Oncologist compulsory medical insurance
Ivanova
Marina Viktorovna
5 years experience
Oncologist (CHI)
Make an appointment
Gastric cancer is a malignant neoplasm that forms from the mucous epithelium and grows rapidly, spreading to other organs. The altered cells lose their original function, they only have the ability to divide uncontrollably, which leads to a rapid increase in tumor size. Metastases spread throughout the digestive tract, penetrate into the liver and lungs with the bloodstream, and into regional and distant lymph nodes with lymph.
Kinds
Up to 95% of all cases of the disease are adenocarcinomas. These tumors develop from mucosal cells that produce gastric juice. According to the histological classification of gastric cancer, there are four main types of adenocarcinomas:
- tubular - the most common mushroom-shaped neoplasms;
- papillary - characteristic of the upper part of the stomach, often metastasizing to the lymph nodes and liver;
- mucinous - mucous formations with tumor cells, accounting for about 10% of all cases of the disease;
- signet ring cells - consisting of cells with a displaced nucleus, which is why they resemble rings in shape.
About 5% of clinical cases are lymphomas, squamous cell, carcinoid and small cell tumors.
Signs before death
There are general signs that appear in a patient before dying and which characterize stage 4, when almost all organs of the body are affected by a malignant tumor:
- Chronic fatigue, sleepiness, due to the absorption of a large amount of energy and nutrients by the tumor.
- Appetite decreases against the background of general intoxication of the body due to the tumor’s production of toxic products into the blood. The body no longer needs energy and the patient does not want to eat or drink.
- Coughing attacks, heavy breathing due to damage by lung metastases.
- Disorientation. Occurs due to impaired metabolism with brain tissue and severe intoxication. Memory loss and hallucinations may occur.
- Limbs turn blue. The body tries to function somehow, but there is little strength left. As a result, blood rushes to the heart, kidneys, and brain. The limbs begin to cool, turn blue and pale.
- Spots on the arms and legs that are associated with poor circulation. Muscle weakness is a concern, movement is limited, many patients become completely bedridden.
- A comatose state that can occur unexpectedly.
Stages of dying:
In a state of preagonia, the patient's blood pressure becomes low.
- Predagonia. Malfunctions of the nervous system occur, emotions become dulled, the skin on the arms and legs turns blue, the face darkens, and blood pressure drops.
- Agony. Due to the spread of the tumor, oxygen starvation occurs with a slow heartbeat.
- Clinical death. The heart stops working and the person stops breathing.
- Biological brain death.
Death does not always come quickly. Patients can be in great pain and suffer for a long time. If there is no chance of saving a person, to reduce suffering, properly selected therapy should still be carried out, which will help to live longer and alleviate the condition. Medicine has not yet been able to treat advanced stage gastric cancer. Therefore, it is important to make a diagnosis as early as possible and begin treatment.
Symptoms
It is extremely difficult to identify the first signs of stomach cancer; the symptoms of the initial stages are often mistaken for manifestations of common gastrointestinal diseases:
- flatulence after eating;
- constant discomfort in the stomach;
- nausea with slight salivation;
- heartburn (if the tumor forms in the upper part of the stomach);
- loss of appetite and weight loss.
The listed symptoms of stomach cancer are accompanied by rapid fatigue, a constant feeling of tiredness, drowsiness, apathy, and poor health. As it grows, local signs appear, depending on the location of the tumor:
- in the upper part – difficulty swallowing food;
- in the middle section - constant salivation;
- in the lower part - a constant feeling of heaviness, belching with a putrid odor.
The patient suffers from severe abdominal pain; with gastric bleeding, vomiting “coffee grounds” is possible, i.e. dark mass, or mixed with scarlet blood.
Causes and risk factors
Currently, the main cause of stomach cancer is infection with the bacterium Helicobacter Pylori. This is the only microorganism that can survive and multiply in the acidic environment of constantly secreted gastric juice. The metabolic products of the bacteria irritate the gastric mucosa, which leads to atrophy of the glandular tissue, which degenerates into tissue resembling intestinal epithelium. If irritating factors are not eliminated, then dysplasia develops in the affected area - the cells become atypical, and in the future the process becomes malignant.
Gastroenterologists identify the following as negative factors that lead to the development of symptoms of stomach cancer:
- inherited predisposition to the development of gastric cancer;
- commitment to spicy foods, smoked meats, dried fish and meat, fatty and fried foods;
- long-term use of certain medications;
- excessive doses of radiation;
- smoking tobacco and regular alcohol consumption.
