – usually occurring when the liver is exposed to provoking factors and congenital pathologies;
- mechanical (subhepatic) - usually occurring when direct bilirubin increases due to the inability to remove it through bile ducts blocked (by stones, tumors or helminths).
According to the duration of its course, jaundice is divided into:
- spicy;
- protracted;
- chronic.
List of sources
- Gubergrits N.B. Jaundice syndrome in clinical practice / Health of Ukraine. 2009, No. 12, pp. 30-33.
- Jaundice syndrome in the clinic of infectious diseases. Tutorial. Compiled by Valishin D. A., Kutuev O. I., Khunafina D. Kh., Burganova A. N., Khabelova T. A. Ufa, 2014. - 42 p.
- UN clinical syndromes in diseases of the hepatobiliary system. Educational and methodological manual. Compiled by Khvashchevskaya G. M., Nerobeeva S. I., Bobkov V. Ya., Kryzhanovsky V. L. Minsk: BSMU, 2018. – 24 p.
- Shcherbinina M.B. Modern views on the diagnosis and treatment of cholestatic liver diseases / Health of Ukraine, 2016, No. 3, pp. 5-6.
- Interpretation of liver tests and their abnormalities. Based on materials from Evaluation of Abnormal Liver Chemistries. Am J Gastroenterol advance online publication/Health of Ukraine. 2022, No. 17 (438), pp. 45-46.
Diagnosis of jaundice
Typically, the danger is not caused by jaundice itself, but by the pathologies that caused it. As a result of intoxication of the body with bilirubin, a serious failure of its various systems can occur, and in young children - mental retardation. Therefore, accurate diagnosis of this condition is so important, for which they carry out:
- comprehensive ultrasound of the abdominal cavity and retroperitoneal space;
- laboratory blood tests (general and biochemical blood tests);
- liver functional studies;
- liver biopsy.
Complications
Disturbances of brain structures progress and by 12-15 months they manifest themselves as strabismus
Bilirubin encephalopathy does not go away without leaving a trace. Disorders of brain structures progress and by 12-15 months they manifest themselves as convulsions, deterioration of vision, hearing, and strabismus.
Due to extensive damage to brain neurons, 90% of children develop hyperactivity syndrome, a developmental delay. There is also an increased risk of epilepsy.
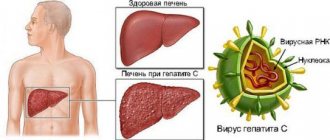
What is hepatitis
Hepatitis is an inflammatory process in the liver under the influence of a provoking (in most cases viral) agent, causing damage to its tissues.
Today, hepatitis is considered one of the most common infectious diseases after ARVI, influenza and chickenpox. Most often, the disease is diagnosed in young people aged 15-30 years (especially those prone to unprotected sex and drug use), another “risk group” is usually represented by medical specialists who have direct contact with blood (including infected people).
Prevention
Nonspecific prevention of viral enteral hepatitis (hepatitis A, E) includes:
- control over water supply (safety of drinking water) and sanitary condition of food facilities;
- compliance with the sanitary regime in medical institutions;
- wastewater disposal;
- timely diagnosis of the disease and urgent isolation of patients;
- maintaining personal hygiene (washing hands with safe water).
Specific prevention - vaccination
Prevention of hepatitis A consists of a two-time administration of the vaccine - Havrins-720 , Hep-A-in-VAK , Vakta , Avaxim . Vaccination is carried out at intervals of 6-12 months. Within one month, 100% of those vaccinated with one dose have antibody levels sufficient to provide protection. For the formation and sustainable immunity for many years (20 years), a second dose is recommended. Vaccination against hepatitis A is carried out from 3 years of age.
The following vaccines are used to prevent hepatitis B Euvax , Regevan-B , Engerix , Combiotech , HB-Vax-II , as well as combined ones - Bubo-Kok and Bubo-M . Bubo-Kok is a vaccine against whooping cough, diphtheria, tetanus and hepatitis B. Bubo-M against tetanus, diphtheria and hepatitis B. In children, vaccination is carried out according to the schedule 0 - 1 month -6 months.
Vaccination of adults is carried out in the following regimen:
- first - at any age;
- the second – after 30 days;
- the third – 4 months after the introduction of the first.
There is also a vaccine against hepatitis A and hepatitis B at the same time - Twinrix . Standard regimen for children and adults 0 - after 1 month - after 6 months.
For parenteral hepatitis (C, B, D), the safety rule is to avoid contact with biological (blood, mucus, saliva) human fluids. In the smallest doses, blood on razors, scissors and toothbrushes can become a source of infection. Protection during intimate relationships is also important. Maintaining the sterility of instruments for manicure, pedicure and tattooing is of no small importance.
What are the symptoms of hepatitis
It must be remembered that the symptoms of hepatitis can be vivid, but sometimes they can be almost completely absent (giving time for the undetected disease to become chronic). However, quite often all types of hepatitis are characterized by common symptoms of any intensity:
- jaundice;
- change in urine color (darkening to brown)
- pain (often pressing) in the liver area;
- indigestion (nausea, vomiting with a bitter taste, diarrhea or constipation);
- weakness and increased fatigue;
- increased body temperature and headache;
- skin itching;
- increased liver size.
