What is esophageal spasm, esophagospasm, cardiospasm?
Esophageal spasm, esophagospasm, esophageal cardiospasm is a disease characterized by episodic disruption of esophageal peristalsis and the rhythmic opening of the lower esophageal sphincter,
spastic contractions of its wall. Esophageal spasm , which refers to conditions involving impaired motor function of the esophagus, causes a delay or slowing of the antegrade movement of the bolus and/or, in some cases, retrograde movement of food. Esophageal spasm is the most common cause of dysphagia (impaired swallowing). Synonyms for esophageal spasm are “ esophagospasm ”, “ hypermotor dyskinesia of the esophagus ”, “ cardiospasm ” (meaning the cardiac part of the esophagus).
Compared to diseases of the stomach and intestines, diseases of the esophagus are rare. In a healthy person, food does not remain in the esophagus, and therefore the esophagus is less subject to various irritations. Of the diseases of the esophagus, the most common are esophageal spasms, inflammation (esophagitis, esophagitis), sometimes followed by narrowing, and esophageal cancer.
Traditional medicine recipes
As an alternative, you can use unconventional means that can help solve the problem:
- A simple recipe is to take a teaspoon of flaxseed oil on an empty stomach. The procedures are carried out daily, the oil is heated to room temperature. It is better to drink it 20-30 minutes before meals.
- Prepare a decoction of motherwort and valerian root, mix the ingredients in equal proportions, pour boiling water and leave for at least 2 hours. You can supplement the decoction with hops. This medicine will have a good sedative effect.
- Mix flax and anise seeds in equal proportions, grind them in a coffee grinder or use a blender. Pour the mixture with honey, let it stand for 2 days, stirring occasionally. The product can be consumed daily, 1 teaspoon.
- Herbal baths have good results. The procedures are carried out at home, using various herbs: mint, lemon balm, fir needles, hops. Such baths have a sedative effect and are taken before bedtime. You can replace herbal decoctions with essential oils: lavender, ylang-ylang.
Causes of esophageal spasm
As food moves through the esophagus, it contracts in waves (peristalsis). Impaired motility of the esophagus leads to its spasm. Spasms of the esophagus occur more often in young, easily excitable people with an unstable nervous system. Various nervous experiences and mental stimulation can cause spasms. We consider spasms of the esophagus as a manifestation of general neurosis. Eating in a hurry also contributes to the occurrence of spasms, since poorly chewed food, mechanically irritating the esophagus, can reflexively cause spasms. Sometimes there is a spasm of the inlet part of the stomach - at the junction of the esophagus and the stomach. This is the so-called cardiospasm.
What are the possible complications?
With a sliding hiatal hernia, the upper stomach and distal part of the esophagus can move into the chest cavity and then return to their natural position.
- However, with a large hernia, existing adhesions, or a short esophagus, fixation of the hernia is possible, and reduction becomes impossible. In the absence of quality treatment, fibrous stenosis may develop.
- With prolonged exposure to aggressive gastric contents on the esophageal mucosa, an inflammatory process develops, and the appearance of ulcerative lesions, cicatricial strictures and shortening of the esophagus is possible. Ulcers are difficult to treat and are often complicated by bleeding and perforation. With a long-standing disease, the mucous membrane that comes into contact with aggressive gastric contents is gradually rebuilt. For example, the epithelium of the distal esophagus becomes similar to the epithelium of the stomach, which is regarded as a precancerous condition.
- Entry of gastric contents into the respiratory tract leads to aspiration pneumonia.
- A sudden increase in blood pressure is possible.
- In the presence of a paraesophageal hernia, the signs may be supplemented by symptoms of intestinal obstruction, since when the esophageal hernia is strangulated, the contents of the hernial sac also become intestinal loops. This condition requires urgent assistance from a surgeon.
According to information provided by the Gastroenterological Associations of Europe and America, in the absence of treatment for hiatal hernia, the likelihood of developing esophageal cancer increases by 270% over five years.
