Indigestion is one of the most common ailments that force patients to seek medical help. Gastrointestinal pathology in children ranks second after respiratory diseases, and in adults, according to various observations, it ranks second or third.
In recent years, epidemiological studies in various countries have shown a rapid increase in the incidence of gastrointestinal diseases throughout the world. In some regions, especially in industrialized, "stressful lifestyles", these diseases are already at the forefront of prevalence statistics.
This was widely discussed at an expert symposium of the gastroenterology section of the European Union of Medical Specialists (UEMS). Research data presented at the event shows that in some Western countries, gastrointestinal diseases kill more people than coronary heart disease, and these negative trends are becoming more pronounced.
Causes
The content of the article
Experts attribute the rise in digestive disorders to many factors: increasing life expectancy (aging population), unhealthy and irregular diets, food contamination, the use of various gastrointestinal toxic drugs, allergies, infections, long-term stress and much more.
Gastrointestinal diseases are becoming an important issue for quality of life, public health, and the economy due to their increasing prevalence and difficulty in treating them.
Complex and fragile organ
The gastrointestinal tract begins in the oral cavity and ends in the anus. The large area of the mucous membrane leads to a very intense interaction of the body (mechanical and chemical) with food and other substances entering through the mouth. Although the mucous membrane of the gastrointestinal tract has a huge reserve of regeneration (a new one is restored within a few days), pathogens, toxins and other substances that constantly enter it can accumulate and their harmful effects develop into pathology over time.
Each segment of the gastrointestinal tract performs a specific function: food is mechanically crushed in the oral cavity, carbohydrates are fermented (broken down: the enzymes ptyalin, salivary amylase, proteins - trypsin, etc. work here), and are digested in the stomach. The ducts of the liver (bile) and the exocrine glands of the pancreas open into the duodenum, so the most important and active processes of breakdown of nutrients and preparation for absorption in the intestine occur in this segment of the gastrointestinal tract.
The greatest burden on the digestive function falls on the pancreas, since it is the only one in the human body that synthesizes and secretes the three most important digestive enzymes:
- amylase (breaks down carbohydrates);
- trypsin (for proteins);
- lipase (for fat).
All these enzymes are part of pancreatin (pancreatic juice). It is necessary to break down fats - the enzyme lipase is produced in the human body only by the pancreas. Pancreatic lipase cannot be replaced by any other digestive enzyme, so it is lesions of the pancreas (exocrine insufficiency) that cause the most severe symptoms of gastrointestinal dysfunction and are the most difficult to correct.
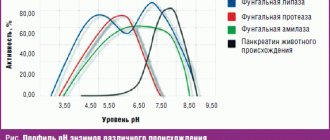
Lipase is the most problematic enzyme because it is the most unstable: it is broken down faster than amylase or trypsin by organic acids (in the stomach), higher temperatures, contact with drugs and chemicals, etc.
Associated technological difficulties in the production of pancreatin preparations: protection of pancreatic enzymes (primarily lipase) from aggressive gastric juices and preservation of activity in the duodenum, the physiological epicenter of the digestive process.
Food is a source of energy and building material
To maintain his life, a person must eat food.
Food products contain all the substances necessary for life: water, mineral salts and organic compounds. Proteins, fats and carbohydrates are synthesized by plants from inorganic substances using solar energy. Animals build their bodies from nutrients of plant or animal origin. Nutrients that enter the body with food are building materials and at the same time a source of energy. During the breakdown and oxidation of proteins, fats and carbohydrates, a different but constant amount of energy is released for each substance, characterizing their energy value.
Chronic pancreatitis and other conditions
Chronic pancreatitis and other conditions
Pancreatic enzyme medications are among the most commonly used medications. This is due to two factors: the high prevalence of indigestion and their negative impact on the quality of life and the safety of these drugs (close to physiological).
The most important and most motivated indication for prescribing pancreatin drugs is the absence of exocrine (digestive) pancreatic enzymes, when replacement therapy with these enzymes is required.
Complete (true) pancreatin deficiency most often occurs in patients with chronic pancreatitis. It is worth remembering that overdiagnosis of chronic pancreatitis is a common occurrence in clinical practice.
It has been found that the exocrine reserve of the pancreas is very high, so pancreatin (digestive enzyme) deficiency becomes clinical (symptomatic) only when the pancreatic tissue is severely damaged.
