Dairy products occupy a place of honor in every person’s complete diet, along with bread, meat, vegetables and fruits. Dairy products contain many vitamins, nutrients and calcium, which ensure the strength of the skeletal system, nails, hair and other tissues.
For those suffering from pancreatitis, drinking milk results in diarrhea, nausea, abdominal pain, bloating; in other words, pancreatitis and dairy products are not very compatible. This is caused by a deficiency of lactase, an enzyme necessary for digesting dairy products. It is necessary for such people to consume dairy products, but they just have to do it correctly.
What kind of dairy can you eat if you have inflammation of the pancreas?
The main rule in case of illness is to consume foods in moderation and diluted quantities in different dishes. To achieve this, fatty foods are excluded from the diet. For preparation, milk must be diluted with a certain amount of drinking water, which reduces its fat content.
Milk dishes are indicated for the disease:
- You can drink tea with a small amount of fresh milk added.
- Cottage cheese pastes.
- Milk jelly.
- Casseroles of different cooking methods and products used, cereals.
- Souffle.
- Puddings.
- Sum and milk porridge.
When choosing fermented milk products, you must choose low-fat or low-fat products:
- Buttermilk.
- Sour cream (for sauces or dressings in very limited quantities).
- Ryazhenka.
- Curdled milk.
- Yogurt.
- Kefir.
- Cottage cheese.
- Hard cheeses.
Cottage cheese and hard cheeses are made by fermenting milk, which provides benefits for a patient with pancreatitis:
The products contain over 120 types of useful substances, represented by enzymes, fatty acids, mineral elements, amino acids, vitamins;
- Metabolism is stabilized.
- Flatulence is reduced.
- Pathogenic flora is suppressed.
- Protects the intestinal wall from infectious effects.
- The functioning of the gastrointestinal tract system is normalized.
During the chronic stage of the disease, the consumption of fermented milk products created on the basis of fermentation of living microorganisms relieves inflammation of the gland and accelerates the restoration of damaged mucous tissues of the gastrointestinal tract. It is permissible to include milk in the diet if there is no negative reaction or negative consequences. You can drink or eat diluted up to 100 g of the product per day.
What fermented milk can you eat if you have inflammation of the pancreas?
Sour milk contains over 120 types of beneficial substances, including enzymes, fatty acids, mineral elements, amino acids, and vitamins;
- Metabolism is stabilized.
- Flatulence is reduced.
- Pathogenic flora is suppressed.
- Protects the intestinal wall from infectious effects.
- The functioning of the gastrointestinal tract system is normalized.
During the chronic stage of the disease, the consumption of fermented milk products created on the basis of fermentation of living microorganisms relieves inflammation of the gland and accelerates the restoration of damaged mucous tissues of the gastrointestinal tract.
Yogurt
The process of preparing yogurt involves fermenting a pure culture of thermophilic streptococcus and Bulgarian bacillus in fresh milk. The taste is improved by adding vegetables or fruits, their juices or pulp. This product is also used for other diseases as dietary food.
The impact of yoghurts on health in pancreatitis:
- Enriches with minerals and vitamins.
- Supports the immune system.
- Simplifies the process of digestion of dairy products due to processing by lactic acid bacteria.
- Normalizes gastrointestinal motility, helps with constipation.
- Used as a medicinal and prophylactic agent for various intestinal disorders.
- Fills the body with proteins of animal origin, which promotes tissue restoration due to peptides and casein processed into amino acids.
If the product is not created on the basis of natural ingredients, then a patient with pancreatitis should not use it. For acute stages of the disease, only 1% fat yogurt is suitable after 3 weeks from the onset of the disease. The intake should be with a gradual increase in dose - per day from ¼ glass to a full glass separately from other food instead of kefir.
In the remission stage of the chronic course of the disease, the fat content of yogurt can be 3.2%; it can be used with syrup, honey in small quantities, fresh juices, berry pulp, and fruits.
Important!
Before consumption, yoghurt for patients with pancreatitis must be heated to a temperature of 20–25 °C.
In the diet of a person suffering from pancreatitis, yogurt is an essential component due to the content of many nutrients and food proteins.
Cottage cheese
For pancreatitis, the use of cottage cheese is allowed as part of a variety of dietary dishes or as an independent product. The pancreas and organs of the digestive tract are not irritated by fats and proteins of the product, due to their rapid absorption.
There are several requirements for cottage cheese that this product for patients with pancreatitis must meet:
- The consistency should be pasty.
- Only fresh cottage cheese is allowed.
- Do not eat the product if it is acidic or expired.
- You cannot cook from a fatty product or add spices that have a juice-like effect.