Among the existing types of esophageal hernias, paraesophageal hernias pose a greater health hazard. Despite minor manifestations, patients are recommended to undergo surgical treatment before complications develop, since movement of most of the stomach into the chest cavity can lead to disruption of the functioning of the chest organs.
Esophageal spasm: classification, types
Gastroenterologists and reflexotherapists in Saratov divide esophageal spasm into 2 types.
1. Diffuse spasm of the esophagus, characterized by uncoordinated contractions of the esophagus along its entire length (dysphagia is observed);
2. Segmental spasm of the esophagus, characterized by contractions of the esophagus in a certain area with excessive amplitude (with this type, food passes, but the person experiences pain, and deformation of the esophagus occurs).
Why does esophageal spasm occur? Pathogenesis
Often, spasm of the esophagus occurs due to impaired motor function against the background of neurasthenia, depression, stressful situations, worries, worries, in patients with mental disorders of an organic and functional nature, as well as when spastic contractions of the esophageal wall occur as a result of pathological visceral reflexes with the mucous membrane the lining of the esophagus with its increased sensitivity due to a pathological process (esophagitis, ulcer, cancer).
Spasmodic contractions of the esophagus are possible in healthy people when eating quickly, swallowing a large piece of unchewed food, or eating spicy, dry or too hot food.
The main pathogenetic factors in the development of esophageal spasm are dystrophic changes in the intermuscular nerve plexus of the esophagus, not excluding the effect of NO-ergic receptors.
Tests and diagnostics
X-ray examination
The study reveals pathology only in 50% of cases. When a contrast agent passes through the walls of the esophagus, instead of sequential, normal peristaltic movements, simultaneous, spastic, uncoordinated contractions are recorded in various parts of the esophagus.
Thanks to X-ray contrast examination, it is possible to identify such forms of deformation of the esophagus as “corkscrew”, “rosary beads”, and also assess the quality of esophageal peristalsis. For example, with a diffuse form of esophagospasm, peristalsis becomes irregular and uneven. Unlike achalasia cardia, the passage of barium through the external esophageal sphincter during spasm is not impaired.
Fibrogastroduodenoscopy
Usually this study is difficult due to severe pain. Most often it is carried out to exclude other pathologies of the esophagus ( petic ulcers , esophagitis , GERD , etc.).
Esophagomanometry
In some patients, the results of esophageal manometry may be normal, but in some patients certain abnormalities are detected:
- reflex relaxation of the lower esophageal sphincter, its incomplete relaxation;
- thanks to episodes of normal peristalsis, it is possible to differentiate esophagospasm and achalasia ;
- the pressure in the esophagus during spastic contractions exceeds 30 mm Hg.
Endoscopic method for examining the esophagus
This method allows you to identify and determine the severity of reflux esophagitis, which is the main complication of esophageal dyskinesia. Quite often, in patients with hypotonic-hypokinetic dyskinesia, a gaping cardia is detected and reflux of stomach contents into the esophagus is observed (GER - gastro-esophageal reflux).
Most modern experts consider the endoscopic method of examination to be of little significance in identifying GERD. Against the background of gagging movements that occur during esophagoscopy, the risk of overdiagnosis often increases due to displacement of the cardiac part of the stomach.
Daily monitoring of pH in the lower third of the esophagus
If the pH value is below o, then with a high degree of probability they speak of a recorded episode of GER. The results of the study indicate the total number of refluxes lasting more than 5 minutes, the total time of the study, and the average duration of attacks.
Intraesophageal impedanceometric diagnostics
This research method is used to assess the motor function of the esophagus.
There are no pathognomonic laboratory tests that clearly indicate the disease. All tests are carried out only to identify concomitant diseases and determine etiological factors. A general blood test and biochemical analysis are required to determine the level of sugar, total protein, amylase, alkaline phosphatase, ALT, AST.
Esophageal spasm, cardiospasm: symptoms, signs
What are the symptoms of esophageal spasm ? The clinical picture of esophagospasm is characterized by dysphagia and retrosternal or epigastric pain.
