Risks of occurrence
Scientists have not yet established the exact cause of pancreatic cancer. The growth of a malignant neoplasm can begin under the influence of the following provoking factors:
- Excessive smoking – causes ischemia (oxygen starvation) of organ tissue;
- Excess of easily digestible carbohydrates in the diet creates additional stress on the gland;
- Chronic pancreatitis - the development of atypical cells occurs against the background of an uncontrolled inflammatory process in the pancreas;
- Excess body weight - fat deposits affect internal organs, including the pancreas, and additional load increases the risk of developing tumors;
- Chronic intoxication – long-term toxic effects negatively affect the structure and functions of the pancreas;
- Oral diseases - caries, periodontitis, periodontal disease, which significantly increase the risk of the formation of tumor foci in the pancreas.
The highest incidence of pancreatic cancer is typical for economically developed countries, which are characterized by urbanization and high socio-economic indicators. Malignant neoplasms develop with a burdened heredity.
Tumor cells from other organs affected by the tumor process metastasize to the pancreas. More than 75% of patients with pancreatic cancer have reached 70 years of age. However, the pathology also affects younger people.
Expert opinion
Author: Alexey Andreevich Moiseev
Oncologist, chemotherapist
Pancreatic cancer is a malignant tumor that develops in the glandular tissue or ducts of the organ. The tumor very quickly destroys tissue and grows into neighboring organs, so it is important to know the main symptoms of the disease in order to consult a doctor in a timely manner.
According to doctors, the main cause of the tumor is a genetic failure at the cellular level. As a result, the affected cells cannot perform basic functions, but multiply intensively, which leads to the formation of a tumor. Medicine is unable to find the root cause of oncology and answer the question of what gives impetus to the degeneration of healthy cells into cancerous ones. Research has been conducted for many years, but no clear cause of the pathology has been found.
Provoking factors are considered to be smoking, excessive alcohol consumption, diabetes mellitus, surgical interventions on the gastrointestinal tract, and poor environmental conditions.
Not a single doctor will answer you how long a patient will live or whether a patient will live at one or another stage of pancreatic cancer. It all depends on the severity of the pathology, the extent of the damage, and the state of the patient’s body. Doctors at the Yusupov Hospital practice an integrated approach to diagnosing and treating pancreatic cancer in a hospital setting.
Pathogenesis
It is known that chronic pancreatitis increases the risk of pancreatic cancer by 9-15 times. The main role in the development of pancreatitis and cancer belongs to the stellate cells of the gland, which form fibrosis and at the same time stimulate tumorigenesis. Stellate cells, producing extracellular matrix , activate the destruction of gland cells and reduce insulin production by β-cells. At the same time, they increase the oncogenetic properties of stem cells, stimulating the occurrence of pancreatic cancer. And the constant activation of stellate cells disrupts the homeostasis of the tissues surrounding the tumor, which creates the ground for the invasion of cancer cells into neighboring organs and tissues.
Another factor in oncogenesis is obesity . Obesity undoubtedly affects the pancreas. Visceral fat is an active endocrine organ that produces adipocytokines . In insulin resistance, steatosis and inflammatory cytokines cause organ dysfunction. Elevated levels of free fatty acids cause inflammation, ischemia , organ fibrosis , and ultimately cancer .
The following sequence of changes in the pancreas has been proven - non-alcoholic steatosis , then chronic pancreatitis and cancer . Patients quickly develop cachexia , which is associated with dysregulation of the hormones ghrelin and leptin under the influence of the same cytokines. If we take into account gene mutations, it can take 10 years from the appearance of the first signs of mutations to the formation of a non-invasive tumor; then it takes 5 years for the transformation of a non-invasive tumor into an invasive one and the development of a metastatic form. And after this, the oncological process quickly progresses, leading to an unfavorable outcome within 1.5-2 years.
Symptoms
The insidiousness of pancreatic cancer lies in the fact that the initial stages of the disease are practically asymptomatic. There is no severe pain or obvious manifestations of any abnormalities in health or discomfort. You should be wary and immediately visit a doctor if the following symptoms appear:
- Pain in the abdominal area, radiating to the back, increasing with changes in body position;
- Yellowness of the skin;
- A sharp decrease in body weight;
- Loss of appetite;
- Nausea and vomiting, dizziness, loose stools, weakness for no apparent reason.