Hepatitis classification
In its form, hepatitis can be acute or chronic.
Depending on the provoking factor, hepatitis is divided into:
- infectious (caused by viruses or bacteria);
- toxic (when the body is poisoned with alcohol, chemicals or drugs);
- autoimmune (caused by autoimmune pathologies);
- radiation (for example, as a consequence of radiation therapy).
Viral hepatitis, in turn, is divided into types (depending on the virus that provokes the disease):
- hepatitis A (Botkin's disease) - transmitted through contaminated food and water, with an incubation period of 2-6 weeks, after the disease giving lifelong immunity to this type;
- hepatitis B - transmitted through unprotected sexual contact and through open access to blood (at home, dentistry, cosmetology, etc.) using unsterilized instruments, with an incubation period of 1.5-6 months, the duration of the acute disease is from 6 to 8 weeks (with recovery in 90% of cases) and rare transition to chronic;
- hepatitis C is the most dangerous type, transmitted in the same way as hepatitis B, but with almost unnoticeable symptoms, which is why the disease can proceed unnoticed by the patient for years in a chronic form, leading to cirrhosis and liver cancer;
- hepatitis D – transmitted in the same way as hepatitis B and C, but developing only after infection with the hepatitis B virus, easily becoming chronic and ending in cirrhosis of the liver;
- hepatitis E is transmitted in the same way as hepatitis A, with similar symptoms, usually common in African and Asian countries.
Diet
Diet 5th table
- Efficacy: therapeutic effect after 14 days
- Duration: from 3 months or more
- Cost of products: 1200 - 1350 rubles per week
Diet Table No. 5a
- Efficacy: therapeutic effect after 5-7 days
- Time frame: 2-6 weeks
- Cost of products: 1300 - 1400 rubles per week
Diet Table 5b
- Efficacy: Therapeutic effect after 10 days
- Timing: Constantly
- Cost of products: 1300-1400 rubles per week
Gentle nutrition is aimed at restoring liver tissue and improving its function. At the height of the disease, a more strict Diet No. 5a , which is expanded - Diet No. 5 . Despite the restrictions, the diet should be complete, containing proteins and carbohydrates, and the amount of fat should be limited. The amount of protein is within 100-110 g due to animal protein: lean boiled meat and fish, low-fat cottage cheese, protein omelet, kefir and yogurt. Most meat dishes are steamed or baked in foil to prevent a crust from forming.
Vegetable oils (olive, sunflower, corn) are introduced into the diet as an additive to ready-made meals and vegetable salads. Butter is allowed in the amount of 20-25 g. Easily digestible carbohydrates (sugar, jam, honey, preserves, wheat bread, soft cookies) are allowed. The basis of complex carbohydrates is cereals - buckwheat, oatmeal, rice, semolina, wheat. Porridges are prepared with water or with the addition of milk. Boiled, steamed vegetables in the form of puree and soufflé. Pumpkin, potatoes, zucchini and cauliflower are allowed. The liquid is not limited; fruit, berry and vegetable juices, dried fruit compote, jelly, weak tea, herbal teas, and rosehip decoction are introduced. Food is taken in small portions up to 5-6 times a day. This diet promotes regular bile secretion and bile stagnation does not develop.
Pork, goose, duck, liver, kidneys, fried meat, smoked meats, canned food (meat and fish), any sausages, fish roe, radishes, turnips, white cabbage, garlic, onions, sorrel, spinach, pickled and pickled vegetables, all are excluded. spices, natural coffee, carbonated drinks, butter and puff pastry pastries, chocolate, halva, pastries with cream, ice cream. After suffering from viral hepatitis, patients must monitor their diet and strictly follow a diet for 6 months.
What is liver cirrhosis
Liver cirrhosis is a pathological and chronic process in the liver, as a result of which its parenchymal tissue is replaced by fibrous connective tissue (stroma). There is also a structural restructuring of the vascular bed and a decrease in the number of normally functioning hepatocytes (liver cells).
According to statistics, the global annual mortality rate from cirrhosis is about 300 thousand people, with a progressive upward trend. The disease most often affects men over 40 years of age, those prone to alcoholism, as well as patients with:
- chronic hepatitis B, C and D;
- pathologies complicated by fatty hepatosis;
- some hereditary diseases (for example, hemochromatosis);
- some autoimmune diseases;
- toxic liver damage from chemicals.
Mechanism of origin and development
The pathogenesis of the disease is directly related to the causes that caused it. If these are options in which the organ is affected by infection or toxins, sclerotic processes, oncology, a decrease in the rate of active hepatocytes, their functionality decreases. Moreover, this decrease can be reversible or irreversible.
As a result, free bilirubin undergoes uptake, glucuronidation and excretion into bile.
At the same time, reverse penetration of water-soluble bilirubin from the bile capillaries into the blood and lymph vessels is observed. The starting point in this process is a violation of bile secretion, which leads to its stop and secondary destruction of liver cells.