More often there is intense pain , which is localized in the sternum or in the epigastric region. The pain radiates along the front surface of the chest up to the neck, into the shoulders, and into the lower jaw. The pain begins spontaneously, as well as when swallowing saliva or food, can last several hours or suddenly stop after swallowing a sip of warm liquid. The frequency of pain varies: sometimes esophageal spasms appear several times during meals, and in other cases – several times a month. There are often cases of the development of spasm of the esophagus at a time of strong emotions, excitement, and neuropsychic stress. Sometimes retrosternal pain during esophagospasm resembles pain during angina attacks. Paradoxical dysphagia may occur, in which solid food passes better than liquid food. At the end of the attack, it is often possible to regurgitate a small amount of mucus.
Esophageal spasm can last from a few seconds to many hours. In some cases, dilatation of the esophagus develops above the spastic contraction. With cardiospasm, dilatation (expansion) of the entire esophagus is sometimes observed, which may be accompanied by vomiting of eaten food. The so-called esophageal vomiting differs from gastric vomiting in that it occurs soon after eating, and the vomit consists of just eaten food and does not contain gastric juice (pepsin and hydrochloric acid). Under the influence of certain living conditions, spasms of the esophagus can periodically recur.
Diet
Diet for reflux esophagitis
- Efficacy: therapeutic effect after 14 days
- Timing: constantly
- Cost of products: 1300-1400 rubles per week
Diet for gastritis and esophagitis
- Efficacy: therapeutic effect after 14 days
- Timing: constantly
- Cost of products: 1500-1600 rubles. in Week
To improve the patient's condition, regular, split meals (4-6 times a day) are recommended. If possible, food should be mushy or liquid. It is recommended to completely avoid eating too cold or too hot food, carbonated drinks, sour juices, and coarse fiber.
How to relieve spasm of the esophagus, how to relieve esophagospasm in Saratov, Russia
At the first consultation, the doctor will tell you what esophageal spasm , what causes, signs, and symptoms are observed with esophageal spasm, how esophageal spasm is treated in Saratov, esophageal spasm treatment in Russia? Why does spasm of the esophagus occur due to nerves? How to relieve spasm of the esophagus and stomach? What to do if there is spasm of the esophagus, esophagospasm, esophagospasm of the esophagus, neurospastic spasm of the esophagus, diffuse spasm of the esophagus when swallowing in men and women, adolescents, children, how to relieve spasm of the esophagus in Saratov .
Sign up for a consultation. There are contraindications. Specialist consultation is required.
Photo: Bds | Dreamstime.com\Dreamstock.ru. The people depicted in the photo are models, do not suffer from the diseases described and/or all similarities are excluded.
Related posts:
Heartburn, burning in the stomach, treatment in Saratov, how to get rid of heartburn, what to do
Spasm of the esophagus: treatment, causes, how to relieve, treat cardiospasm of the esophagus, esophagospasm
Hepatomegaly, steatosis, fibrosis, alcoholic hepatitis, liver cirrhosis, alcohol damage
Stomach ulcer, duodenal ulcer, peptic ulcer: treatment in Saratov
Belching, treatment, frequent rotten belching of air, eggs, food
Comments ()
Survey
To make a diagnosis and carry out diagnostic procedures, you will have to consult a doctor. The following specialists can help solve the problem:
- Surgeon
- Gastroenterologist.
To differentiate the disease you will need to go through a series of examinations:
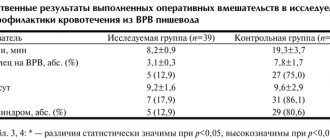
| X-ray examination of the esophagus: | Esophagography examination: |
| The examination is carried out in most cases due to its simplicity and accessibility. The image reveals an expansion or change in the organ. The esophagus, in case of severe changes, looks like a serpentine road. The problem is that in half of the cases, x-rays do not reveal any changes in patients. | Carry out with the introduction of contrast. Depending on which part of the esophagus the contrast agent has accumulated, a conclusion is made about the area of damage to the organ. The examination is effective because it helps differentiate the disease. |
As part of diagnostic procedures, it is permissible to prescribe other procedures. The doctor may also refer the patient to have tumor markers tested. The analysis will help exclude the presence of diseases of oncological origin.