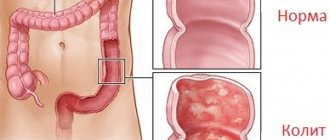
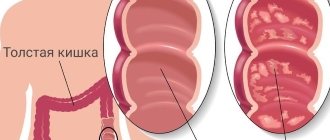
Colitis is an inflammatory disease that affects the large intestine. As the disease progresses, the intestinal mucosa atrophies, disrupting the functioning of one of the most important organs of the digestive system. Colitis can occur in all parts of the intestine at once (then it is called pancolitis) or in a specific section (then it is called segmental).
The symptoms are specific and extremely unpleasant, so patients usually consult a doctor on time. Often acute colitis becomes chronic; one of the most serious forms is ulcerative colitis. Erosion and ulcers form in the intestinal mucosa; symptoms occur during exacerbations.
At CELT you can get advice from a gastroenterologist.
- Initial consultation – 4,200
- Repeated consultation – 3,000
Make an appointment
Why does colitis develop?
Colitis is a polyethological disease. This means that doctors identify many different reasons for the development of this disease. The main reason is infection of the intestines by pathogens - bacteria, protozoa, helminths.
In addition to the direct cause, there are risk factors that can increase the likelihood of developing colitis:
- Taking medications that inhibit the natural intestinal microflora. As a result, normal flora dies and pathogenic microorganisms take its place. This result can be caused by: antibiotic therapy, long-term use of laxatives, and the use of suppositories.
- Chronic poisoning - chemical or food. Toxins penetrate the intestines through the bloodstream and inhibit the natural microflora.
- Stress, physical and mental overload.
- Exposure to heavy metal salts, work in hazardous industries.
- Diseases associated with circulatory disorders.
- Poor eating behavior: eating insufficiently processed food, frequent snacking on the go, dry food, addiction to spicy, salty and fatty foods.
- Alcohol abuse.
Causes of chronic colitis
Chronic colitis can be associated with acute intestinal infections (dysentery, salmonellosis, yerseniosis, etc.), helminthic and parasitic infestations. Among colitis of non-infectious origin, radiation, toxic, allergic, ischemic, and nutritional (with systematic violation of the diet) are distinguished.
Toxic colitis occurs as a result of long-term intoxication with compounds of mercury, lead, phosphorus, arsenic, drugs (cytostatics), etc. Toxic colitis can also occur due to irritation of the intestinal wall by products formed in the body that are excreted by it (with renal failure, gout).
Colitis of an allergic nature is observed with food allergies, with intolerance to certain medications and chemicals, and increased individual sensitivity of the body to certain types of bacterial intestinal flora and decay products of microorganisms.
Drug-induced colitis is associated with long-term uncontrolled use of laxatives, non-steroidal anti-inflammatory drugs, antibiotics and some other drugs. Chronic colitis can develop in the presence of foci of infection in the gallbladder, pancreas and other organs anatomically connected to the intestines, as well as with prolonged monotonous nutrition, systematic consumption of large quantities of indigestible food, abuse of spicy foods, and alcohol. Often, with chronic colitis, several factors mutually enhance the pathogenic effect.
Classification
There are several types of colitis:
- Ulcerative. Experts still find it difficult to name specific mechanisms for the development of this disease. It is known that the risk is increased by hereditary predisposition, as well as infectious diseases of the gastrointestinal tract.
- Infectious. Develops after infection with pathogenic and opportunistic microorganisms.
- Ischemic - occurs against the background of damage to blood vessels - the branches of the abdominal aorta, and the blood supply to the intestine is disrupted.
- Toxic. Occurs against the background of poisoning with various chemicals, including uncontrolled use of medications.
- Radiation is a consequence of radiation sickness. Anyone who works in an area of high radiation exposure, as well as patients receiving radiation therapy, are at risk.
- Spastic - the exact causes have not been established.
- Microscopic – lymphocytic, collagen. Inflammatory changes are diagnosed only by histological examination.
Symptoms and treatment of colitis depend on the type of colitis diagnosed.
Microscopic colitis and irritable bowel syndrome with diarrhea: difficulties in differential diagnosis
Microscopic colitis (MC) is a special form of chronic inflammatory bowel disease, which is characterized by specific changes in the colon.
Regarding histological changes, lymphocytic colitis (the presence of significant infiltration of the colon mucosa with intraepithelial lymphocytes with preserved mucosal architecture) and collagenous colitis (thickening of the basement membrane due to collagen deposits in it) are distinguished. The dominant, and often the only clinical manifestation in such patients is diarrhea without pathological impurities.