If we are talking about hereditary forms, then the source of the disease is a disrupted process of convergence of unbound pigment, which is associated with enzyme deficiency, which is congenital. However, direct bilirubin, due to a defect in the genetic nature of the transport system, also becomes the starting point for the onset of the disease.
As a consequence of the triggering of the disease development mechanism, the level of bilirubin increases, and the filtration of pigment by the kidneys increases. The latter causes bilirubinuria and dark urine and light-colored feces.
What are the symptoms of cirrhosis
Symptoms of cirrhosis may be completely absent for quite a long time, or appear slightly. Most often, the disease can begin to manifest itself:
- increased fatigue and decreased mental activity, weakness and irritability;
- indigestion (a feeling of bitterness in the mouth, nausea and vomiting, flatulence and upset stool), especially in the morning;
- pain in the right hypochondrium (increased after drinking alcohol or fatty foods, as well as during physical activity);
- increased bleeding in the mucous membranes and subcutaneous hemorrhages (with characteristic spider veins at the top of the body and redness of the palms);
- itchy skin and aching joints.
A long-term progressive disease is also characterized by:
- decrease in body weight and muscle volume;
- “protrusion” of the abdomen (against the background of thinning limbs with thickening fingertips) with an enlarged liver and spleen, ascites;
- painful swelling of the joints;
- jaundice;
- decreased sexual function and secondary sexual characteristics.
Clinical picture
Phases of kernicterus
The first distinguishing sign of kernicterus is the yellow discoloration of the skin and sclera. It is important to differentiate the condition from physiological jaundice, in which yellow skin is the only symptom.
In its development, bilirubin encephalopathy goes through two stages, characterized by certain symptoms:
- Asphyxia stage. First, the sucking reflex weakens while irritability increases. Muscle tone also decreases, intermittent breathing begins with complete stops for several seconds. These signs are characteristic of other pathologies, for example, sepsis.
- Spastic stage . At this stage, characteristic signs appear:
- Muscle hypertonicity.
- Muscle spasm in the back of the head.
- Difficulty straightening the arms and legs, clenched fists.
- Opisthotonus, that is, convulsions during which the baby sharply arches his back and throws his head back.
- Swollen fontanel.
- Sudden screams.
- Lack of facial expressions or twitching of facial muscles.
- “Sunset syndrome” - throwing back the head and rolling the eyes.
- Lack of reaction to loud noises and Moro reflex (baby startle).
- Chaotic frequent eye movements.
- Respiratory depression, cardiac arrest.
- Temperature increase.
These symptoms intensify over several days, then the baby’s condition gradually normalizes, but neurological abnormalities persist.
Diagnosis of cirrhosis
Diagnosis of the disease is based on the results of a comprehensive examination of the condition of the liver and organic systems most closely related to its work, as well as establishing the causes of cirrhosis. To do this:
- comprehensive ultrasound of the abdominal organs and retroperitoneal space (kidneys and adrenal glands), as well as portal vessels;
- laboratory blood test (including biochemical, for the presence of hepatitis viruses, as well as a coagulogram);
- esophagogastroduadenoscopy to identify dilated veins of the esophagus;
- liver biopsy and scintigraphy.
Treatment of cirrhosis
Typically, treatment of liver cirrhosis is aimed at stopping (in the initial stages of the disease) or slowing down progressive pathological processes. Conservative therapy is strictly individual and often consists of:
- taking medications (hepatoprotectors);
- following a diet (with the obligatory exclusion of alcohol, fatty and canned foods);
- excluding physical and emotional overload.
Treatment of end-stage cirrhosis can only be associated with liver transplantation.
It must be remembered that only a preventive comprehensive ultrasound of the abdominal organs in most cases can help to recognize pathological changes in the liver in time, even before the first symptoms appear! Save your health!
Causes
One of the main functions of liver cells (hepatocytes) is to capture, bind and release bilirubin into bile. Parenchymal jaundice develops in the following pathological conditions that impair the functioning of hepatocytes:
- Infectious diseases. The most common cause of liver tissue damage is viral hepatitis. Also, the organ parenchyma is susceptible to pathological changes during infectious mononucleosis, enterovirus and adenovirus infections, and leptospirosis.
- Liver failure, which is accompanied by the replacement of liver cells with connective tissue. Such changes are observed in cirrhosis and fibrosis.
- Exposure to hepatotoxic substances: chloroethane, ethylene glycol, alcohol, hydrazine. Parenchymal jaundice can also appear with drug-induced hepatitis caused by taking certain groups of antibiotics, cytostatic agents, anti-tuberculosis and some other drugs.
- Destruction of hepatocytes during intrahepatic stagnation of bile, which is observed in pathologies such as cholestasis of pregnancy, cystic fibrosis, cholangitis.
- Autoimmune hepatitis.
- Some hereditary diseases, for example, Gilbert and Krigder-Najjar syndrome, in which the manifestations of jaundice are caused by genetically mediated disorders of bilirubin metabolism.
The development of the parenchymal form of the syndrome can also be caused by extrahepatic pathologies. Severe heart failure, disseminated intravascular coagulation syndrome, and various types of shock can cause characteristic changes in hepatocytes.