Special studies show that symptoms of exocrine pancreatic insufficiency occur in about 90% of patients. The parenchyma of the pancreas, and its remaining functionally active tissue, is not able to satisfy the need for enzymes necessary for digestion.
Chronic pancreatitis is not a common disease. Most often (up to 75-80% of cases), it occurs in people with chronic alcoholism. Research shows that signs of chronic pancreatitis (including enzyme deficiency) occur within an average of 10 years of continuous alcohol consumption. What in everyday life (sometimes in everyday clinical practice is called “chronic pancreatitis”) often turns out to be a digestive disorder of another etiology, including psychogenic, functional.
Types of enzymes
When food breaks down into molecules, the creation of building material is ensured, which is involved in the process of construction and functioning of cells, tissues and organs. The course of metabolism depends on the degree of supply of energy material. The absorption process occurs at all levels of the digestive tract, the beginning of which is already noted in the mouth.
Many people are concerned about the question of why salivary enzymes are active in the oral cavity, but lose their properties when they enter the stomach. This is explained by the fact that enzymes are active in a slightly alkaline environment (saliva pH is on average 7.4-8.0), while in an acidic environment they are inactivated. In addition, proteolytic elements are connected to the digestion process in the stomach, which are more actively involved in the breakdown process.
Types of enzymes that act in general during digestion:
| Carbohydrate metabolism | Fatty | Protein |
| Amylase, maltase. | Lipase | Proteases: pepsin, trypsin, chymotrypsin. |
Amylase
The main enzyme in the oral cavity is this enzyme, also called ptyalin. Its participation is noted in the breakdown of carbohydrates. Range of action: oral cavity, esophagus.
When food enters, starch and glycogen begin to break down into maltose, which then, under the influence of other components, breaks down into glucose with the release of energy.
Quickly digestible carbohydrates are easily subject to destruction processes. The partially processed component in the form of sucrose is able to be absorbed through the bottom of the mouth, providing the effect of rapid saturation when eating sweets.
The synthesis of this enzyme is noted not only in the salivary glands, but also in the pancreas. The combined action of enzymes allows the process of carbohydrate breakdown to be completed in full.
The photo shows the general scheme of glycolysis.
Lipase
When exposed, reactions occur that decompose fats into glycerol and fatty acids. Mainly synthesized by secretory cells of the stomach.
Under the influence of the substance, milk fats are broken down. Having the optimal amount is especially important in young children, since enzymatic systems are poorly expressed.
Proteases
The action instructions involve the breakdown of proteins into amino acids. Synthesis occurs only in the stomach and pancreas.
The stomach produces pepsinogen (an inactive form), which, after coming into contact with hydrochloric acid, is converted into pepsin. The pancreas is involved in the secretion of trypsin and chymotrypsin. Under the general influence of enzymes, the protein part of food breaks down.
Exocrine pancreatic dysfunction - pathogenesis
Indigestion occurs when the pancreas cannot produce enough enzymes and other active substances needed to break down food and meet physiological needs. With pancreatic insufficiency, the symptoms of malabsorption become more pronounced: the absorption of nutrients in the intestine is impaired, signs of a lack of substances that are very important for the body appear (steatorrhea is oily, shiny, very unpleasant-smelling), feces (a sign of lipase deficiency).
Absolute pancreatin deficiency usually occurs in patients with:
- chronic pancreatitis;
- cystic fibrosis (a hereditary disease that increases the viscosity of many glands and secretes leakage);
- after surgery to remove part of the pancreas or other segments of the gastrointestinal tract.
Exocrine pancreatic insufficiency is much less common in patients with:
- stomach ulcer;
- celiac disease;
- Crohn's disease;
- systemic lupus erythematosus.
In clinical practice, relative deficiency of pancreatic enzymes often occurs for two reasons:
- increased demand for pancreatic enzymes (rich and difficult to digest food);
- gastrointestinal infections, dyskinesia, etc.;
- when it is necessary to compensate for the loss of function of other parts of the gastrointestinal tract (after resection of the stomach, intestines, cholecystectomy, etc.).
Small intestine
The small intestine is the longest part of the digestive tube, reaching 6–7 meters in an adult. It consists of the duodenum, jejunum and ileum.
The excretory ducts of two large digestive glands - the pancreas and liver - open into the initial section of the small intestine - the duodenum. Here the most intensive digestion of food gruel occurs, which is exposed to the action of three digestive juices: pancreatic, bile and intestinal.
The pancreas is located behind the stomach. It distinguishes between the apex, body and tail. The apex of the gland is surrounded in a horseshoe shape by the duodenum, and the tail is adjacent to the spleen.
Gland cells produce pancreatic juice (pancreatic). It contains enzymes that act on proteins, fats and carbohydrates. The enzyme trypsin breaks down proteins into amino acids, but is active only in the presence of the intestinal enzyme enterokinase. Lipase breaks down fats into glycerol and fatty acids. Its activity increases sharply under the influence of bile produced in the liver and entering the duodenum. Under the influence of amylase and maltose in pancreatic juice, most food carbohydrates are broken down into glucose. All pancreatic juice enzymes are active only in an alkaline environment.
In the small intestine, food gruel undergoes not only chemical, but also mechanical processing. Thanks to the pendulum-like movements of the intestine (alternate lengthening and shortening), it mixes with digestive juices and liquefies. Peristaltic movements of the intestines cause contents to move towards the large intestine.
The liver is the largest digestive gland in our body (up to 1.5 kg). It lies under the diaphragm, occupying the right hypochondrium. The gallbladder is located on the lower surface of the liver. The liver consists of glandular cells that form lobules. Between the lobules there are layers of connective tissue in which nerves, lymphatic and blood vessels and small bile ducts pass.
Bile, produced by the liver, plays a large role in the digestion process. It does not break down nutrients, but prepares fats for digestion and absorption. Under its action, fats break up into small drops suspended in liquid, i.e. turn into an emulsion. In this form they are easier to digest. In addition, bile actively influences absorption processes in the small intestine, enhances intestinal motility and the secretion of pancreatic juice. Despite the fact that bile is produced continuously in the liver, it enters the intestines only when eating. Between periods of digestion, bile is collected in the gallbladder. Through the portal vein, venous blood flows into the liver from the entire digestive canal, pancreas and spleen. Toxic substances that enter the blood from the gastrointestinal tract are neutralized here and then excreted in the urine. In this way, the liver carries out its protective (barrier) function. The liver is involved in the synthesis of a number of important substances for the body, such as glycogen, vitamin A, and influences the process of hematopoiesis, the metabolism of proteins, fats, and carbohydrates.
Clinic and symptoms
Clinic and symptoms
Pancreatic enzyme deficiency manifests itself in:
- abdominal discomfort (pain, swimming, bloating, gurgling, etc.);
- signs of disturbance, breakdown of nutrients (primarily fats) - steatorrhea.
Poor intestinal absorption can lead to some symptoms of nutrient deficiency, such as: blurred vision in the dark (vitamin A deficiency), bone pain, muscle twitching, cramps (electrolyte imbalance) and bruising (impaired clotting factor synthesis). blood).
Nutrient Absorption
In order for the amino acids, simple sugars, fatty acids and glycerol resulting from the breakdown to be used by the body, they must be absorbed. These substances are practically not absorbed in the oral cavity and esophagus. Water, glucose and salts are absorbed in the stomach in small quantities; in the large intestines - water and some salts. The main processes of nutrient absorption occur in the small intestine, which is quite well adapted to carry out this function. The mucous membrane of the small intestine plays an active role in the absorption process. It has a large number of villi and microvilli, which increase the absorption surface of the intestine. The walls of the villi contain smooth muscle fibers, and inside them there are blood and lymphatic vessels.
Villi take part in the absorption of nutrients. By contracting, they promote the outflow of blood and lymph, rich in nutrients. When the villi relax, fluid from the intestinal cavity again enters their vessels. The products of the breakdown of proteins and carbohydrates are absorbed directly into the blood, and the bulk of digested fats are absorbed into the lymph.
Principles of treatment
Depending on the cause and course of exocrine pancreatic insufficiency (absolute, long-term or relatively short-term), treatment can be episodic or long-term.
In case of irreversible pancreatic insufficiency, enzyme preparations must be used for a long time, even throughout life, but their dose varies depending on the amount and nature of food eaten, the functional state of the digestive organs, and concomitant diseases.
Treatment consists of two stages: diet and pancreatin replacement therapy.
Digestive organs
The alimentary canal is a tube that runs throughout the body. The canal wall consists of three layers: outer, middle and inner.
The outer layer (serous membrane) is formed by connective tissue that separates the digestive tube from surrounding tissues and organs.
The middle layer (muscular layer) in the upper parts of the digestive tube (oral cavity, pharynx, upper part of the esophagus) is represented by striated muscle tissue, and in the lower parts - smooth muscle tissue. Most often, the muscles are located in two layers - circular and longitudinal. Thanks to the contraction of the muscular membrane, food moves through the digestive canal.
The inner layer (mucosa) is lined with epithelium. It contains numerous glands that secrete mucus and digestive juices. In addition to small glands, there are large glands (salivary, liver, pancreas) lying outside the digestive canal and communicating with them through their ducts. The following sections are distinguished in the digestive canal: oral cavity, pharynx, esophagus, stomach, small and large intestines.
Diagram of the digestive tract as part of the digestive system:
|
Diet
Reducing the amount of fat in the diet is recommended for patients with pancreatic insufficiency (the amount of fat in the diet should not exceed 30-40% of calories). A diet rich in fiber is not recommended for patients with chronic pancreatitis or similar diseases, as it aggravates steatorrhea, promotes the accumulation of gases in the intestines, and flatulence.
Research has shown that food allergies can contribute to pancreatic enzyme deficiency. If there is a suspicion that damage to the pancreas may be of allergic origin, special tests are carried out, and potentially allergenic products - eggs, fish, kiwi, etc. - are not used.
Replacement therapy: essential pancreatic enzymes
Pancreatin substitutes are most effective for relieving symptoms of pancreatic enzyme deficiency and normalizing digestion. Natural digestive enzymes are produced by the pancreas (pancrelipase): they are the most active and physiological, and are best tolerated.
Studies have shown that pancreatic enzyme preparations:
- Effectively improve the absorption of nutrients and eliminate the symptoms of indigestion (gurgling in the stomach, bloating, feeling of fullness, etc.);
- Remove steatorrhea;
- Slightly weaker, relieves abdominal pain caused by pancreatic insufficiency.
Preparations with enzymes that are more protected from external unfavorable factors are more active than standard ones. However, studies have not shown that drugs rich in lipase are more active than drugs with a standard dose (activity) of lipase.
Digestive enzymes produced by the pancreas (especially lipase) are chemical protein compounds with a very complex structure, therefore, their synthesis in the laboratory is not yet possible.
These pancreatic enzymes, used for replacement therapy, are extracted from the pancreas of pigs. They are the most active, safe, and do not develop tachyphylaxis.
Digestion in the mouth
The oral cavity is the initial section of the digestive tract. It is bounded above by the hard and soft palate, below by the diaphragm of the mouth, and in front and on the sides by the teeth and gums.
The ducts of three pairs of salivary glands open into the oral cavity: parotid, sublingual and submandibular. In addition to these, there is a mass of small mucous salivary glands scattered throughout the oral cavity. The secretion of the salivary glands - saliva - moistens food and participates in its chemical changes. Saliva contains only two enzymes - amylase (ptialin) and maltase, which digest carbohydrates. But since food does not remain in the oral cavity for long, the breakdown of carbohydrates does not have time to complete. Saliva also contains mucin (a mucous substance) and lysozyme, which has bactericidal properties. The composition and quantity of saliva may vary depending on the physical properties of the food. During the day, a person secretes from 600 to 150 ml of saliva.
In the oral cavity, an adult has 32 teeth, 16 in each jaw. They grab food, bite it off and chew it.
Teeth consist of a special substance called dentin, which is a modification of bone tissue and has greater strength. The outside of the teeth is covered with enamel. Inside the tooth there is a cavity filled with loose connective tissue containing nerves and blood vessels.
Most of the oral cavity is occupied by the tongue, which is a muscular organ covered with mucous membrane. It is distinguished by the top, root, body and back, on which taste buds are located. The tongue is the organ of taste and speech. With its help, food is mixed during chewing and pushed through when swallowing.
Food prepared in the oral cavity is swallowed. Swallowing is a complex movement that involves the muscles of the tongue and pharynx. During swallowing, the soft palate rises and blocks the food from entering the nasal cavity. At this time, the epiglottis closes the entrance to the larynx. The bolus of food enters the pharynx, the upper part of the digestive canal. It is a tube, the inner surface of which is lined with mucous membrane. Through the pharynx, food enters the esophagus.
The esophagus is a tube about 25 cm long, which is a direct continuation of the pharynx. No food changes occur in the esophagus, since digestive juices are not secreted in it. It serves to carry food into the stomach. The movement of the food bolus through the pharynx and esophagus occurs as a result of contraction of the muscles of these sections.