The first description of microscopic colitis was made by Lindstrom and Freeman in 1976, which made it possible to distinguish this pathology from infectious and intestinal diseases. Since then, little data on MK has been obtained, the disease continues to remain poorly understood, and the reasons for its occurrence and progression are not fully understood. This may be due to the low prevalence of MC (103.00 per 100,000 people, M. Storr et al. Microscopic Colitis: Epidemiology, Pathophysiology, Diagnosis and Current Management—An Update 2013. ISRN Gastroenterol. 2013).
It is believed that lymphocytic and collagenous colitis develops as a result of the interaction of several factors, among which heredity, the state of the intestinal microflora, and immune disorders are of particular importance. Smoking and the influence of drugs (aspirin, lisinopril, ranitidine, madopar, simvastatin) are considered as possible trigger mechanisms for the development of the disease.
Today, therapy methods have been developed that allow, if not to cure such patients, then to improve their quality of life. In clinical practice, one of the most common diseases in which diarrhea without pathological impurities is observed is irritable bowel syndrome (IBS). Thus, practicing doctors are often faced with the need for a differential diagnosis when such diarrhea is detected. To clarify and describe the differences between MK and IBS, a large multicenter study was conducted in France.
Goals and methods
The aim of this prospective study was to describe the characteristics of a cohort of patients with urticaria and compare them with patients with IBS with diarrhea. This study was conducted in 26 medical centers in France. Inclusion criteria were: diarrhea without pathological impurities at least 3 times a day, disease duration of more than 3 weeks and the absence of organic pathology during colonoscopy. In this case, each patient underwent biopsies from the area of the cecum and all parts of the colon during colonoscopy, and also underwent esophagogastroduodenoscopy with the collection of biopsy material from the stomach and duodenum.
The diagnosis of “lymphocytic colitis” was established based on the detection of more than 20% of intraepithelial lymphocytes in the colon mucosa and “collagen colitis” based on thickening of the basement membrane of more than 10 microns due to collagen deposits. The obtained data were statistically processed and compared with each other.
results
Of the 433 people included in the study, 129 were diagnosed with MK (lymphocytic colitis in 87 and collagenous colitis in 42 patients), 278 subjects were diagnosed with IBS with diarrhea, as a result of which they were assigned to the control group. Organic pathology was detected in 26 participants. The diagnostic yield of biopsy was higher in the transverse colon, with lymphocytic colitis 96% and collagenous colitis 98.5%, and lower in the rectum, 83% and 78%, respectively. Taking medications was noted in 53% of patients with MK; a connection with autoimmune diseases was detected in 34% of cases.
In statistical analysis, a significant difference between the groups of patients with MK and IBS was observed in such characteristics as: average age (61 g for MK vs. 47 years for IBS, p
Conclusion
In this multicenter prospective study, the most reliable factors for establishing a diagnosis of microscopic colitis were identified: age over 50 years, onset of diarrhea at night, weight loss, receiving new medications within a period of no more than 3 months, and the presence of autoimmune diseases. Association with medications and autoimmune pathology is more often associated with collagenous colitis. It was also found that the diagnostic accuracy of biopsies was maximum in the transverse colon and minimum in the rectum. The data obtained are intended to help practicing physicians in diagnosing MK and its treatment.
Source: Microscopic colitis or irritable bowel syndrome with diarrhea: prospective multicenter study. G. Macaigne et al. UEG journal, 2013. p. A78.
Symptoms of colitis
Symptoms manifest in different ways. There are main signs of colitis - diarrhea and abdominal pain, but there are symptoms that may not appear for a long time.
Signs of colitis include:
- Abdominal pain of varying intensity and localization, constant or occurring at regular intervals.
- Bloating and flatulence, discomfort in the intestinal area.
- Periodically occurring chills, fever.
- Diarrhea, which may alternate with constipation.
- Frequent urge to defecate, including false ones.
- An admixture of blood and mucus in the stool. It is important to know that this symptom is characteristic of many intestinal diseases and in any case requires consultation with a doctor.
- Symptoms of dehydration with severe diarrhea: dizziness, weakness, rare urination, dry mouth, dry skin, feeling of “sand in the eyes.”
In adults, local intestinal signs of colitis are accompanied by general malaise. Weight loss may occur. Symptoms disappear with treatment. Progress before starting therapy. In the chronic form, sometimes you feel better than in the acute form. Symptoms are less obvious. Worries include loss of appetite, decreased performance, belching and nausea.