- It is unacceptable to cook cottage cheese by frying, with the formation of a fried or crispy crust, using an abundance of oil.
Ryazhenka
The use of this product is very controversial. Different patients suffering from pancreatitis are able to react differently to fermented baked milk. This is due to the rather high fat content of the product. With a fat content of up to 4%, it is permissible to consume no more than 1 glass of this product per day. At the stage of remission, fermented baked milk is alternated with other dishes made from fermented milk products. To make the diet more varied, fermented baked milk is prepared with the addition of fruits or berries.
Rules for using fermented baked milk in case of illness:
- The product can be taken as an afternoon snack with bread or cookies.
- In the morning, the best time to take the product is after the meal.
- You should make sure that there is at least 1-2 hours before bedtime from the last use of the product.
Sour cream
Sour cream is a fermented milk product with enormous fat content. During an exacerbation of a chronic disease or the acute stage of pancreatitis, the use of this product can create a large load on the gastrointestinal tract and gland itself. Even a small spoon of sour cream can cause a relapse.
The inclusion of the product in dishes is allowed only in cases of stable remission of pancreatitis. It is necessary to verify the presence of non-contaminated fat in the feces in order to include the product in the diet.
The ideal schedule for introducing sour cream into food is to consume up to 1 tsp per day. in one day. The product should be of high quality, not expired, with a fat content of no more than 20%. The composition of sour cream should not include anything other than sourdough, milk and cream.
The product is accepted only when prepared with other dishes. Most often in combination with cottage cheese, vegetable puree, soups, sauces, salads, casseroles, and puddings. It is not permissible to use with fried mushrooms or fish in sour cream.
Cottage cheese recipes
It is not necessary to include cottage cheese in dishes; it can be used as an independent product. Due to the fact that cottage cheese is combined with various foods, there are different taste variations, namely:
- Salty cottage cheese. If you mix this product with vegetables, herbs, and add a little sour cream, you can get a very tasty diet breakfast;
- Sweet cottage cheese. Various dried fruits, fruits, honey are added to this product in accordance with taste preferences. From these components you can make very tasty puddings and soufflés.
Cottage cheese casserole
This option for preparing casseroles has been familiar to many since early childhood. A person who is on a constant diet due to problems with the pancreas cannot please himself with many tasty but unhealthy desserts, but you can eat casserole even every day.
To prepare we will need:
- Cottage cheese (300 gr);
- Egg (2 pcs);
- Semolina (3-4 tbsp);
- Raisins, which are added to taste (can be replaced with any other fruit);
- Vanillin (very little is needed, literally on the tip of a knife);
- Sugar (4 tbsp required);
- Baking powder (1 sachet);
- Just a little salt.
The cooking process is quite simple:
- Rinse the raisins and pour boiling water over them. This needs to be done so that it swells a little;
- Mix semolina with sour cream and leave for 15 minutes;
- Add cottage cheese and baking powder to the resulting mixture. Mix well;
- In a separate container, beat eggs with sugar;
- Carefully add the curd mass to the resulting mixture so that the whipped foam does not settle;
- Add raisins and mix everything carefully;
- Pour just a little semolina into the bottom of the baking dish and distribute evenly. This must be done in order to avoid possible burning;
- Place the dough and bake in the oven at 180 degrees for 40 minutes.
Syrniki
For pancreatitis, you can also make cheesecakes.
Cheesecakes can be boiled or steamed, less often fried in a frying pan.
To prepare them you will need:
- Egg (1 piece);
- Cottage cheese 9% (200 g - approximately 1 pack);
- Butter (0.5 tsp);
- Sour cream (1 tbsp);
- Flour (0.5 cup);
- Semolina (1 tsp).
The cooking process is very simple:
- Mix the pureed cottage cheese with semolina, sugar and egg;
- Mix the resulting mass well, shape (1.5 cm), bread in flour;
- Place in a baking tray, which should first be greased with oil, and place in the oven for 25 minutes at 180 degrees;
- You can serve with a little sour cream.
Lazy dumplings
For pancreatitis, lazy dumplings with cottage cheese can be prepared according to the usual recipe, but it is necessary to reduce the amount of sugar.
To prepare we will need:
- Sugar (2 tsp);
- Low-fat cottage cheese (250 g);
- Flour (3-4 tbsp).
Cooking process:
- Mix sugar with egg, add cottage cheese, flour and knead thoroughly;
- From the resulting dough, you need to form a sausage;
- Cut the sausage into pieces and make a ball from each piece;
- Cook the dumplings for 7 minutes after floating.
They must be served warm, topped with yogurt.