Men suffer from stomach cancer more often than women, and older people more often than young people.
Causes of stomach cancer
Cancer occurs when the number of acquired mutations in the DNA of a certain population of cells, caused by various reasons, allows them to divide uncontrollably and “hide” from the immune system.
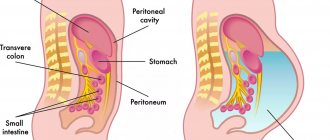
Accumulating cancer cells form a tumor that can invade nearby structures. Cancer cells can break away from the tumor and spread throughout the body. This is called metastasis.
Although the underlying cause of gastric cancer is still unclear, there is a clear understanding of risk factors and predisposing factors.
In recent years, the evidence base for the connection between stomach cancer and infection with the bacterium Helicobacter pillory, which often causes chronic gastritis and gastric ulcers, has been gaining momentum.
There is a proven link between a diet high in salty and smoked foods and cancer located in the main part (body) of the stomach. As the use of refrigeration to preserve food has increased, rates of stomach cancer have decreased worldwide.
Stages
The development of the oncological process begins with the zero stage of gastric cancer, at which dysplasia transforms into malignant cells. This stage is called cancer “in situ”, i.e. "on the spot." The neoplasm is extremely small in size and is discovered accidentally during an endoscopic examination for another disease. The process then develops in the following stages.
- Malignant cells spread throughout the mucous membrane, penetrate into the submucosal and sometimes into the muscular layer.
- The neoplasm penetrates all layers of the gastric wall, up to the outer membrane, and metastasizes to several regional lymph nodes.
- The tumor increases in size and affects up to 15 regional lymph nodes. Spread into neighboring organs is possible.
- The malignant process affects several vital organs - the heart, esophagus, lungs. Metastases penetrate to distant organs and lymph nodes.
Diagnostics
Instrumental and laboratory diagnosis of stomach cancer includes the following studies.
- Gastroscopy. An endoscopic examination allows you to examine the internal surface of the organ and take a sample of pathological tissue for analysis.
- X-ray. It is performed with a contrast agent and allows you to identify changes in the relief of the mucous membrane, a decrease in the elasticity of the gastric wall and other changes.
- Ultrasound of the abdominal cavity. The study allows us to identify metastases to other organs.
- CT scan of the stomach. Shows how far the malignant process has spread.
- Blood test for tumor markers.
- Histological examination of a biopsy to determine the type of cancer cells.
Attention!
You can receive free medical care at JSC “Medicine” (clinic of Academician Roitberg) under the program of State guarantees of compulsory medical insurance (Compulsory health insurance) and high-tech medical care.
To find out more, please call +7, or you can read more details here...
Treatment
The choice of treatment regimen for stomach cancer depends on the stage of the disease.
- Surgery is the most effective method to completely restore the patient’s health. If cancer is detected “in situ”, laparoscopic sparing intervention is performed. Abdominal surgery with partial or complete removal of the stomach is performed at the first and second stages. At the same time, the affected lymph nodes are removed.
- Chemotherapy. Potent chemotherapy drugs are prescribed before surgery to reduce the size of the tumor or after - to destroy the remains of malignant cells and avoid relapse. At the inoperable stage, it becomes the main method of treatment. As a rule, several different drugs are combined to increase effectiveness.
- Radiation therapy. This method is also used before and after surgery, and for inoperable patients it is used to reduce tumors and prolong life. Radiation treatment is often combined with the use of chemotherapy.
- Targeted therapy. Selective drugs are prescribed to inoperable patients to block certain protein receptors and stop tumor growth. These drugs are suitable for approximately 20% of patients. They do not destroy tumor cells and are used as a palliative.
- Laparocentesis. The accumulated fluid is removed from the peritoneum through a small incision.
- Symptomatic therapy. Patients experiencing severe pain are prescribed painkillers according to a special regimen.
Palliative care in the last days of a person’s life
“Those whom we ourselves accompany in the last phase of life,
teach us that
that preparation for death is the best preparation for life itself.”
The death of a palliative patient is a natural outcome of a chronic disease. The doctor’s task is not to artificially prolong the dying process, but to preserve the quality of a person’s life until the very end. Doctors must relieve painful symptoms, provide the patient with high-quality, sensitive care, and also help his loved ones cope with the loss of a loved one.