Signs of colon inflammation
The main symptoms of colitis include moderate to severe pain, tenderness at the site of inflammation, increased bowel movements, persistent diarrhea with blood or pus, fecal incontinence, increased gas, loss of appetite, fatigue and unexplained weight loss. Metabolic and electrolyte disturbances occur due to disruption of absorption processes.
More severe illness may include rapid or irregular heartbeat, difficulty breathing, and a high fever.
Less common symptoms include joint pain, mouth ulcers (stomatitis), bloodshot eyes, and skin rashes.
Chronic pain and poor health can cause anxiety and affective mood disorders in patients.
Survey
Colonoscopy
- Cost: 25,000 rub.
More details
Diagnosis begins at a consultation with a gastroenterologist with examination and questioning. The nature of pain and discomfort and their duration play a big role. When diagnosing colitis, a whole range of instrumental studies is used:
- Colonoscopy. The most common endoscopic examination of the intestine.
- Sigmoidoscopy (examination of the rectum and anal area).
- Laboratory examination of stool (scatology, bacterial examination, inflammatory markers - calprotectin and others).
- X-ray examination using a contrast agent (irrigoscopy). Allows you to detect the exact localization of inflammation.
- Biopsy of the mucosa for histological examination. Allows you to clarify the diagnosis and exclude the possibility of a malignant neoplasm, which often manifests itself with the same symptoms as colitis.
Diagnostics is aimed at collecting the maximum amount of data about the disease. The doctor tries to find out the cause (it must be eliminated during treatment) and to clarify the localization of the inflammatory process. The more accurate the examination, the easier it is to choose effective treatment tactics.
How to treat intestinal colitis in adults
Chronic colitis is treated on an outpatient basis or in a hospital, depending on the severity of the condition. The doctor selects treatment tactics. If the cause of acute colitis is an infectious agent, then treatment is carried out in the infectious diseases department.
For any type of colitis, depending on the clinical picture, the following prescriptions are made:
- Diet 4 or 3.
- Taking adsorbent drugs.
- Drugs that normalize intestinal motility.
- Laxatives or antidiarrheals.
- Drugs that stimulate the regeneration of the intestinal mucosa.
- Anti-inflammatory drugs.
- Preparations that promote the growth of normal microflora (prebiotics and probiotics).
- Detoxification.
- Taking vitamins, minerals, treatment with mineral waters, physical therapy.
During treatment, it is necessary to try to eliminate the cause of colitis, for which the following are prescribed:
- antiparasitic drugs;
- antimicrobials;
- vascular drugs to improve blood circulation.
Colitis is a disease that is sufficiently amenable to conservative treatment. CELT clinic specialists will help you cope with the problem. Examination using the latest equipment guarantees an accurate diagnosis. Many years of experience of doctors works for your health.
Complications
In the absence of timely treatment, colitis can cause the following complications:
1. Development of ulcerative colitis. Ulcers usually form in old forms of colitis, when the causative factor affects the intestinal mucosa for a long time. Ulcers can lead to perforation of the intestinal wall and the release of contents beyond its boundaries, which is fraught with infection and the development of sepsis. Perforation also results in severe internal bleeding, which requires immediate surgical intervention. Otherwise, everything could end in death.
2. Blood poisoning (sepsis). The intestines have a complex branched circulatory system, so any damage to its walls leads to rupture of blood vessels. Feces contain a large number of harmful substances and pathogenic microorganisms, which, if the integrity of the intestinal wall is damaged, are absorbed into the systemic bloodstream, which can lead to the development of sepsis. The likelihood of developing this complication is especially high in infectious colitis.
3. Intestinal obstruction . A fairly common and extremely dangerous complication of colitis. As a result of the inflammatory process, intestinal motility worsens, feces are not evacuated in a timely manner and acquire a rocky structure. Gradually they accumulate and completely close the intestinal lumen, causing obstruction. In this case, the patient needs urgent surgery, otherwise everything can end in death.
4. Intoxication of the body . Colitis, especially its chronic form, always leads to the development of stagnant processes in the intestines. As a result, toxins are not removed, but are reabsorbed into the blood, poisoning the body. Intoxication is manifested by symptoms such as causeless weakness, decreased performance, decreased appetite, headaches of unknown etiology and a number of others.
5. Dehydration . Due to frequent diarrhea, most of the liquid does not have time to be absorbed by the body due to irritation of the mucous membrane and disruption of its absorption capacity, which leads to dehydration.
Our services
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Sigmoidoscopy | 2 500 |
| Colonoscopy (video colonoscopy) | 7 000 |
| Irrigoscopy | 7 000 |
All services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions