Causes
The main causes of esophageal stenosis are the following factors:
- embryonic malformation of the esophagus;
- disease of any organ of the digestive system;
- cicatricial ulcers, in particular, provoke the occurrence of cicatricial stenosis of the esophagus;
- toxicosis during pregnancy;
- anorexia;
- bulimia;
- severe infectious diseases;
- tuberculosis;
- scarlet fever;
- syphilis;
- esophageal injuries;
- radiation therapy;
- the occurrence of benign tumors;
- esophageal carcinoma;
- compression of the esophagus by enlarged lymph nodes, tumors, etc.
Preventive actions
Doctors make the following recommendations:
- Proper and correct treatment of diseases that can lead to the formation of Schatzki rings
- Avoid contact with aggressive liquids - acids, alkalis, and other dangerous compounds.
- After surgery or bougienage of the esophagus, conduct x-ray examinations regularly. The following frequency is shown: 30 days after surgery, 90 days, and then once every 6 months.
Symptoms of esophageal stenosis
Symptoms of esophageal stenosis look like this:
- frequent regurgitation of the newborn;
- excessive salivation in the child;
- discharge of mucus from the nose in a newborn;
- swallowing dysfunction (dysphagia) in a child;
- chest pain in an adult;
- vomit;
- attacks of coughing or choking;
- excessive regurgitation after every meal;
- pain in the esophagus;
- aspiration pneumonia;
- tumors in the area of the stricture;
- spontaneous or traumatic ruptures of the esophagus.
If you experience similar symptoms, consult your doctor
. It is easier to prevent a disease than to deal with the consequences.
Postoperative period, rules for patients
One-time volume of food is 150 - 200 ml.
For 5 days after the intervention, eating and drinking through the mouth is prohibited. Nutrient mixtures are given through a nasal tube.
Additionally, intravenous nutrition is indicated. Patients are injected with a solution of glucose, sodium chloride, and blood plasma.
On the 6th day you are allowed to take liquids - sweet tea, decoctions of medicinal herbs, kefir. A single volume of food should not exceed 150–200 ml. From day 8, food intake should be increased. Patients are not recommended to consume sweets, full-fat milk, carbonated water, raw vegetables and fruits. Pureed, low-fat and non-spicy foods are indicated.
Dishes should not irritate the esophagus and stomach.
Diagnostics
Diagnosis of esophageal stenosis involves taking the following measures:
- examination by a gastroenterologist
; - examination of the newborn by a pediatrician
; - endoscopic examination of the digestive system;
- X-ray examination
of the digestive system; - esophagoscopy;
- endoscopic biopsy to identify ulcerative and tumor formations.
The main task of a specialist when diagnosing esophageal stenosis is to exclude pharyngitis, the presence of foreign bodies in the esophagus or esophageal diverticula, which are similar in symptoms to the described disease.
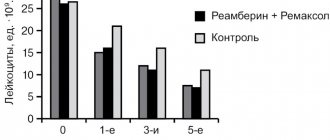
Reflection of the disease in the picture of laboratory data and ECG
In a general blood test, anemia (normochromic or hypochromic) may be observed. This is due to the depletion of the body’s intake of various nutrients and valuable substances, especially iron. The number of red blood cells increases when repeated vomiting occurs and the body becomes dehydrated. Dehydration also causes the blood to thicken. This increases hemoglobin and may increase ESR.
In the biochemical blood test, the content of protein and albumin was reduced. Repeated vomiting also shows signs of dehydration. We are talking about electrolyte disturbances: hyponatremia, hypochloremia, hypokalemia, hypocalcemia. Sometimes the amount of iron decreases. Hypochloremia leads to an increase in urea levels in the blood.
According to the ECG results, changes in the myocardium of a diffuse nature are observed: the amplitude of the T wave in several leads decreases. If the electrolyte composition of the blood is disturbed, this will be reflected in the ECG accordingly. If hypocalcemia is present, there will be a prolongation of the electrical systole of the ventricles - the QT interval, sometimes a shortening of the PQ interval and a decrease in the amplitude of the T wave.
Hypokalemia gives a decreasing amplitude of the T wave or shows the formation of a biphasic (±) or negative asymmetrical T wave. An increase in the amplitude of the U wave can also be observed. Sometimes there is a lengthening of the electrical systole of the ventricles - the QT interval; The ST segment moves horizontally below the isoline.
