Colitis is an inflammation of the mucous membrane of the large intestine. The disease is based on the development of dystrophic changes in the intestinal walls. Catarrhal colitis of the intestine is a certain stage in the development of pathology. Most often, the disease affects the ascending and descending sections of the colon. However, it does not cause irreversible changes in tissues.
In general, the prognosis of the disease is favorable. However, if left untreated, the catarrhal stage can transform into a more severe form. Among the provoking factors in the development of the disease, experts identify the penetration of pathogenic microorganisms, poor nutrition and weak immunity. The pathology causes pain, flatulence, and disruption of the bowel movement.
It is diagnosed at the very beginning and progresses rapidly with pronounced clinical symptoms. The disease does not have specific symptoms, so it is easy to confuse it with other pathologies. Treatment generally involves the use of conservative techniques. In some cases, pathology may develop not as a separate process, but against the background of food or alcohol poisoning. Properly administered therapy will prevent the disease from becoming chronic.
What it is
Catarrhal colitis of the intestine is the first phase of an acute inflammatory process in the mucous membranes of the organ. For a long time, the pathology can develop in an asymptomatic form. The period of exacerbation is characterized by rapid progression. The onset of serious inflammation is indicated by mucus in the stool. Colitis of the catarrhal type occurs against the background of erosions and hyperemia of the mucous membranes of the digestive organ. The disease provokes reversible changes in the intestines. Timely therapy allows you to completely restore the functional state of the gastrointestinal tract.
Pathogenesis:
- during the inflammatory process, the mucous membranes increase in size;
- Ulcers and hemorrhages appear on the intestinal tissues.
Traditional medicine in the treatment of ulcerative colitis
It is strictly not recommended to try to treat ulcerative colitis with “folk” remedies and alternative medicine. Considering the severity of the disease and the general danger it poses to the human body, all actions must be performed under the supervision and with the approval of a doctor.
Remember, even chronic diseases are not a death sentence, but a guide to action. Competent and timely diagnosis, professional consultation from highly qualified doctors and a personalized approach to therapy are the key to successful treatment and further fulfilling life.
You can make an appointment with a gastroenterologist at the Naedine Clinic by phone in Kirov: (8332) 32-7777 or through the form on our website.
Acute and chronic form
Catarrhal colitis of the intestine can develop in acute and chronic form. Each type of disease has its own characteristics of manifestation. Exacerbation of the inflammatory process begins with a sudden painful attack. General weakness is complemented by signs of tachycardia, increased body temperature, excessive sweating, and surges in blood pressure. When palpating the abdomen, the patient experiences pain.
If attacks of acute catarrhal colitis are ignored, the disease will take a chronic form. This type of pathology can develop asymptomatically for a long time. Regular attacks are inferior in intensity to the first version of inflammation.
Forms of chronic catarrhal colitis:
- hypertensive form (hypertonicity of the colon, narrowing of the intestinal lumen);
- spastic form (spasms caused by increased tone of the intestinal walls);
- distal form (hypertonicity of the sigmoid and descending intestines).
Acute colitis
Acute colitis develops rapidly
It occurs quite quickly and all the symptoms of this disease also develop rapidly. Symptoms:
- Repeated loose stools and vomiting
- A sharp increase in temperature, which can reach 38-39 degrees
- Ailments, weakness
- Loss of appetite
- Headache
- Dull or spasmodic pain in the abdominal area
Acute colitis is very dangerous for children under one year of age. Frequent bowel movements and repeated vomiting may cause dehydration or seizures. If acute colitis does not go away within 2 weeks, it becomes chronic. In this case, such patients periodically experience exacerbations.
Diagnosis and treatment
The diagnosis is made based on examination of the patient, as well as additional laboratory tests. In order to determine the causative agent of the disease, stool and blood tests are taken. To examine the intestinal mucosa, modern technologies are used in the form of endoscopy or x-rays.
Only after a thorough examination is a final diagnosis made.
Treatment occurs in two methods, which are used in parallel to each other. Maintenance therapy, which is aimed at preventing dehydration of the body. Drink plenty of water using water-salt solutions that restore water balance in the body.
Causes
Seasonal factors can provoke catarrhal colitis. For example, in the summer, with an abundance of vegetables and fruits, there is a risk of eating them unwashed. In combination with a poor diet and a low level of immunity, infection with pathogenic microorganisms triggers the development of an inflammatory process on the mucous membranes of the digestive organs. Common causes of the disease include an unbalanced diet.
Sudden changes in diet (for example, when following a diet) can also be a trigger for colitis.