What is prohibited?
There are a number of dairy products that are contraindicated for those suffering from pancreatitis, even in the form of supplementation or heat treatment. Among them :
- Factory products containing flavoring, aromatic, and coloring additives.
- Condensed milk.
- Smoked and processed cheeses are spicy.
- Ice cream.
- Whole milk.
- Fatty cheeses.
- Fatty and sour cottage cheese.
- Sour cream.
- Cream.
It is prohibited to buy dairy products “from hand” without proper processing. On the one hand, the products are definitely of natural origin, but on the other hand, there is a risk of the presence of infectious bacteria, such as salmonella.
For those suffering from pancreatitis, infection with such a microorganism can cause serious consequences and cause serious damage to health and well-being. Store-bought products should be without additives, low-fat and fresh.
Features of use at different stages of the disease
Depending on the characteristics of the disease, the patient’s diet is adjusted. Many products that have been indicated in remission for acute or chronic exacerbations will cause harm or defeat all efforts to stabilize the condition.
In the chronic stage
At this stage of the disease, not all dairy products are allowed. Kefir and cottage cheese are allowed, according to the scheme :
- From the moment the attack begins, you should wait 4-5 days from eating foods, and the cottage cheese should be finely ground.
- At the end of the week after the attack of the disease, kefir with a fat content of 1% is introduced.
- From the beginning of the third week after an attack, it is allowed to take yogurt, yogurt, fermented baked milk without sugar, additives of berries or fruits, and thickeners.
During the period of exacerbation
From the onset of an attack of pancreatitis (acute stage), you should immediately exclude all dairy products from the diet. Only from 2–3 days is milk porridge allowed in liquid, ground form, prepared with milk 2.5% fat or diluted in a 1 to 1 ratio with water.
5-6 days after the attack of the disease, the use of non-sour low-fat cottage cheese is indicated. The dose is dosed from the first day to 50 g and up to 100 g of the product a week later. It is allowed to prepare a steam omelet using diluted milk.
If positive dynamics are observed, then the diet begins to be diluted with kefir. It is recommended to use it gradually from 50 g on the first day after 10–14 days from an attack to 100 g a week later.
It is allowed to add unsalted butter in the amount of 5 g per day to fruit, vegetable puree or porridge. A person suffering from pancreatitis must adhere to this regimen until acute remission is achieved and the exacerbation is completely relieved. This is approximately 2 months.
In remission
Despite the fact that all the dangers and discomfort are behind us, the use of milk in diluted form is recommended for jelly, omelettes, soups and cereals. The daily allowance for butter is no more than 10 g, added to puree or porridge. Low-fat cottage cheese and 1% fat kefir are retained in the diet.
It is allowed to replace kefir with homemade yogurt, bifidok, fermented baked milk, yogurt with a fat content not exceeding 2.5%. The presence of these products in the diet is mandatory. It is allowed to eat mild soft cheeses, dilute fermented milk drinks with sweeteners or sugar, berry or fruit puree. No more than 1 tsp. sour cream and cream with a fat content of no more than 10% are introduced for the daily requirement in sauces and other dishes.
What diet is necessary for pancreatitis?
The main goal of the diet for inflammation of the pancreas is to unload the digestive tract and reduce the production of digestive enzymes, which during inflammation do not exit through the ducts into the duodenum, but remain inside the gland and “digest” its tissues. Nutrition for pancreatitis should be balanced to cover the body's needs for essential nutrients, vitamins and minerals. The basic nutritional method for patients with pancreatitis was developed by the therapist, founder of dietetics and clinical gastroenterology, Manuil Isaakovich Povzner, and was given the number 5p.
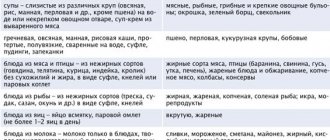
Rice. 1
The essence of the diet is to use foods that do not provoke an abundant secretion of digestive enzymes by the gland. The standard menu for pancreatitis contains warm dishes of liquid, semi-liquid or mushy consistency, prepared by boiling, stewing, steaming or baking. Such restrictions are explained by the fact that fried foods take a long time to digest, and against the background of a decrease in pancreatic enzymes, they can ferment, causing bloating, pain and cramping in the abdomen. Raw vegetables and fruits are also limited due to their ability to provoke gas formation.
The most stringent nutritional requirements are imposed during exacerbation of chronic pancreatitis or during acute inflammation. For 2-3 days, any food is contraindicated for patients. Only unlimited drinking and drip administration of nutrient solutions are allowed. You need to start eating gradually, with small portions of up to 150 ml 5-6 times a day. Preference should be given to liquid dishes that are easily digestible and do not burden the gastrointestinal tract: vegetable broths, semi-liquid purees, porridges, slimy soups. During the week, the menu is expanded, increasing calorie content and serving sizes.
