GASTRECTOMY
(Greek gaster stomach + Greek ektome excision, removal; synonym
gastric extirpation
) - operation of complete removal of the stomach. One of the methods of surgical treatment of malignant tumors of the stomach, it is used much less frequently for some other diseases (polyposis, high-lying ulcer, Zollinger-Ellison syndrome).
The first successful G. was produced in 1897 by a Swiss. surgeon Schlatter (S. Schlatter). The operation was completed by performing an esophageal-small intestinal anastomosis. In 1898, Brigham and McDonald (S.V. Brigham, R.M. McDonald) reported successful G. with esophageal-duodenal anastomosis. In Russia, the first gastric extirpation for cancer with a favorable outcome was performed by
V. M. Zykov in 1911. The technical complexity of the operation was the reason for its very slow introduction into surgical practice. Thus, N.P. Trinkler (1911) provides summary statistics of 25 cases of G., of which only 13 were successful. By 1933, information about 165 operations performed by 55 surgeons (mortality rate 63%) had been published in the world literature. In the 40s and 50s of the 20th century. The surgical technique was developed in detail, and numerous options were proposed. G. has become widespread and has become a routine surgical intervention in large surgical institutions.
Fig 1. Scheme of restoring the continuity of the digestive tract after gastrectomy: a - esophagojejunostomy; b — esophagoduodenostomy; 1 - esophagus; 2 - diaphragm; 3 - jejunum; 4 - duodenum.
The most common method of reconstruction for G. is the simplest - esophagojejunostomy with Brownian anastomosis (Fig. 1, a). Other modifications of G. are used less frequently, for certain indications.
A number of techniques have been proposed to ensure the creation of an artificial reservoir at the site of the removed stomach using lateral anastomoses. To prevent reflux of intestinal contents along the afferent loop, Roux-en-Y anastomoses were used. Much attention was paid to the development of modifications of surgical intervention that allow, after G., to maintain the passage of food through the duodenum (esophagogoduodenostomy - Fig. 1.6). However, due to the anatomical features of the esophagus and duodenum, this operation can only be used in a limited number of cases.
After the development of methods of intestinal plastic surgery, replacement of the removed stomach with a section of the small intestine began to be used during operations on the stomach, and the restoration of passage through the duodenum was often combined with the simultaneous creation of voluminous reservoirs. A number of technical proposals [operations by A. E. Zakharov, A. M. Betaneli, Pot (EJ Poth)] were caused by the desire to slow down the passage through the small intestinal segment transplanted to the place of the stomach; For this purpose, Nissen, Sperling (R. Nissen, E. Sperling) and others suggested leaving the gatekeeper unremoted. Restoration of passage through the duodenum in some modifications of G. is achieved by transplantation of segments of the colon. Many of the listed surgical interventions are highly technically complex and traumatic), which prevents surgeons from widely using them for cancer patients.
Indications
G. is performed for cancer of the body of the stomach or its upper third, as well as for tumors that spread to most of the organ. For localized tumors of the cardial part of the stomach, in some cases, resection of the proximal part is justified - an operation that has functional advantages over G. The vast majority of modern surgeons have a negative attitude towards the idea of performing G. according to fundamental indications, that is, for any localization of gastric cancer, as this at one time they were proposed by K. P. Sapozhkov (1946), Scott and Longmire (H. Scott, W, Longmire, 1949), Lahey (F. Lahey, 1950) and DR.
The surgeon makes the final decision on the possibility of radical removal of the stomach tumor and the extent of the operation only during the intervention itself, when the limits of spread and the nature of tumor growth (exophytic, endophytic), and the presence of metastases in the lymph nodes are clarified. Every surgeon operating on the stomach for malignant tumors should always be prepared for G.
Of great practical importance is the question of indications for the so-called. combined G., when the organ to which the tumor spreads (transverse colon, spleen, pancreas, liver) is partially or completely removed along with the stomach. The solution to this issue depends on the data of the clinical and radiological examination, as well as on surgical findings. Experience shows that combined operations are justified only in cases where the growth of a stomach tumor into adjacent organs is limited or there is a limited increase in lymph nodes, for example, in the hilum of the spleen. Such operations become futile with multiple metastases.
Contraindications
consist of contraindications of an oncological nature (spread of the tumor to nearby organs, metastasis beyond the regional lymphatic basins, distant metastases) and general contraindications (high degree of surgical risk in elderly patients with concomitant diseases).
Preoperative preparation
should be carried out taking into account the specific features identified as a result of the clinical trial, and should be limited, if possible, to short periods (7-10 days). The issue of rational preoperative preparation should be decided by the surgeon together with the anesthesiologist, therapist and other specialists. The main elements of preoperative preparation are aimed at restoring disturbed biol, balance and correcting homeostasis: good nutrition, providing energy, nitrogen and vitamin balance; compensation of water and electrolyte deficiency with intravenous fluid infusions; correction of disturbances in the volume of circulating blood by transfusion of blood, red blood cells, and protein blood substitutes; treatment of cardiovascular system disorders; normalization of dysfunction of external respiration (breathing exercises, sanitation of the respiratory tract). Antibiotics in the preoperative period are prescribed for special indications (tumor growth into the transverse colon, concomitant inflammatory diseases of the lungs).
Anesthesia
with G. general. Multicomponent endotracheal anesthesia with the use of muscle relaxants and controlled breathing allows for a calm operation and creates optimal conditions for effective measures to prevent disturbances in hemodynamics and gas exchange.
Possible complications after stomach removal
Gastrectomy is a very large operation, and therefore there are a certain number of risks and complications:
- injury to organs adjacent to the stomach, such as the liver, pancreas and small intestine;
- bleeding caused by damage to blood vessels;
- nerve damage, which may impair bowel function;
- infections and abscesses;
- insufficient tightness of seams in the intestinal area;
- excessive scarring of the surgical site with the risk of developing intestinal obstruction;
- inflammation of the pancreas and bile ducts;
- inflammation of the esophagus (heartburn), caused by bile entering the esophagus;
- impaired wound healing;
- hernia scar on the skin of the abdomen;
- anastomotic stenosis (narrowing of the connecting seam);
- peptic ulcer of the anastomosis;
- pneumonia and thromboembolism;
- Iron-deficiency anemia.
Considering all the possible consequences of removing the stomach for cancer, care should be taken to ensure appropriate treatment after gastrectomy. All of the above complications may cause the need for further operations. In the early stages, many patients develop early or late dumping syndrome. Due to the fact that food passes through the digestive tract unusually quickly, after eating the patient may experience nausea, dizziness and weakness after half an hour (early dumping syndrome) or 2-3 hours (late dumping syndrome), and up to collapse of the circulatory system. All these factors are necessarily taken into account in the treatment plan, and, after removal of the stomach, each patient at the Nordwest clinic draws up its own rehabilitation and recovery program.
Operation technique
Gastrectomy in the strict sense of the word is considered to be such an operation when, in addition to the stomach, elements of the esophageal and intestinal epithelium are found in the removed specimen. Surgery for cancer includes, in addition to removal of the stomach, removal of its entire ligamentous apparatus and regional lymph nodes.
The correct choice of surgical approach for G. plays a significant role, largely determining the radicality of the operation, and provides conditions for reliable anastomosis. In each specific case, the access is chosen taking into account the location and nature of tumor growth, as well as the age and general condition of the patient.
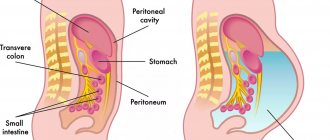
Transperitoneal G.
- the most common operation for advanced stomach cancer.
This approach is less traumatic than transpleural or combined, and, therefore, is more indicated for elderly and debilitated patients. The best access to the upper parts of the stomach is provided by a median laparotomy (see), which, if necessary, can be supplemented by resection of the xiphoid process of the sternum and partial sternotomy. In case of subcardial localization of cancer with limited spread to the abdominal part of the esophagus, transperitoneal G. is performed by resorting to diaphragmocrurotomy according to A. G. Savinykh. Rice.
2. Schematic representation of the boundaries of gastrectomy (black line; the dotted line indicates the boundary of the intersection of the greater omentum). Rice. 3. Scheme of mobilization of the stomach along the greater curvature and preparation for intersection of the gastrosplenic ligament: 1 - diaphragm; 2 - esophagus; 3 - gastrosplenic ligament (clamped); 4 - pancreas; 5 — large oil seal; 6 - stomach. Rice. 4. Scheme of applying an esophageal-intestinal anastomosis with a double-row suture: 1 - application of the first row of sutures; 2 - application of the second row of sutures. The main stages of transperitoneal G. with the application of esophagojejunostomy are as follows. After revision of the abdominal cavity, the edges include examination of the posterior wall of the stomach, gastro-pancreatic ligament, hilum of the spleen, and if a radical operation is possible, mobilization of the stomach begins (the boundaries are shown in Figure 2). The greater omentum is separated from the transverse colon, the stomach is released along the greater curvature along the gastrosplenic ligament and in the fundus (Fig. 3). The distal part of the stomach is mobilized by ligating the right gastric vessels, after which the left gastric artery is ligated and transected in its initial section. The stomach is cut off from the duodenum, the stump of the latter is sutured. Next, having ensured good exposure of the subphrenic space, both vagus nerves and the abdominal esophagus are crossed, the stomach is removed and the esophageal-intestinal anastomosis is started (Fig. 4).
Rice. 5. Scheme of applying esophagojejunostomy with the PKS-25 device: a and b - stages of the operation; c — operation completed; 1 - esophagus; 2 — stapler PKS-25; 3 - jejunum; 4 - spleen; 5 - transverse colon; 6 - pancreas.
There are a large number of different modifications of anastomosis of the jejunum with the esophagus - the most critical stage of the operation. The advantage remains on the side of the technically simplest and most reliable methods, which include the so-called. horizontal esophageal-intestinal anastomoses formed with double-row sutures. The method of applying esophageal-intestinal anastomosis using a PKS-25 stapler has become widespread (Fig. 5).
Transpleural G.
indicated for cancer of the upper stomach that has spread to the esophagus, or if there are signs of tumor growth into the diaphragm. The incision is made along the VII or VIII intercostal space with the patient positioned on the right side (see Thoracotomy). It is advisable to continue the incision on the anterior abdominal wall towards the navel, crossing the costal arch. After revision of the pleural cavity, a diaphragmotomy is performed and the operation continues in the abdominal cavity. Transpleural access provides greater opportunities for a thorough inspection of the organs of the upper floor of the abdominal and thoracic cavities and allows for a more reliable application of the esophageal-intestinal anastomosis. In our country, the first G, through transpleural access, was performed by B.V. Petrovsky in 1946.
G. abdomino-thoracic access
indicated for cancer of the upper stomach when there are doubts about operability. The patient's position is on the right side with the body tilted 45° to the operating table. Through the abdominal part of the incision, the abdominal cavity is inspected, after which, in case of inoperability, the abdominal wall is sutured, and the operation ends there. If radical surgery is feasible, the incision is continued along the VIII intercostal space and the pleural cavity is opened. A combined two-stage approach (median laparotomy and subsequent thoracotomy), requiring an operation in two stages and changing the position of the patient on the operating table, does not have any advantages.
In G., performed by transpleural or abdomino-thoracic access, the mobilization of the stomach is carried out in a top-down direction, i.e., it begins with the mobilization of the esophagus and proximal stomach. The basic details of the surgical technique remain the same.
Postoperative period
Treatment after surgery should be based on the principles of individualization. Main measures: 1) adequate postoperative pain relief, ensuring the prevention of painful shock, sufficient pulmonary ventilation and restoration of normal body functions (painkillers, long-term epidural anesthesia, medical anesthesia); 2) treatment of respiratory failure and prevention of pulmonary complications (oxygen therapy, breathing exercises, drugs that improve the drainage of the bronchial tree, antibiotics and sulfonamides); 3) prevention and treatment of cardiovascular disorders (cardiac glycosides, aminophylline, glucocorticoids if indicated); 4) prevention of thromboembolic complications (early physical activity of the patient, therapeutic exercise and massage, prescription of anticoagulants under the control of a coagulogram); 5) correction of water and electrolyte disturbances and complete parenteral nutrition (intravenous infusion of physiol, solution, polyionic solutions containing potassium, concentrated glucose solutions, transfusion of drugs containing proteins, amino acids, emulsified fats, blood transfusion, vitamin therapy).
Patients usually begin feeding patients by mouth on the 5th day after G., with water or tea allowed on the first day, and liquid food on subsequent days (jelly, juices, raw eggs, butter, broth, thin porridge, etc.); meals are fractional, in small portions up to 6 times a day. By the 14-15th day, patients are transferred to table No. 1 (see Medical nutrition).
Postoperative complications
: insufficiency of esophageal-intestinal sutures from the mouth (the most common complication), pneumonia, pulmonary embolism.
Nutrition after gastric removal
Many patients and their relatives are concerned about what they can eat after removal of the stomach, and whether they need to follow a diet. Of course, gastrectomy imposes its own restrictions regarding nutrition, because the full process of digesting food now becomes impossible. Despite this, over time, the patient has the opportunity to consume all categories of foods, maintain a complete diet in terms of the consumption of proteins, fats, and essential vitamins. The fundamental change in this matter concerns the method of cooking and the amount of food consumed per meal. Preference should be given to steaming, stewing and boiling. One portion should be small, meals throughout the day should be fractional. The diet after gastrectomy involves avoiding very fatty, fried foods and sweets.
Overeating can cause discomfort and pain, so it is important to monitor portion sizes as closely as what is served during meals. For the first time after a gastrectomy, patients are fed through IVs: nutrients are supplied through the blood.
Results of the operation
Complete removal of the stomach often leads to significant disturbances in the body of those operated on. Patients who are practically cured of cancer in the long-term postoperative period present a number of complaints, indicating that the body does not always provide the necessary level of compensation for lost functions. Many disorders have a pronounced clinical picture (eating disorders, agastric anemia, reflux esophagitis, dumping syndrome, etc.) and can be combined with the concept of “post-gastrectomy syndrome” (see Post-gastroresection syndrome). Patients who have undergone G. require constant medical supervision and treatment.
Mortality after gastrectomy averages approx. 7% with fluctuations (from 3.3 to 26.1%, according to various authors). Long-term results of the operation vary depending on the stage, the nature of the tumor (gistol, structure, type of growth) and its location in the stomach (according to many authors, the 5-year survival rate is approximately 30%).
Bibliography:
Babichev S.I. Total gastrectomy, M., 1963; Berezov Yu. E., Cancer of the cardial part of the stomach, M., 1960; Kvashnin Yu. K. and Pantsyrev Yu. M. Consequences of gastrectomy, M., 1967; Mayat V.S. et al. Gastric resection and gastrectomy, M., 1975; Peter r s o n B, E. Cancer of the proximal stomach, M., 1972; Petrovsky B.V. Surgical treatment of cancer of the esophagus and cardia, M., 1950; Ts and ts and n i-di K. N. and Bogdan o in A. V. Esophageal-intestinal and esophageal-gastric anastomoses, M., 1969; Yudin S.S. Sketches of gastric surgery, M., 1955; McNeer G. a. Pack G. T. Neoplasms of the stomach, Philadelphia, 1967; Schlatter C. t)ber Ernahrung und Verdauung nach vollstandiger Entfernung des Magen-Osophagoenterostomie bein Menschen, Bruns' Beitr. klin. Chir., Bd 19, S. 757, 1897
Yu. M. Pantsyrev.
Progress of the operation
In LCRYGB surgery, the size of the stomach is reduced using a surgical staple. This bariatric procedure cuts the stomach so that it leaves a reservoir the size of a walnut. Then the so-called “biliopancreatic branch” (50 cm) is measured. The distal intestinal loops are connected to the reservoir (GEA gastrojejunostomy). This results in food being transported from the stomach directly to the small intestine. The junction of the small intestine (jejuno-jejunal anastomosis EEA) is formed at a distance of 120-150 cm from the GEA.