Main reasons:
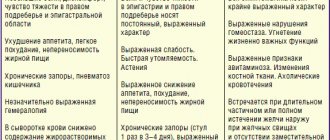
In the photo you can see different pictures of damage to the colon, associated with the scale of the inflammatory process and its localization. compliance with too strict dietary programs;- progression of intestinal dysbiosis;
- infection with parasitic infections;
- a critical decrease in the body's protective functions;
- complications of food poisoning;
- deficiency of minerals in the body;
- uncontrolled use of medications;
- progression of ischemic colitis;
- complications of chronic constipation;
- consequences of injuries to the intestine and its mucous membranes;
- exacerbation of chronic pathologies of the digestive tract.
Symptoms
If you have several symptoms of catarrhal colitis, you should consult a doctor and undergo a comprehensive examination. The danger of the disease lies in the rapid transition from the acute to the chronic phase. The severity of pain during inflammation depends on the general clinical picture of the patient’s health.
A significant deterioration in the condition of the body is observed with diffuse colitis (each intestinal calving occurs).
Other possible symptoms:
- sudden mood changes and insomnia;
- pain in the digestive system;
- pain in the intestines that subsides after defecation;
- increased gas formation;
- belching and bitter taste in the mouth;
- causeless bouts of vomiting and regular nausea;
- general weakness of the body;
- increased body temperature combined with chills;
- bad breath;
- impurities of blood or mucus in the stool;
- disturbances in the process of bowel movement (diarrhea or constipation);
- signs of intoxication of the body.
With the total form of catarrhal colitis, about 18% of the organ is affected, with the left side - 28%, with rectosigmoid - 54%.
Severe/fulminant UC
According to the current definition, UC with more than 6 bowel movements per day, fever, tachycardia and anemia is considered severe. The use of 5 ASA drugs may lead to worsening of colitis and is therefore not recommended. In this case, the mainstay of therapy is intravenous steroids (prednisolone). The optimal dose is 48 mg per day (16 mg every 8 hours or 2 mg per hour infusion), although bolus administration is also possible. Total parenteral nutrition is also indicated. If there is no effect from 7-day therapy, the question arises of surgical treatment - colectomy. Alternatively, cytostatics such as cyclosporine at a dose of 4 mg/kg/day can be used. Within 7 days of treatment, the effect is achieved in 60-80% of patients [9, 10] , after which the patient is transferred to oral administration of the drug (6-8 mg/kg/day) with a simultaneous gradual reduction in the dose of steroids.
Diagnosis of the disease
To confirm the diagnosis of catarrhal colitis, a number of procedures are necessary. A general analysis of blood, urine and feces should confirm the presence of inflammation in the body. Biochemical studies can determine the degree of damage to the digestive organs. Instrumental procedures are necessary to visualize the changes occurring in the mucous membranes.
Diagnosis of colitis. Diagnostic stages:
- blood test for leukocytosis;
- general analysis of stool;
- colonoscopy;
- endoscopy;
- fluoroscopy;
- anoscopy;
- irrigoscopy.
Treatment
Therapy for catarrhal colitis includes two mandatory methods - taking medications and following a diet. Some folk remedies are a good addition to the main course of treatment. If colitis is detected in an advanced stage, then surgical intervention may be required (for this type of inflammation, surgery is used in isolated cases).
Drug therapy
Treatment of catarrhal colitis is carried out with a complex of several drugs. Medicines should relieve pain, restore intestinal microflora, remove waste products of pathogenic microorganisms from the body and destroy bacteria. Each task is performed by separate types of medications.
Only a doctor can prescribe an effective course of therapy.
Examples of drugs:
- painkillers antispasmodics (No-Shpa, Duspalitrin);
- enzyme preparations (Smecta, Enterosgel);
- antimicrobial medications (Loperamide, Furazolidone);
- adsorbents (Almagel).
Diet food
Recommendations for adjusting the diet for colitis depend on the form of the disease and the degree of damage to the intestinal mucous membranes. During the acute phase, therapeutic fasting is recommended. Eating can cause additional stress on the intestines and worsen the patient's condition.
It is recommended to adhere to fasting only during the period of severe symptoms of an attack.
Nutrition principles:
- during the therapy period, all products are thoroughly crushed (food should have the consistency of puree);
- the first products on the menu after fasting should be cottage cheese and kefir;
- vegetables, fruits, lean meats and fish, cereals, soups are gradually introduced into the diet;
- vegetables and fruits are recommended to be consumed after heat treatment;
- The nutrition program Diet No. 4 is taken as the basis for creating the menu;
- You should not consume dairy products with a high percentage of fat (including whole milk);
- the number of sweets on the menu is reduced (confectionery, butter and sweet pastries, cakes, pastries);
- food is consumed in small portions, but up to six times a day;
- Dishes should be prepared by steaming, stewing or boiling;
- Products with an aggressive effect on the digestive tract (legumes, cabbage, radishes, radishes, mushrooms, seasonings and spices) are excluded from the diet.