With malignant tumors, the pain heads are usually localized in the epigastric region. If the tumor is located in the tail of the organ, patients complain of pain in the left upper quadrant of the abdomen. Gradually the pain becomes more severe and constant, intensifying at night. It can be localized in the back (when it grows into retroperitoneal structures).
The nature of the pain changes when changing position. The patient feels relief when bending the body forward. Exacerbation may occur during attacks of acute pancreatitis. Pain in the left half of the abdomen, constipation or signs of intestinal obstruction are caused by metastasis of cancer of the body or tail of the pancreas to the colon.
Acinar carcinoma is accompanied by a syndrome of focal inflammation and subcutaneous lipoid necrosis. It is characterized by joint pain and increased levels of eosinophils in the blood, high levels of lipase in the blood serum. Similar symptoms are characteristic of recurrent pancreatitis.
Over time, jaundice becomes one of the main symptoms of pancreatic cancer. It is detected in 90% of patients with tumor lesions of the head of the organ. Jaundice is progressive. Tumor remission may result in less jaundice. In case of cancer of the tail and body of the pancreas, jaundice is rarely recorded. With the development of cholangitis, body temperature rises.
Treatment at various stages
Specialists at our Oncology Center in Moscow develop treatment regimens for pancreatic cancer on a strictly individual basis. Doctors take into account the histological type of tumor, its location, the patient’s general health, etc. But the most important parameter is the stage of development of the oncological process.
The most effective method of treatment at the moment remains surgery. It is almost always supplemented with pharmacological and radiation therapy. In the early stages of the existence of a malignant neoplasm, it can be eliminated by operations of various scales:
- Whipple operation - removal of the head of the gland;
- segmental resection - removal of the body of the gland with subsequent connection of its remaining parts;
- distal resection – removal of the body and tail of the gland;
- total resection – removal of the entire gland.
These interventions will be effective on:
- stage zero (the tumor is represented by only a certain number of malignantly degenerated cells in one place);
- first stage (the tumor is entirely in the gland, without affecting either the lymph nodes or other organs):
- second stage (the tumor has spread to the tissues and lymph nodes surrounding the gland, but has not yet grown through the walls of neighboring large vessels).
Also, all nearby lymph nodes are often removed for preventive purposes. In addition, at the second stage, those parts of other organs into which the malignant process has managed to spread are also subject to excision: areas of the duodenum, stomach, gall bladder, etc.
At the third (tumor growth through the walls of large vessels) and fourth (metastases in distant organs) stages, palliative surgical interventions are mainly performed. Their goal is to improve the patient’s quality of life and eliminate the most severe symptoms of a pancreatic tumor. These can be operations on:
- removal of those parts of the tumor that put pressure on surrounding organs, disrupting their functions, or compress blood vessels and nerve pathways;
- removal of the largest metastases, often in combination with HIPEC (Hyperthermic Intra Peritoneal Chemotherapy), an innovative method of hyperthermic intraperitoneal chemotherapy for peritoneal carcinomatosis.
- elimination of obstruction of the biliary tract or intestines, including by applying stents and anastomoses;
- suturing pathological holes in the walls of adjacent hollow organs.
Diagnostics
Detection of a pancreatic tumor at the first stage is extremely rare. This is due to the absence of characteristic symptoms. Most often, cancer in the early stages is diagnosed during examination for another disease.