The article was prepared based on materials from a webinar by Diana Sitnikova, head of the department at the Moscow Multidisciplinary Center for Palliative Care of the Department of Health.
Why don't we provide resuscitation to palliative patients?
Resuscitation measures for a palliative patient lead to an artificial prolongation of the dying process. There is also a legislative basis for this.
Federal Law No. 323-FZ of November 21, 2011 “On the fundamentals of protecting the health of citizens of the Russian Federation” states:
Resuscitation measures are not carried out: in a state of clinical death (stopping the vital functions of the human body (blood circulation and breathing) of a potentially irreversible nature in the absence of signs of brain death) and against the background of the progression of reliably established incurable diseases or incurable consequences of acute injury that are incompatible with life.
Resuscitation. Can she help? What you need to know about resuscitation and the condition of a person in the terminal stage of illness in order to make the right decision at the end of the life of a loved one Vera Foundation
Receiving palliative care
What are the terminal states?
- Predagonia;
- Terminal pause;
- Agony;
- Clinical death;
- Biological death (more about each of them below).
What the doctor needs to do:
- Adjust patient care - make it more gentle, abandon unnecessary manipulations;
- Remove unnecessary drainages, catheters, nasogastric tubes, etc.;
- Adjust therapy, discontinue medications that will not affect the quality and length of life;
Important It is necessary to continue pain relief with possible dose titration to achieve an adequate analgesic effect until the very end!
- Discuss his condition with the patient’s loved ones and explain what to expect.
Communication with the patient's loved ones
- Tell the patient's relatives what will happen to their loved one. Point out to them that what they perceive as torment is not always so for the patient.
- Give people time to accept the inevitability of loss as much as possible.
- Remind them that it is important to have time to resolve everyday, legal and civil issues: write a will, deeds of gift, etc.
- Help people spend time with a loved one: say something unsaid, finish something.
Spiritual testament: how to convey your experience to loved onesAbout the practice of writing letters in which a person can summarize his life, give parting words and share lessons with those who will remain after his passing The GroundSwell ProjectEnd of life
What can be done for the patient?
If a person is in a hospital, if possible, transfer him to a separate room and provide comfortable conditions. If the person is religious, offer to invite a clergy member and arrange for the visit if the patient agrees.
Organize an individual nursing station.
A person should not leave alone, even if he is already unconscious. One of the junior or nursing staff must be with the patient at all times.
Don't involve volunteers or interns in this - they may not be competent at this. The person nearby should have time to notice changes in the patient’s condition and inform the doctor about it in time.
Learn more about each phase of dying
Predagonia
Predagonia is characterized by severe circulatory and respiratory disorders, which lead to hypoxia. In the central nervous system at this moment, the process of inhibition predominates, the electrical activity of the cerebral cortex fades away.
Predagonia can last from 1 day to 1 month. The duration depends on the rate of progression of the underlying disease, the age of the patient and the initial resources of the body.
Symptoms of preagonia:
- Tendency to hypotension, hemodynamic disturbances;
- First tachycardia, tachypnea - then bradycardia and bradypnea;
- Progressive depression of the level of consciousness. From lucidity to coma;
- Increased hypoxia;
- If the patient is conscious, there is a gradual decrease in appetite;
- Oliguria, changes in the skin;
- Cyanosis, marbling of the skin;
- Hyperthermia.
Practical recommendations for the treatment of painful symptoms To help medical specialists, we have prepared practical recommendations for the treatment of the most common painful symptoms and conditions in palliative practice: nausea and vomiting, shortness of breath, constipation, itching, hiccups, anorexia and cachexia.
What should you do during this period?
First, hydration therapy (infusions or enteral nutrition) should be gradually reduced. If the life expectancy is several hours, stop completely. This should be done if the patient is already unconscious.
Important All actions must be coordinated with the patient’s relatives.
Continue symptomatic therapy - if there are any painful symptoms, including pain, continue to relieve them.
If the patient is at home, the question of hospitalization is raised in the following cases:
- If a person has pain or convulsive syndrome that cannot be controlled at home;
- Delirium requiring medical sedation;
- Obvious defects in care;
- If relatives are physically unable to care for a person in serious condition;
- If hospitalization is requested by the patient himself or his relatives who are not ready for the person to leave at home.