You need to eat in small portions. Dishes should definitely be cooked without oil, and preferably steamed.
Folk remedies
Alternative medicine recipes can be used as an adjunct to drug treatment. Plant components have a beneficial effect on the functioning of the digestive tract and the condition of the intestinal mucous membranes. Before using folk remedies, the presence of an allergic reaction should be ruled out. Recipes based on herbal ingredients cannot replace drug therapy.
Examples of traditional medicine:
- microenemas with potato juice (dilute potato juice in equal quantities with water, the resulting liquid is used for an enema, potato juice heals wounds well and slows down inflammatory processes);
- bergenia root (pour a teaspoon of raw material into a glass of boiling water, leave for thirty minutes, take small portions throughout the day);
- herbal decoctions (to make medicinal decoctions, you can use oak bark, St. John's wort and chamomile; independent decoctions are prepared based on such ingredients; it is permissible to mix the components in equal proportions);
- honey (three times a day before main meals, it is recommended to drink a glass of water with a teaspoon of honey diluted in it; the product is suitable for use only in the absence of an allergic reaction to bee products).
Catarrhal colitis of the intestine - what is it and how to treat it?
What drugs are prescribed for atrophic colitis and its other forms?
In the treatment of colitis, conservative and surgical methods are used.
Conservative treatment
Patients are interested in what medications should be taken for atrophic colitis or its other forms. This is determined by the doctor in each specific case. Based on the appointments:
- diet;
- antibacterial or antiparasitic drugs;
- agents that improve blood flow in the intestinal wall;
- intestinal adsorbents;
- laxatives or antidiarrheals;
- agents that improve the condition of normal intestinal microflora;
- detoxification therapy;
- immunomodulators;
- pain relief. The doctor decides what medications to use to relieve pain in acute colitis of the rectum or other locations.
Surgical treatment
It is used for severe complications such as ulcerative colitis or progressive ischemia of the large intestine.
If the damage is significant, resection (removal) of part of the intestine is performed. This is fraught with deterioration of its functions:
- absorption of vitamins;
- absorption of fluid and formation of feces.
Complications
Catarrhal colitis in the early stages does not pose a threat to the patient's life. This type of pathological process is the first phase of inflammation of the mucous membranes. With proper treatment, the risk of negative consequences and complications is minimal.
If the symptoms of disorders in the digestive tract are ignored, then their progression causes irreversible changes in the intestines.
Possible complications:
- peritonitis;
- massive gastrointestinal hemorrhages.
UC with steroid refractoriness/dependence
In this case, the drugs of choice are Azathioprine (2.5 mg/kg/day) and 6-mercaptopurine (1.5 mg/kg/day). Their use makes it possible to achieve remission and stop using steroids in approximately 2/3 of patients [1,2] . However, the effect of their use occurs after 2-3 months of treatment (the process of reducing the dose of steroids should not begin earlier), and the risk of side effects is high. Therapy with this group of drugs is also indicated for patients with a relapse of UC when the dose of prednisolone is reduced below 15 mg per day, with a relapse within 6 weeks after stopping steroid treatment, and also for patients requiring two or more courses of steroid therapy per year.
Prevention
In most cases, the symptoms of catarrhal colitis are a consequence of poor personal hygiene or poor nutrition. Eliminating these factors helps reduce the risk of inflammation. Products that are intended for fresh consumption (vegetables, fruits, berries) must be fully processed to remove contamination. Regular quick snacks can disrupt the functional state of the digestive tract and provoke the onset of colitis.
Other preventive measures:
- strengthening the body’s immune system (taking vitamins, eating healthy foods, healthy lifestyle);
- regular examination by a gastroenterologist (especially if there are signs of abnormalities in the digestive tract);
- avoiding uncontrolled use of medications that can have a negative effect on the digestive tract and intestinal microflora.
Drug-induced colitis
This type of disease occurs as a result of long-term use of drugs that negatively affect the intestinal microflora. These include: laxatives, antibiotics and individual intolerance to certain types of drugs.
Drug-induced enterocolitis occurs due to improper treatment, and most often in people who try to treat themselves. Incorrect dosage or choice of drug can lead to serious consequences, including the occurrence of colitis. Don't treat yourself.