Digestive system, how does it work? Watch the video:
Treatment of esophageal stenosis
Treatment of esophageal stenosis involves the following manipulations:
- regular visits to a gastroenterologist
; - a gentle diet, including the consumption of liquid and semi-liquid foods;
- taking antacids and astringents;
- bougienage;
- balloon dilatation;
- endoscopic dissection with electrosurgical instruments in the treatment of cicatricial stenosis of the esophagus;
- endoprosthesis replacement of the esophagus by installing a self-expanding stent into its lumen;
- resection of the narrowing area;
- esophagoplasty (replacement of the resected area with gastric or intestinal grafts);
- gastrostomy aimed at providing enteral nutrition.
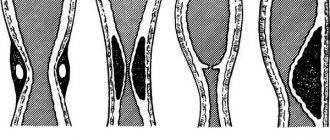
The history of the development of palliative treatment of cancer patients with tumor strictures of the esophagus goes back more than 50 years. To eliminate dysphagia, at first they tried to use various cylindrical structures: from silver wire, latex, specially treated animal fangs, rubber, polyethylene, polyvinyl chloride, organosilicon compounds, etc. In the 70-80s, methods of recanalization of the tumor-affected esophagus came to the fore: balloon dilatation, bougienage, electrocoagulation, argon-directed coagulation, Nd:YAG laser destruction, brachytherapy, ethanol injection into the tumor, etc. Since the early 80s of the last century, the method of photodynamic therapy (PDT) has been successfully used for stenosing esophageal cancer.
In this paper, we present 15 years of experience in endoscopic treatment of patients with malignant esophageal strictures in the clinic of the Moscow Research Oncological Institute named after. P.A. Herzen.
The main cause of the development of malignant stricture of the esophagus is primary locally advanced esophageal cancer, which ranks 16th in the structure of oncological diseases. Every year in Russia, 7700–7800 patients with esophageal cancer are diagnosed, while early stages are diagnosed in only 5% of patients (V.M. Kukharenko, 2000). Most often the disease is diagnosed after 50 years. The proportion of patients with advanced stage esophageal cancer is 60-70%.
For incurable patients with common forms of stenosing esophageal cancer, complicated by dysphagia and/or the formation of an esophageal-bronchial fistula, gastrostomy has been the main method of palliative care for many years. However, this method significantly worsens the quality of life, causes additional psychological trauma, and deprives patients of the opportunity to naturally eat. Recently, various options for endoscopic recanalization of the lumen of the esophagus and prosthetics have become widespread, allowing to eliminate dysphagia and restore the natural way of eating.
Indications for recanalization and prosthetic replacement of the esophagus are:
- stenosing cancer of the esophagus or cardia with grade II-IV dysphagia (preparatory stage for chemoradiotherapy or surgical treatment, and in incurable patients - as an independent method of palliative treatment, alternative to gastrostomy);
- esophageal cancer or lung cancer with the formation of esophageal-tracheal or esophageal-bronchial fistula;
- malignant tumors and metastatic lesions of the mediastinal organs with secondary lesions and stenosis of the esophagus;
- recurrence of stomach cancer (after gastrectomy) with the development of a malignant stricture in the area of the esophageal-intestinal anastomosis.
Methods of endoscopic surgery and prosthetics
Patients with inoperable stenotic forms of esophageal cancer in most cases suffer from various concomitant diseases, the severity of which increases against the background of malnutrition and dehydration. In this regard, preparing patients for endoscopic treatment should include correction of dysfunctions of the cardiovascular system, water and electrolyte balance, protein and energy deficiency using parenteral nutrition.
Before and during endoscopic intervention on the esophagus, depending on its complexity and duration, in addition to local anesthesia, it is advisable to enhance the anesthetic effect with a combination of small doses of hypnotics and analgesics (diprivan, etc.) in sub-narcotic doses. In the postoperative period, the use of analgesic drugs is indicated for 2-3 days to relieve pain.
Endoscopic treatment of stenotic esophageal cancer To recanalize the lumen in stenotic esophageal cancer, we use antegrade and retrograde electrocoagulation, argon-directed coagulation and laser tumor destruction. In recent years, the advantage remains with electrocoagulation.
The antegrade method of recanalization is used for tumors up to 5 cm in length with partial obstruction of the lumen of the esophagus. In these cases, tumor destruction is carried out in the direction from the proximal to the distal edge. In such patients, with an exophytic form of tumor growth affecting one wall (no more than 1/2 of the lumen) of the esophagus, preference is given to electroresection and Nd:YAG laser destruction.
With the retrograde method of esophageal recanalization, electrocoagulation is carried out using an electric probe, “hot” forceps or argon-directed coagulation. The operation begins from the distal edge of the tumor with gradual movement in the proximal direction. If it is impossible to pass an electric probe or light guide to the distal edge of the tumor, bougienage is performed before the tumor destruction session: using an endoscope, a guide string is passed behind the tumor, after removing the endoscope along the string, bougies are sequentially inserted into the narrowed section of the esophagus, increasing their diameter. After removing the bougies, additional electrolaser destruction of the tumor is performed. We consider preliminary bougienage of the esophagus to be a mandatory procedure before using Nd:YAG laser destruction.
PDT for stenotic esophageal cancer is used both independently and after preliminary electrolaser destruction of the exophytic component of the tumor and reducing the degree of stenosis. Photoheme (2.5-3.0 mg/kg), photosens (0.5 mg/kg), and radachlorin (1.2 mg/kg) are used as photosensitizers. The diffuser for laser irradiation during PDT is passed through the narrowed section of the esophagus and placed at the distal edge of the tumor. After this, sequential irradiation with light of a certain wavelength (for photohem - 630 nm; photosens - 670 nm; radachlorin - 662 nm) is carried out to the area of the tumor lesion of the esophagus throughout its entire length by moving the light guide in the proximal direction. Calculation of energy, light dose, number of positions and irradiation time is performed individually in each case, depending on the type of photosensitizer, the nature of tumor growth, the degree of stenosis, etc.
Endoprosthesis replacement of the esophagus is carried out to prevent restenosis after the first stage of recanalization.
In the first years (1987-1994) of mastering the method of endoscopic surgery of the esophagus, our institute used prostheses (Russia) made of medical silicone rubber with a fixing device and a cone-shaped funnel at the proximal end. However, they have a number of disadvantages: fixed diameter, insufficient elasticity, complex installation technique in the esophagus, severe and prolonged postoperative pain syndrome.
Currently, we give preference to self-expanding endoprostheses (Z-stents) (81 patients), which we have been using since 1999. 2 stents were installed in the lumen of the esophagus in 5 patients. In 14 of 81 patients, only bougienage or balloon dilatation was used as a preparatory step before stenting. In the remaining 83% of cases, one of the methods of electrolaser or photodynamic recanalization of the lumen of the esophagus was used. After installation of the stent and stabilization of the general condition of the patient, 30 patients underwent multi-course PDT with light exposure to the esophageal tumor through the transparent polyethylene wall of the stent. The average life expectancy of patients after single or multiple recanalization was 8 months.
After recanalization and installation of an esophageal stent, the patient was able to eat almost any food from the first day. All patients showed improvement in their general condition, stabilization and restoration of normal body weight. The life expectancy of patients after recanalization and prosthetic replacement of the esophagus was: up to 1 year in 44 patients, from 1 year to 2 years in 23, from 2 to 3 years in 14. The maximum life expectancy of a patient with prosthetic esophagus was 20 months.
Of the complications associated with recanalization and stenting of the esophagus, in all cases there was pain behind the sternum of varying intensity in the first 7-15 days after stent installation. The intensity of pain depended on the extent and degree of initial stenosis of the esophagus. After complete expansion of the stent within 5-7 days, the pain syndrome completely disappeared or significantly weakened; there was no need to take strong painkillers. In 2 patients, during recanalization and stent installation, partial perforation of the esophageal wall occurred. A stent was installed at the site of perforation, and conservative treatment was prescribed. Upon further observation, no signs of mediastinitis or other complications were recorded.
Stent migration into the stomach (for cardia cancer) and small intestine (for recurrent gastric cancer after gastrectomy) was observed in 4 patients over a period of 2 weeks to 4 months. In 2 patients, the stent was re-installed; in 2 patients, the stent was removed and palliative treatment was continued in the form of multi-course recanalization of the lumen of the esophagus. In 2 patients, the stent migrated in the proximal direction. In 1 case, the stent was removed and reinstalled. In 5 patients, after 6-18 months, tumor overgrowth of the stent occurred along the proximal (4) and distal (1) edges with the development of dysphagia. In 2 patients, a second stent was installed in the area of stenosis; the remaining 2 patients underwent electrocoagulation and PDT.
In patients with locally advanced esophageal cancer, when endoprosthesis replacement was not possible, we used the technique of multi-course endoscopic recanalization with an interval of 1-1.5 months. The maximum number of endoscopic operations is 46 over 3 years of treatment.
Thus, expanding the scope of surgical endoscopy for esophageal cancer for both palliative and radical treatment (for early tumor pathology in somatically incurable patients) should be considered justified. To increase the effectiveness of therapy in incurable patients with malignant strictures of the esophagus, a combination of surgical endoscopy, PDT and prosthetics is promising.
Material taken from the magazine “Together against Cancer”, #4, 2004.