In this phase, we try to choose the least invasive method of administering drugs to the patient. Most often this is the buccal method. If the patient is still swallowing, tablet forms can be continued. The drugs can also be administered transdermally. You should switch to subcutaneous or intravenous injections only if necessary - with complete depression of consciousness and absence of swallowing. We try to avoid the intramuscular method, as it is the most painful.
Terminal pause
This phase is often difficult to identify. The terminal pause is characterized by:
- Sudden stoppage of breathing;
- Consciousness is completely absent;
- Peripheral reflexes are significantly reduced or completely absent;
- Muscle tone is minimal;
- A complete cessation of cardiac activity is possible.
Most often, the terminal pause ends in clinical death, bypassing all subsequent phases.
Agony
During this period, maximum activation of the body's resources to support life occurs. Against the background of pronounced inhibition of the cerebral cortex, strong excitation of the bulbar centers occurs.
The duration of agony depends on the type and mechanism of death, as well as on the adaptive capabilities of the body. It can last from several minutes to several hours, and sometimes be absent altogether.
Dr. Elisabeth Kübler-Ross. From the book “In the Middle of Life” The author of the concept of the five stages of grief, she saw the horrors of war, became a doctor at 31 and devoted her life to caring for the terminally ill Editors
About palliative care
Signs of agony:
- There is no consciousness;
- Terminal (agonal) breathing;
- Decreased pupillary response to light, no pharyngeal or corneal reflex;
- Muscle tone is reduced, but there may be decerebrate muscle rigidity;
- Convulsions;
- Hyperthermia or hypothermia;
- Hemodynamic disturbances;
- The pulse can only be felt in the carotid arteries;
- Discharge of biological vomiting and discharge of feces and urine;
- Tendon reflexes are absent;
- Maximum activation of the body’s vital forces is possible (this happens rarely);
- Lazarus syndrome, when flexion movements appear in the trunk and limbs, and the patient seems to sit down, raising his hands to his face - the so-called “boxer pose” (this happens extremely rarely).
At the end of the agony, manifestations of neuro-reflex activity completely disappear.
What should you do during this period?
Continue taking opioid analgesics. However, if the patient is unconscious, if there are no signs of pain and, in all likelihood, the end of life is a matter of minutes, then all interventions should be stopped. The same applies to positioning a person in bed - there is no need to turn him. The risk of developing bedsores is no longer important.
Important There should be a minimum of interventions at this stage! We leave only moisturizing of the mucous membranes, oral cavity, lips, conjunctiva.
Clinical death
The main signs of clinical death:
- Lack of consciousness;
- Lack of spontaneous breathing;
- Absence of pulse in the main arteries;
- Wide pupils;
- Lack of pupillary response to light and corneal reflex;
- Paleness, cyanosis of the skin.
Biological death
It is characterized by irreversible changes in all organs and systems that are permanent, cadaveric in nature.
A morgue is a civilized place. An interview with forensic expert Olga Fateeva about how a morgue works, what happens to a person’s body after death, why the deceased may be completely different from his living self, and whether embalming is always necessary Evgeniya Rezvan
End of life
Features:
- Early - drying and clouding of the cornea, a symptom of "cat's eye".
- Late - cadaveric spots and rigor mortis.
Practical advice
After declaring death, the doctor’s diary must indicate:
- – pallor and cyanosis of the skin;
- – lack of consciousness;
- – lack of breathing;
- – absence of pulse;
- – lack of reaction of the pupils to light;
- – absence of corneal reflex.
The exact date and time of death is also indicated.
What to do with painful symptoms in terminal conditions
Asthenization
Make sure the person is in a comfortable position in bed. Turn and move it less. You can massage before and after turns, especially in problem areas (such as bony prominences).
Important:
do not force the patient to do more than he wants or is able to do. Turns every two hours are no longer relevant. Absorbent underwear should be changed only when necessary: if the patient does not urinate, then there is no need to do this.
Depressed level of consciousness
The depression of consciousness can be gradual or, conversely, abrupt. May begin with increased sleepiness and difficulty waking up. The patient may have no initial reactions to verbal and tactile stimuli. Speech function deteriorates: the patient finds it increasingly difficult to find words, he gives monosyllabic, slow, sometimes inadequate answers, which he thinks about for a long time. Speech may also be completely absent.
What to do?
- Even if it seems that the patient does not hear or understand the spoken speech, you still need to warn about all your actions, speak calmly and quietly, and do not rush into answers.