Comprehensive diagnosis of pancreatic cancer includes:
- General and biochemical blood test. It is prescribed to identify the inflammatory process in the body. Pay attention to such indicators as ESR, leukocyte formula, ALT, AST, bilirubin, lipase, amylase and alkaline phosphatase;
- Coagulogram. Determined to assess the degree of blood clotting disorder;
- Determination of the level of tumor markers in the blood. CA-242 and CA-19-9 are considered specific tumor antigens for pancreatic cancer. An increase in their concentration indicates a high risk of tumor formation;
- Ultrasound examination (ultrasound) of the abdominal organs. Allows you to evaluate the structure of the pancreas, its size, as well as the location of the pathological focus;
- Computed tomography (CT) and magnetic resonance imaging (MRI). Layer-by-layer examination of the pancreas makes it possible to assess the location, size and degree of tumor invasion into adjacent tissues;
- Positron electron computed tomography (PET-CT). A contrast agent is used for the study. After the labeled isotope accumulates in the pancreas, the organ is examined for the presence of tumor formation;
- Endoscopic retrograde cholangiopancreatography. The head of the pancreas is examined using an endoscope. A contrast agent is injected through it, which stains the organ. A series of x-rays allows you to determine the location and size of the tumor;
- Laparoscopy is a high-tech and informative research method. During the procedure, it is possible to perform a biopsy for histological analysis of the tissue samples obtained from the pathological focus;
- Biopsies. Pancreatic cancer must be confirmed by histological examination. A biopsy can determine the type and stage of cancer. This is necessary to determine treatment tactics.
Diagnosis of pancreatic cancer in the early stages of the disease (before the lumen of the bile ducts closes and penetrates the duodenum) is difficult.
Evaluation with barium contrast X-ray is only useful if the tumor is large. An x-ray may show displacement of the stomach cavity and the posterior wall of the abdominal cavity. The tumor can affect the mucous membrane of the duodenum and stomach. When barium suspension is used, the structures have an irregular shape.
The use of ultrasound and computed tomography makes it possible to detect small tumors, including neoplasms of the body and tail of the pancreas. If the results of the study are negative, endoscopic ultrasonography is performed. Using computed tomography, tumor lesions of the pancreas and its penetration into the surrounding area, cancer metastasis to the liver and neighboring lymph nodes are determined. A puncture biopsy allows for histological examination and confirmation of the diagnosis.
Patients with obstructive jaundice undergo transhepatic cholangiography and endoscopic retrograde cholangiopancreatography. Transhepatic penetration reveals the proximal site of obstruction and helps distinguish pancreatic malignancy from cancer of the gallbladder, bile duct, or papilla of Vater. Using endoscopic retrograde cholangiopancreatography, narrowing of the common pancreatic duct and compression of the common bile duct by a neoplasm can be detected.
Endoscopic ultrasound is useful in cases where resection is contemplated. Before surgery, surgeons prescribe angiography to exclude involvement of draining veins in the tumor process. In approximately 60% of cases, cancer occurs in the head of the pancreas. Tumors are usually poorly demarcated.
Closure of the lumen of the pancreatic duct with an upstream dilation, as well as signs of chronic pancreatitis, create a “double-barreled shotgun” symptom when both ducts (pancreatic and common bile ducts) are dilated. These changes are detected by imaging.
The diagnosis is confirmed in 75% of cases either cytologically (using fine-needle aspiration biopsy) or histologically (using internal biopsy under ultrasound guidance or computed tomography).
Ductal adenocarcinoma is detected in 80% of patients suffering from pancreatic cancer. They vary in the degree of differentiation, the presence of mucin, and the presence or absence of giant cells or squamous elements. Less commonly, malignant neoplasms have predominantly acinar characteristics or a main mucous (colloid) component.
Causes
The exact reasons have not been identified, but there is evidence of the role of certain factors:
- Diseases of the pancreas. First of all, chronic pancreatitis . In patients with alcoholic pancreatitis, the risk of malignant diseases of the organ increases 15 times, and with simple pancreatitis - 5 times. With hereditary pancreatitis, the risk of cancer is 40% higher.
- Pancreatic cysts, which in 20% of cases develop into cancer. A high risk of malignancy is indicated by a family history of cancer of this organ.
- Genetic mutations. More than 63 mutations are known to lead to this disease. 50-95% of patients with adenocarcinomas have mutations in the KRAS2, CDKN2 gene; TP53, Smad4. In patients with chronic pancreatitis - in the TP16 gene.
- Obesity , which is always associated with pancreatitis , diabetes and an increased risk of prostate cancer. Obesity during adolescence increases the risk of cancer in the future.
- Type of food. A diet high in protein and fat, lack of vitamins A and C, carcinogens in food (nitrites and nitrates). An increased content of nitrates in products leads to the formation of nitrosamines , and they are carcinogens. Moreover, dietary habits and the carcinogenic effects of foods appear after several decades. Thus, nutritional characteristics in childhood and young adulthood also matter.
- Increased levels of cytokines (in particular IL-6 cytokine), which play a role not only in the development of inflammation, but also in carcinogenesis.
- Smoking is a proven risk factor for cancer of this organ.
- Exposure to ionizing radiation and carcinogenic fumes (for example, in the aluminum industry, dry cleaners, oil refineries, gas stations, dyeing industries). These unfavorable environmental factors cause DNA changes and failure of cell division.
- Gastrectomy (removal of the stomach) or gastric resection. These operations for ulcers and benign tumors of the stomach increase the risk of pancreatic cancer several times. This is explained by the fact that the stomach is involved in the degradation of carcinogenic substances entering the body with food. The second reason is the synthesis of cholecystokinin and gastrin in the mucosa of the small intestine and pylorus (due to the absence of the stomach or part of it), and this stimulates hypersecretion of pancreatic juice and disrupts the normal functioning of this organ.
Classification
The classification of pancreatic cancer depends on the histological structure of the tumor and the location of the tumor. According to histological structure, malignant neoplasms of the pancreas are divided into:
- Squamous;
- Adenocarcinoma;
- Cystadenocarcinoma;
- Glandular-squamous;
- Unspecified cancer;
- Ductal adenocarcinoma.
The most common form of pancreatic cancer is adenocarcinoma. The tumor is formed from the epithelial cells of the ducts. It is accompanied by an intense fibrotic reaction. Cystadenocarcinoma has a generally favorable prognosis. Acinar cancer is observed in 5% of patients. Pancreatic sarcoma is a rare disease that is usually diagnosed in childhood.
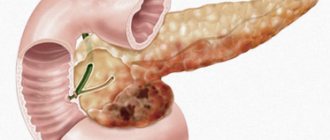
In accordance with the location, cancer of the head, body, and tail of the organ is distinguished. In 65% of cases, the tumor is localized in the head of the pancreas, in 30% in the body and tail, and in 5% only in the tail. Malignant neoplasms of the head of the pancreas penetrate the duodenum.
The exocrine part of the pancreas has a well-developed network of lymphatic ducts that are located along the blood vessels. Tumors localized simultaneously in the tail and body of the pancreas spread through the lymphatic ducts.
List of sources
- Veligotsky N.N. Obstructive diseases of the pancreaticoduodenal zone / N.N. Veligotsky, A.N. Veligotsky. – Kharkov: Planeta-Print, 2015. – 136 p.
- Malyarchuk V.I., Klimov A.E., Pautkin Yu.F. Biliopancreatoduodenal cancer: Monograph. – M.: RUDN Publishing House, 2006. – 444 p.
- Galperin E.I. Lectures on hepatopancreatobiliary surgery / E.I. Galperin, T.G. Dyuzheva. – M.: Vidar, 2011. – 536 p.
- Shchepotin I.B., Lukashenko A.V., Kolesnik E.A. et al. (2011) Pancreatic cancer: criteria for resectability. Clinical Oncology, (4(4)): 65-71.
- Patyutko Yu.I., Kotelnikov A.G., Abgaryan M.V. Modern surgical and combined treatment of patients with exocrine cancer of the head of the pancreas and organs of the periampullary zone. Practical oncology. T.5, N2, 2004, pp.94–107.
Pancreatic cancer in men and women
Statistics show that men are more likely to suffer from pancreatic cancer. At risk are representatives of the stronger sex over 50 years of age, smokers, eat fatty and fried foods in large quantities, and are overweight. Therefore, when the first pathological symptoms appear, doctors recommend seeking medical help for a comprehensive examination.
Women are less likely than men to suffer from this disease. However, against the background of other somatic diseases, they do not pay attention to the early signs of pancreatic cancer. In this regard, there is a delay in seeking medical help and detection of the tumor at later stages.
General information
The pancreas is an organ of the human digestive system that simultaneously performs an exocrine function (secretes digestive enzymes) and an intrasecretory function (synthesis of hormones - insulin , glucagon , somatostatin , pancreatic peptide ). Malignant tumors of this organ can be localized in the endocrine and exocrine sections, as well as in the epithelium of the ducts, lymphatic and connective tissue. The ICD-10 code for pancreatic cancer is C25. Anatomically, the gland consists of parts - head, body, tail. The subheadings of ICD-10 include processes localized in various departments and have codes from C25.0 to C25.8. If we consider the anatomical localization of the tumor process, then more than 70% of all malignant tumors of the gland occur in the head. This is a disease of the elderly - its greatest incidence is at the age of 60-80 years and very rarely at the age of 40 years. Men get sick 1.5 times more often. The disease is more common in people who eat high-carbohydrate and fatty foods. In patients with diabetes, the risk of developing this disease doubles.
Pancreatic cancer remains the most aggressive and is characterized by extremely low patient survival. This is due to the fact that the malignant tumor is asymptomatic, difficult to diagnose and early metastasizes to the lymph nodes, lungs and liver, and also quickly spreads through the perineural spaces and grows into the duodenum and colon, stomach and large vessels. In 52% of patients, it is detected in late stages - at the time of diagnosis there are already liver metastases. Early diagnosis is often an impossible task. Even with regular ultrasound, it is not always possible to detect cancer at an early stage.
Over the past 40 years, there have been few advances in diagnosis and treatment that would improve this situation. Despite the improvement of the surgical method and the performance of extended operations, they do not show benefits at those stages at which this disease is detected. Despite its rare occurrence (compared to malignant diseases of other locations - lung, stomach, prostate, colon and breast), mortality from pancreatic cancer ranks fourth in the world. In this regard, research is aimed at finding methods for early diagnosis and the most effective chemotherapy .
Benign pancreatic tumor
The causes of benign pancreatic tumors have not been established. They are believed to develop under the influence of the following factors:
- Genetic pathology predisposing to neoplastic processes;
- Unfavorable environmental conditions;
- Smoking tobacco;
- Alcohol abuse.
A large role in the development of benign tumors of the pancreas is played by inflammatory processes in the organ, primarily chronic pancreatitis. Risk factors for the development of benign tumors include poor nutrition - a predominance of fatty foods, mainly of animal origin, in the diet, lack of proteins, fiber, vitamins, and improper diet (overeating, lack of regular meals).
Tumors of the head of the pancreas manifest themselves as pain in the right hypochondrium and epigastric region, the body of the organ - in the upper abdomen, the tail - in the lumbar region and left hypochondrium. The mass may compress the pancreatic or common bile ducts. In this case, signs of obstructive jaundice appear:
- Icterus (yellowness) of the sclera and skin;
- Itching;
- The appearance of dark colored urine;
- Discoloration of stool.
If any part of the intestine is compressed, intestinal obstruction may develop.
Treatment of benign pancreatic tumors is only surgical. Resection of the head of the gland or tail is performed if there is a tumor in the corresponding part of the organ. If a large tumor is located in the area of the head of the gland and causes a violation of the outflow of bile, pancreaticoduodenectomy is performed - the tumor is removed along with part of the gland and the duodenum). An effective method of treating pancreatic hemangioma is selective arterial embolization - blocking the blood supply to the space-occupying lesion.
Consequences and complications
Complications include:
- Metastases to the lungs, lymph nodes and liver. Peritoneal metastases can compress the intestine and cause constipation or intestinal obstruction .
- The occurrence of thrombosis (with adenocarcinoma the risk is much higher than with squamous cell carcinoma).
- Stenosis and bleeding when the tumor grows into the stomach and duodenum.
- Hepatocerebral insufficiency , which is manifested by lethargy.
- Splenomegaly and bleeding from the veins of the esophagus when the tumor is located in the body or tail.
Treatment
Treatment tactics for pancreatic cancer are determined by its stage of development, location and size of the tumor focus. Both conservative and surgical methods are used for therapy. Among them are:
- Surgical operations. Oncologists distinguish several types of surgical treatment performed for pancreatic cancer. They differ in the scope of intervention. In accordance with this, total, partial or segmental resection is distinguished;
- Chemotherapy. Most often used in conjunction with radiation therapy. The essence of treatment is the introduction of drugs into the body that stop the growth of cancer cells. These medications do not have a selective effect. Therefore, oppression also affects healthy cells. The result is side effects;
- Radiation therapy. The main goal of this treatment method is to reduce the size of the tumor focus. Radiation therapy can be given both before and after surgery. In advanced stages of pancreatic cancer, radiation therapy is palliative;
- Symptomatic therapy. An essential part of comprehensive treatment for pancreatic cancer. Symptomatic therapy is designed to relieve the pain experienced by patients at all stages of treatment. For this purpose, narcotic and non-narcotic analgesics are used.
Forecast
Survival rates for patients with this pathology are very low due to the lack of diagnostic capabilities to detect the disease in its early stages. Despite the treatment, the prognosis for life expectancy for pancreatic cancer remains unfavorable. It all depends on the stage of the disease and the presence of gene mutations. In 80-90% of patients, the tumor turns out to be inoperable at the time of diagnosis (metastasis or invasion of nearby organs), which has a poor prognosis in the future. Survival also depends on the genetic profile. Tumors harboring DAXX or ATRX mutations are associated with poor prognosis. By studying the genetic profile, it is possible to identify in advance patients who need early and aggressive therapy. Expression of the SerpinB2 gene in the body of the gland in adenocarcinoma is not associated with metastasis, therefore such patients have long survival.
Treatment methods are also important in prognosis. After radical surgical treatment, survival rate does not exceed 15%, and the remaining patients die within 5 years after treatment. Therefore, the surgical method is supported by chemotherapy treatment. Combinations of several drugs significantly improve the prognosis.
How long can you live with pancreatic cancer? After surgical treatment, the prognosis remains unfavorable, since the relapse rate is 80-90%. Five-year survival after surgery is achieved by 25-30% of patients without metastases and only 10% of patients with metastases. If combined chemotherapy is administered after surgery, 29% of patients live 5 years. The type of tumor also affects life expectancy.
How long do people live with stage 4 pancreatic cancer? Since this stage is characterized by a metastatic process, the lifespan for stage 4 pancreatic cancer is 3-6 months. How do patients die? Departure from life is individual. Typically, patients develop severe pain that requires the prescription of narcotic drugs; all patients develop cachexia , which leads to protein-energy malnutrition. Protein deficiency reduces immunity, and the enzymatic function of the gland is further impaired. Decreased immunity increases the risk of infections. The presence of cachexia limits the ability to fully administer chemotherapy . Patients spend more time sleeping, and there is detachment, lethargy and apathy. We must try to organize good care for the sick to give them the opportunity to die peacefully.
Stages and prognosis
Identifying the stage of development of pancreatic cancer is important for determining further treatment tactics. In accordance with the classification, there are:
- 0 (TisN0M0): the tumor does not spread beyond the pancreas, there are no clinical symptoms;
- 1A (T1N0M0): a tumor with a diameter of up to 2 cm is localized within an organ, diarrhea, nausea or vomiting may occur;
- 1B (T2N0M0): the size of the tumor focus becomes more than 2 cm, dyspepsia persists;
- 2A (T3N0M0): the tumor grows beyond the pancreas, but does not affect the lymph nodes;
- 2B (T1-3N1M0): the cancer process spreads to nearby lymph nodes, a sharp loss of weight occurs, yellowing of the skin and visible mucous membranes and pain appear;
- 3 (T4N0-1M0): the tumor grows beyond the pancreas, affecting arteries, veins, and nerves;
- 4 (T0-4N0-1M1): the most severe stage, at which the cancer process affects distant lymph nodes and organs, metastases appear.
The prognosis for five-year survival depends on the stage at which the formation was detected. The earlier cancer is diagnosed, the higher the chances of successful treatment of the pathology.
Prevention
The basis of prevention is maintaining a healthy lifestyle and eliminating all possible risk factors.
Article sources:
- Pancreas cancer. Foltz E.E. Bulletin of medical Internet conferences No. 3, 2022. p. 146-151
- Diagnosis and treatment of pancreatic cancer. Patyutko Yu. I., Sagaidak I. V. Bulletin of the Russian Cancer Research Center named after. N. N. Blokhin RAMS No. 2, 2006. p. 36-37
- Difficulties in diagnosing pancreatic cancer. Evdokimova S.Yu. E-Scio, 2019
- Pancreatic cancer: indications for surgery. Keck T. Medical Council, 2010. p. 65-68
- Chronic pancreatitis and pancreatic cancer. Lazebnik L.B., Vinokurova L.V., Yashina N.I., Bystrovskaya E.V., Bordin D.S., Dubtsova E.A., Orlova Yu.N. Experimental and clinical gastroenterology, 2012. p. 3-9
- Genetic aspects of pancreatic cancer. Grigorieva I.N., Efimova O.V., Suvorova T.S., Tov N.L. Experimental and clinical gastroenterology, 2014. p. 70-76
- Diagnosis and surgical treatment of pancreatic cancer. Norbert Hüser, Volker Assfalg, Daniel Hartmann, Daniel Reim, Alexander Novotny, Edouard Matevossian, Helmut Friess. Experimental and clinical gastroenterology, 2011. p. 102-111
- Results of surgical treatment of pancreatic cancer. Mikhailov I.V., Bondarenko V.M., Kudryashov V.A., Prigozhaya T.I., Podgorny N.N., Shimanovsky G.M., Starinchik V.I., Novak S.V., Atamanenko A. .V., Dovidovich S.V., Kravchenko O.V., Nesterovich T.N., Achinovich S.L. Problems of health and ecology, 2014. p. 46-51
- The relationship between diabetes mellitus and pancreatic cancer. Kashintsev A.A., Kokhanenko N.Yu. Siberian Journal of Oncology, 2013. p. 36-39
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
Relapse and treatment tactics
The possibility of pancreatic cancer recurrence depends on the stage at which the disease was detected and the quality of treatment provided. It is impossible to accurately predict the possibility of tumor recurrence. Relapse is influenced by various provoking factors.
After completing treatment, it is important to follow your doctor's recommendations and attend regular preventive examinations. The tactics for managing a patient with a recurrent tumor depends on its location, size and stage of development of the tumor focus. For this, the same methods are used as for the primary disease.
How is jaundice treated?
A special case of the disease is concomitant jaundice due to compression of the common bile duct by a cancerous tumor, therefore, at the first stage, the outflow of bile is surgically restored, and after some time the issue of radical surgery is resolved.
Restoring the patency of the bile duct is possible in several ways, which are selected individually depending on the patient’s condition, the location of the lesion and its size: an expander is installed in the duct - a stent or catheter; a bypass route for the excretion of bile into the intestine is formed.
Nutrition for pancreatic cancer
Patients are prescribed table No. 5p. It is characterized by the following parameters:
- The calorie content of the diet does not exceed 1800 kcal;
- Carbohydrate content – up to 200 g;
- The amount of protein is 100-120 g, fat 80 g per day.
The diet is based on limiting extractive substances of plant and animal origin, which stimulate the pancreas. Nutritionists do not recommend foods with seasonings, foods rich in fiber, fatty fried foods, and foods that are high in fat.
If a patient suffering from pancreatic cancer has severe intestinal disorders, he is prescribed table No. 4 according to Pevzner. The calorie content of the diet is 1600 kcal. The patient receives 120 g of protein, 100 g of fat, and 200 g of carbohydrates per day. The menu includes the following dishes:
- Fish and meat soufflé;
- Low-fat cottage cheese;
- Weak tea;
- Bird cherry compote;
- Blueberry jelly;
- White steamed scrambled eggs or omelet, or soft-boiled egg.
The patient can eat decoctions of rice and buckwheat, meat and fish low-fat broths. Meals for stage 3 pancreatic cancer should be divided, 5-6 times a day, in small portions. All products are boiled, grilled or steamed.
A sample menu looks like this:
- Breakfast – fish soufflé, steamed egg white omelette;
- Second breakfast – low-fat cottage cheese;
- Lunch – pureed meat soup in low-fat broth, steamed minced meat;
- Afternoon snack – a glass of blueberry jelly or bird cherry infusion;
- Dinner – boiled meat (beef, chicken fillet), tea.
Products made from white flour are excluded from the diet of patients with pancreatic cancer. Patients are given gluten-free crackers. Strong meat broths, fatty meat and fish, fatty cheese and cottage cheese, various snacks, and seasonings are excluded from the diet. Patients are not recommended to consume milk, kefir, fermented baked milk, or add sour cream to dishes.
Signs of gland cancer
Cancer is detected mainly at stages 3-4. This is due to the absence of symptoms in the early stages. The tumor does not show any signs at all, and it is impossible to independently determine its appearance. Only an annual ultrasound or MRI will detect cancer when it is small.
The clinical picture can be varied. There are symptoms that indicate pancreatic cancer in patients over 55 years of age:
- sudden development of diabetes mellitus;
- jaundice without pain;
- constant pain in the stomach area with normal gastroscopy results.
When the head of the gland is affected, pain in the hypochondrium is characteristic, radiating to the back. They resemble those in chronic pancreatitis. The pain occurs when consuming fatty foods and intensifies at night. If you lean forward and bend your knees, it becomes easier.
The appearance of the skin of the legs may change - it becomes bluish due to the appearance of microthrombi.
As with other gastrointestinal tumors, with this type of cancer a person always loses weight. The loss is 10% or more even from the first stages, but not everyone notices the changes. After eating there is heaviness in the pit of the stomach. Fatigue, drowsiness, skin itching, nausea, vomiting are increasingly observed, feces become greasy and shiny.
Prevention of pancreatic cancer
To reduce the likelihood of developing pancreatic cancer, doctors have developed preventive recommendations. They include:
- Maintaining a rational and balanced diet. In the daily menu it is necessary to limit the amount of easily digestible carbohydrates and proteins. The products you choose should not contain nitrates;
- Active lifestyle. Adequate physical activity reduces the risk of obesity;
- Quitting smoking and excessive alcohol consumption. Chronic intoxication negatively affects the condition of the pancreas, stimulating the growth of tumor cells.
You can conduct a full course of diagnosis and treatment of pancreatic cancer in Moscow at the Yusupov Hospital. The clinic has the latest equipment and a professional team of doctors. Fast and accurate diagnosis allows you to identify cancer in the initial stages of development.
Diet
Diet for pancreatic cancer
- Efficacy: no data
- Timing: constantly
- Cost of products: 1500-1600 rubles. in Week
In the initial stages of the disease, patients can eat regular food and take pancreatic enzymes. Subsequently, most patients experience anorexia and malabsorption syndrome due to a violation of the exocrine function of the gland. High-fat foods are excluded from the diet of patients. The diet reduces the amount of fiber because it absorbs enzymes, reducing the supply of nutrients. Nutrition for pancreatic cancer should be organized as for any cancer, and it must be taken into account that its insufficiency in such patients only aggravates metabolic disorders.
When the patient's condition is severe or when they are unable to consume enough calories and with progressive weight loss, they resort to oral administration of mixtures intended for enteral nutrition, in small sips (siping) or through a tube. This is a type of therapeutic nutrition in which hypercaloric drinks and creams with increased taste provide cancer patients with reduced appetite with all the necessary substances.
The administration of liquid mixtures can stop weight loss and normalize nutritional status for further antitumor treatment programs. With a smaller volume of liquid, the mixtures have a high calorie content, they are balanced, enriched with vitamins and microelements, and contain omega-3 fatty acids. Currently, mixtures for oral administration have been developed, which are positioned as specifically intended for use in patients with cancer to prevent the development of cancer cachexia . These can be mixtures based on whey protein peptides ( Peptamen ) or a mixture with a high content of protein, omega acids, antioxidants and reduced carbohydrates ( Supportan Drink ).
If there are metastases
Spread of the tumor to nearby or distant organs without treatment is inevitable. Metastases spread through the blood and lymph, but more often they simply grow through the peritoneum. From the tail, cancer often grows into the spleen, from the head - into the liver and stomach.
Symptoms at this stage are not invisible, some are life-threatening:
- ascites - dropsy of the abdomen;
- girdle pain in the abdomen;
- refusal to eat and subsequent exhaustion;
- sharp enlargement of the liver and spleen;
- pale or yellowish skin;
- acute pain due to severe stretching of the spleen capsule;
- multiple nodes under the skin.
When the liver is damaged, the eyes and skin are constantly yellow, the stool is colorless, there is a painful odor from the mouth, and the gums bleed. Distant metastases can penetrate the brain and bones. This is expressed by pain in the corresponding localization, lameness, and focal symptoms. With metastases to the lungs there is a cough, hemoptysis, and shortness of breath.