Rice. 2
The daily diet should contain:
- Complex carbohydrates - up to 350 g;
- Proteins - up to 125 g;
- Fats - up to 70 g;
- Vitamin C - 150 mg;
- B vitamins (B1 and B3) - up to 2 mg (vitamin B1 requires up to 10 mg);
- Vitamin A - 10 mg;
- Calcium - 0.8 g;
- Magnesium - 0.5 g;
- Iron - 0.03 g;
- Phosphorus - 1.3 g;
- Sodium - 3 g.
The volume of liquid that the patient should consume during the day is at least one and a half liters, and the total daily calorie content of meals is no more than 1800-2500 kcal.
Goat milk
The peculiarity of this dairy product is its low fat content and high content of nutrients. For patients with pancreatitis, nutritionists and therapists strongly recommend adding this product to their usual diet.
Before taking it, you should know a few rules that will allow you to get the greatest benefit, protect against side effects and make the product tasty.
- Goat milk is consumed warm.
- Boiling is required. To digest a raw product, the body will need much more energy, which is fraught with additional stress on the immune system and gastrointestinal tract.
- It is best to combine milk with other dishes and products. This makes the animal fats of the product easier to digest.
- The first three methods should be accompanied by diluting milk with boiled water in a proportion of equal parts or 1 to 2 parts of water.
- The first doses should not exceed 100 ml, even better than 50 ml, in order to determine exactly how the gastrointestinal tract will react to goat milk. The maximum dose at the end of this regimen is 200 ml.
- It is recommended to take it in the morning on an empty stomach, as goat milk has antibacterial properties, which has a soothing, healing and protective effect on the pancreas.
- It is best to use the services of a nutritionist, who, after certain tests and examination, will determine the optimal dose, dosage regimen and duration of therapy.
What to do in case of lactase deficiency
A digestive enzyme such as lactase increases the absorption of dairy and fermented milk products. Deficiency of this substance is a fairly common problem among adults, as it accounts for approximately 15-20%. A deficiency of this substance is noticed very simply:
- The reaction to dairy products from the gastrointestinal tract is accompanied by increased fermentation.
- Dyspepsia occurs, which is manifested by pain along the intestinal tract, bloating, and diarrhea.
In most cases, the cause of milk intolerance is pathology of the small intestine, which worsens with the development of pancreatitis. If there is a negative reaction of the body to whole milk, you should try drinking it in diluted form, or as a fermented milk product. Adding whole milk to jelly, tea, soup and other dishes also helps to cope with the problem quite well.
What are lactose and lactase?
Lactose, or milk sugar, is the main carbohydrate in milk. At its core, lactose is not dangerous, and even has benefits: in addition to its nutritional value, it, for example, promotes better absorption of calcium from milk. However, the digestibility of lactose plays a crucial role in this. Lactic sugar intolerance is a problem that, according to various sources, affects 30 to 50% of Russians [1], [2]. This problem is related to an enzyme called lactase, which is produced by the body, is responsible for the absorption of lactose and becomes less active with age - as can be seen in the graph below:
Dietary dishes with milk for illness
If you are ill, you should adhere to a strict diet that will allow you to consume dairy products in a controlled manner, in the form in which they bring benefits to the body without harmful effects or worsening the condition.
The most common dishes based on whole milk or a diluted product are:
- Omelette.
- Souffle.
- Puddings.
- Casseroles.
- Adding milk to hot drinks.
- Milk porridge.
- Milk-based soups.
- Curd paste.
- Cheese pancakes based on cottage cheese.
- Steamed cottage cheese soufflé or with the addition of vegetables and fruits.
Is lactose-free milk harmful?
Is it possible to drink lactose-free milk if there is no problem with lactase deficiency? Can! For example, Valio Eila milk contains 30% less carbohydrates, which means fewer calories. It is also additionally enriched with vitamin D, which will help provide the body not only with the most important vitamin, but also with calcium. The absence of lactose in this case does not affect the absorption of beneficial nutrients from milk or the taste of the product, so lactose-free milk benefits the body.
[1] Union of Pediatricians, St. Petersburg, 2012
[2] Yulia Khabarova, Suvi Torniainen, Hanna Nurmi, Irma Järvelä, Mauri Isokoski, and Kari Mattila: Prevalence of lactase persistent/non-persistent genotypes and milk consumption in a young population in north-west Russia, 2009