- If the person does not seem to recognize anyone, we still talk to him as if he were a capable person.
- Continue pain therapy if we are 100% sure that it is not the cause of depression of consciousness.
- If the patient is unconscious, do not discuss the diagnosis or prognosis in front of him. Also don't do it if he doesn't want to talk about it.
- Do not talk about the patient in the third person.
- Avoid excessive activation, do not disturb the person, giving time to rest.
Palliative sedation: regulatory, ethical and clinical aspectsWhen is palliative sedation needed, is it necessary to obtain the patient’s consent and what moral problems will one have to face Diana Nevzorova Tatyana GremyakovaPain management at the end of life
What do relatives often ask?
Question: Why does he sleep all the time?
Variant answer: The patient does not have the strength to talk or stay awake due to increasing intoxication. If you imagine very severe poisoning, multiplied by a hundred times, this is what your relative is experiencing now. All the forces of his body are aimed at maintaining the central functions of the body: breathing, heart function. Sleep is a defensive reaction.
Question: Is it from the drugs you give him?
Possible answer: If this were a side effect of narcotic analgesics, it would appear during the initial intake or after increasing the dose. If this does not happen, then most likely the patient’s condition is associated with the manifestation of the underlying disease.
Hemodynamic disorders
Tachycardia, hypertension followed by hypotension, peripheral cooling, cyanosis, marbling of the skin.
What to do?
- If the patient feels weak due to a decrease in blood pressure, administer glucocorticosteroids (if there are no contraindications).
- Warm with a heating pad, always wrapped in a cloth or towel.
- Give a light massage if you feel chilly.
Under no circumstances should you carry out massive infusion therapy or administer vasopressors, as this is an artificial prolongation of life!
What do relatives often ask?
Question: Why are my hands and feet cold and cyanotic?
Variant answer: There is a redistribution of blood flow and centralization of blood circulation: the main blood flow is directed to the heart and brain, and less blood flows to the periphery (to the legs and arms).
Question: Why don’t you increase your blood pressure with medications?
Variant answer: At the moment, a decrease in blood pressure does not lead to worsening of the condition and death, but is a sign that the person is leaving. If we increase the pressure, we will artificially prolong his agony and, most importantly, his suffering.
Terminal breathing
There are several types of terminal breathing. The most common are those associated with an imbalance between excitation and inhibition in the central nervous system. The most common: Cheyne-Stokes, Biot, Grock or Kussmaul breathing.
What can you do about it?
- Give the person a comfortable position. Typically this means raising the head end of the bed.
- Continue to care for your oral cavity - moisturize the mucous membranes. With pathological breathing, the mouth is open, which means the mucous membranes dry out.
- Continue with previously prescribed opioid analgesics. Perhaps with dose titration.
- If you have previously started low-flow oxygen therapy, you can continue it. Under no circumstances stop it in the presence of relatives! Only if we could convince them that this was no longer necessary.
Death rattle
This painful symptom often worries the patient’s loved ones. It no longer bothers the person himself. It can be combated by administering moderate doses of M-anticholinergic drugs, for example, atropine. Or simply by turning the patient's head to the side. Mechanical ventilation should not be prescribed unless it has already been started (except in patients with ALS).
Palliative care for patients with ALS Breathing and swallowing disorders, communication difficulties and other symptoms in amyotrophic lateral sclerosis Vadim Parshikov
Symptomatic treatment
What do relatives often ask?
Question: Why did breathing change?
Variant answer: Our breathing is regulated by the respiratory center, which is now in a state of hypoxia. This can cause breathing to become irregular. This is a natural process.
Question: Why does the patient wheeze? Perhaps he is suffocating?
Variant answer: The sound is associated with impaired evacuation of bronchopulmonary secretions. The person cannot cough it up, and it seems that he is choking. This is not so: in fact, the person does not feel it, and he does not have the need to clear his throat.
Question: Do something, he’s suffering!
Variant answer: We understand how difficult it is to look at a loved one in such a state, but, believe me, the person himself no longer experiences suffering.
Lack of appetite and gradual decrease in fluid intake
What can be done?
- Give the patient small, frequent sips of water.
- If this is not possible, or the patient refuses by clenching his teeth (sometimes this is the only way for a person to show that he does not want to do this), try to irrigate the oral cavity with water or special gels such as artificial saliva.
- If, on the contrary, a person wants to eat, clarify his taste preferences. Someone wants champagne, someone wants red caviar - on their deathbed, everything is possible.
- When fluid intake is reduced, subcutaneous administration of saline is an option. We are always afraid of dehydration, since this can cause a deterioration of the condition - depression of consciousness, the development of delirium, constipation, etc.
Important: Do not force feed the patient under any circumstances!
Parenteral and enteral nutrition is contraindicated for patients in terminal conditions. This will not help anything and will not prolong life.
A nasogastric tube is placed if the prognosis for survival is several weeks. Installation of a gastrostomy tube is indicated if the life expectancy is at least 6 months.
Nasogastric tube: placement, feeding rules, prevention of complications Technique for placing the tube, possible complications and their prevention Varvara Brusnitsyna
Symptomatic treatment
What do relatives often ask?
Question: A person is dying of hunger, why does he refuse food?
Possible answer: Loss of appetite at this stage is normal and natural. All body functions are slowed down, so less energy is needed. The man is not hungry. If he wanted, he would eat. We cannot force him.
Question: Why is enteral nutrition not prescribed?
Variant answer: The body no longer has the energy resources to digest and assimilate food, the gastrointestinal tract is not able to extract nutrients. Blood circulation is aimed only at maintaining the functioning of the heart and brain. Enteral nutrition in this phase will not give anything.
Pain management at the end of life
- Continue pain management based on the severity of the person's condition. Opioids should not be discontinued if confusion or unconsciousness occurs. Rate pain using the PAINAD scale.
- If the patient can no longer speak, assess his pain behavior.
- If there is no swallowing, the patient should be switched to injectable forms of analgesics in an equivalent dosage.
Important In a number of patients in the terminal phase, pain becomes refractory and cannot be effectively treated. In this case, opioids are used in invasive forms in the form of prolonged subcutaneous or intravenous infusion. Their use is possible only in a hospital setting.
In some cases, with refractory pain, additional drug sedation is possible.
Delirium, agitation, increased anxiety
First, find out the cause of the agitation. It may be associated with unmet physical needs - unrelieved pain, bladder or bowel fullness.
If it is not possible to find out, the patient should be preventively anesthetized. That is, exclude pain as a possible cause.
It is necessary to show the patient that the doctor is his ally. Speak calmly and confidently. Do not object or argue with the patient. If this does not help, you should resort to drug treatment: haloperidol intramuscularly, if this does not help, aminazine.
Confusion, disorientation, anxiety - how to help? Sometimes terminally ill patients become agitated, cannot calm down, can get confused in time and space, and see people and things that are not there. What can be done for them? Vera Foundation
End of life
What do relatives often ask?
Question: Can a person in such a state harm himself?
Variant answer: In this condition the patient is already too weak. Most likely, he simply does not have enough strength for this. In addition, we will not allow him to be left alone, and we will install an individual nursing station in the ward.
Question: Why is this happening, why does he behave this way?
Variant answer: This condition is not a manifestation of a mental illness, but a consequence of dysfunction of internal organs, endogenous intoxication.
Question: Can he be calmed down?
Possible answer: Yes, but the patient may become drowsy and difficult to contact.
Ethical and psychological aspects of accompanying the patient and his family in the last hours of life
What should the doctor do before the patient reaches a terminal condition?
- Understand which of your loved ones will be with the patient and will participate in decision-making.
- Assess the extent to which the patient himself is aware of the approach of death: his speech and communication characteristics should be taken into account.
- Find out what the patient wants to know about his diagnosis and life prognosis. Ideally, find out where the person wants to die. There are people who fundamentally want to die at home. It is better to know about this in advance in order to provide transportation, painkillers, and organize visits from the patronage service - that is, arrange hospice at home.
By the way, the British palliative care doctor Bruce Cleminson said that information about the diagnosis belongs, first of all, to the patient. Read it!
In the last hours of a person’s life, his loved ones also need help. Talk to them, explain in advance what they can expect, discuss their fears and concerns.
After a person's death, their loved ones still need help. After all, this is only the beginning of their grief journey. In the Palliative Care Center of the Moscow Health Department, we can offer a consultation with a psychologist and provide the necessary literature. Usually people are confused, they need to clearly explain further actions, because they still have a lot of work to do.
After pronouncing death
- Notify a relative of the death if they were not present.
- Offer a farewell in a comfortable, private setting - only if the relative wants it (some people don’t want this on principle, because it’s morally difficult for them). Explain that there will be an opportunity to say goodbye at the morgue.
- Get ready to have to explain everything to your relatives several times.
- Provide relatives with information brochures to help them understand their next steps.
- Try to complete the documentation quickly. This determines how soon the body will be sent to the morgue and the funeral will take place. This can be very important for the patient's loved ones.
The material was prepared using a grant from the President of the Russian Federation provided by the Presidential Grants Foundation.
Stock image used from Depositphotos.
Diagnosis and treatment of stomach cancer in Moscow
If you need high-quality and accurate diagnosis when symptoms of stomach cancer appear, contact the Medicina clinic. For our patients:
- the most modern diagnostic medical equipment;
- well-equipped in-house laboratory;
- oncologists and gastroenterologists of the highest category;
- comfortable hospital rooms for the treatment of stomach cancer.
Call us to get detailed answers to all your questions.
Recommendations from doctors at the Rassvet clinic for the prevention of stomach cancer
It remains unclear exactly what the key factor causes gastroesophageal cancer or gastric body cancer, so it cannot be prevented. But you can take steps to reduce the risk of developing this terrible disease.
To do this, you need to make small changes in your daily life:
- Control your weight. If you have signs of obesity, consult a dietitian about changing your eating behavior.
- Try to be physically active most days of the week. Regular exercise is associated with a reduced risk of stomach cancer.
- Eat more fruits and vegetables. Try to add more fruits and vegetables to your diet daily. Not only quantity is important, but also variety; it has been proven that eating 5 or more types of vegetables and/or fruits per day significantly reduces the risk of stomach cancer.
- Reduce your consumption of salty and smoked foods.
- Stop smoking. If you smoke, quit. If you don't smoke, don't start. Smoking increases the risk of not only stomach cancer, but also many other types of cancer. Quitting smoking on your own can be very difficult, you can contact the doctors at the Rassvet clinic, they will provide you with practical advice and information about existing medications to make it easier to quit smoking.
Questions and answers
How to recognize stomach cancer in the early stages?
In addition to the specific “stomach” signs of illness - flatulence, stomach discomfort, the patient develops inexplicable weakness and a sharp decrease in performance. One of the rather striking signs is an aversion to protein foods. If these symptoms appear, you need to undergo a gastroscopic examination without wasting time.
Is there a cure for stomach cancer?
The main danger of the disease is that the symptoms of stomach cancer in the early stages are often mistaken for a common disorder and people are in no hurry to consult a gastroenterologist. Even in countries with highly developed medicine, the disease is most often detected at the fourth, inoperable stage. Therefore, if warning signs appear, it is imperative to undergo a screening examination.
What kind of pain is felt with stomach cancer?
Pain sensations depend on the size of the tumor and its growth into other organs. The neoplasm grows slowly, from the moment the first malignant cells appear until the formation of a tumor measuring about 2 mm takes at least two, and more often about five years. All this time there are no symptoms of stomach cancer. Severe and constant pain appears already in the last, advanced stages of the disease.
Attention! You can cure this disease for free and receive medical care at JSC "Medicine" (clinic of Academician Roitberg) under the State Guarantees program of Compulsory Medical Insurance (Compulsory Medical Insurance) and High-Tech Medical Care. To find out more, please call +7(495) 775-73-60, or on the VMP page for compulsory medical insurance
Prognosis for cure
The likelihood of recovery increases if the tumor was detected in the early stages of the disease. Other factors also influence a positive result. Thus, cancer of the 1st and 2nd degrees is not cured in all cases due to the increased aggressiveness of malignant tissues, which accelerate the growth process of the cancerous tumor.
The patient's apathy contributes to his rapid decline.
The highest mortality rate is at stage 4. One case out of 100 is that stomach cancer is diagnosed at the very beginning of the disease. People die quickly from this disease, in most cases not even six months after diagnosis. The reason for this is the rapid progress of the pathology and the apathetic state of the patient. Five-year survival rate at stage 1 is 80%, at 2-56%, 3-38%, at the last stage - 5%. The chances in this case increase if the patient has not died after 2 years.
Using statistics, it is impossible to predict what will happen to a person with stomach cancer, including due to the different rates of cancer spread. There are also other individual factors that influence treatment. For example, good health before being affected by disease.