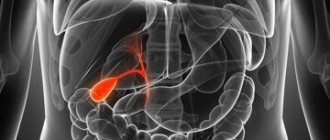
Classification of cholelithiasis
One of the latest classifications of cholelithiasis (GSD) was developed and adopted by the III Congress of the Scientific Society of Gastroenterologists of Russia for use in the clinic.
Stage I of cholelithiasis – initial, or prestone
- A. Thick heterogeneous bile
- B. Formation of biliary sludge: with the presence of microlites,
- with the presence of putty-like bile,
- combination of putty-like bile with microliths
Stage II – formation of gallstones
- A. By localization: in the gallbladder,
- in the common bile duct,
- in the hepatic ducts.
- single,
- cholesterol,
- latent (asymptomatic) course,
III. stage – chronic recurrent calculous cholecystitis.
IV. stage – complications.
Cholelithiasis. Initial stage - biliary sludge
Biliary sludge - what is it and what does it look like?
The term “biliary sludge” appeared in the 70s of the last century and came from English-language literature. Biliary - from the Latin word biliaris, which means bile, and sludge (English Sludge) - “suspension, dirt, mud, turbidity, silt, sand, ice porridge”, since there is no clear translation, the term sludge is used.
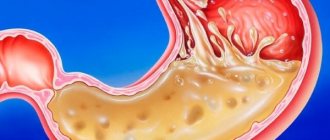
Currently, biliary sludge is understood as any heterogeneity of bile in the gallbladder and ducts, which is detected by ultrasound examination (ultrasound). Detection of biliary sludge is the initial stage of cholelithiasis, its prestone stage.
The first attempts to isolate the pre-stone stage of cholelithiasis were first made in the 70s of the last century, when scientists identified the initial stage of cholelithiasis, understanding by it biochemical changes in the quality of bile with subsequent physico-chemical disturbances in its structure, leading to the formation of cholesterol crystals and the formation of biliary sludge.
Progress in the study and diagnosis of the initial stages of cholelithiasis occurred when ultrasonographic examination (ultrasound) came into widespread practice, which made it possible to create a classification of cholelithiasis and identify types of biliary sludge. Currently, biliary sludge includes any heterogeneity of bile detected by ultrasound.
Main variants of biliary sludge
Echonic bile with clots
Bile with the presence of single or multiple areas of increased echogenicity, having clear or blurred contours, displaced, without an acoustic shadow (loose clots), often located along the posterior wall of the gallbladder.
Suspension of hyperechoic particles
Point, single or multiple, displaced hyperechoic formations that do not produce an acoustic shadow, detected when the body position changes.
Putty-like bile
Echo-heterogeneous bile with the presence of areas approaching the echogenicity of the liver parenchyma, displaced or fixed to the wall of the gallbladder, visible as a clear contour that does not give an acoustic shadow.
In clinical practice, in more than 70% of cases, biliary sludge variant 2 is encountered - a suspension of hyperechoic particles; the detection frequency of the other two sludge variants is 10-12%.
The sensitivity of ultrasound in diagnosing biliary sludge is 55-65%, and the specificity is more than 90%.
Among patients with complaints characteristic of damage to the biliary tract and gallbladder, biliary sludge is detected in 24-55% of cases.
ULTRASONIC DIAGNOSTICS OF GALLBLADDER DISEASES
The use of echography allows you to make a correct diagnosis in the shortest possible time, determine subsequent treatment tactics, and promptly begin conservative or surgical treatment. The paper outlines brief historical data on the use of ultrasound in medicine. Indications for ultrasound examination (echography) of the gallbladder, which reveals developmental malformations and diagnoses different diseases of the organ are given in details. The advantages of ultrasound examination over X-ray cholecystography are shown and the specific features of echograms are considered in different diseases of the gallbladder. The use of ultrasonography enables one to make a correct diagnosis at the earliest possible time, to define further treatment policy, to initiate medical or surgical treatment in time.
S.G. Burkov, Doctor of Medical Sciences, leading researcher at the Laboratory of Gastroenterological Research at the National Research Center of MMA named after. THEM. Sechenov SG Burkov, MD, Leading Researcher, Laboratory of Gastroenterological Studies, Research Center, IM Sechenov Moscow Medical Academy
IN
In recent years, a low-burden, highly informative ultrasound research method (synonyms: echography, sonography, ultrasonography), the diagnostic value of which has been confirmed by the works of many domestic and foreign authors, has become widespread in various fields of clinical medicine [1 - 4]. Ultrasound is elastic vibrations of particles of a material medium with a frequency of more than 20 kHz, i.e. above the threshold perceived by the human ear. Modern ultrasound equipment is based on the principle of echolocation, and all diagnostic devices operate in pulse mode. It is important to know that in the emission mode the device’s sensor operates only 0.1% of the cycle time, while in the receive mode it works 99.9%. This rhythm of work is one of the factors determining the safety of ultrasound examinations. Echography is not associated with ionizing radiation, which distinguishes it favorably from, for example, computed tomography and classifies it as a harmless technique (echography is approved for use during pregnancy due to the absence of possible damaging effects on the fetus). The first successful attempt to use ultrasound in medicine was made by the Austrian neurologist Karl Dussick in 1942. However, the systematic use of echography for diagnostic purposes began only in the mid-60s. In a relatively short period of time, ultrasound diagnostics has gone from one-dimensional echography, which provided a very small amount of information, to complex real-time scanning, which allows visualization of not only organs and systems, but also their structural elements. The resolution of modern ultrasonic devices is 0.1 mm, which determines the high accuracy of the method. The first report of the use of echography to detect gallbladder diseases was made by Ludwig and Struthers in 1950, and today it is the leading method for diagnosing diseases of the biliary system. Typically, an ultrasound examination of the gallbladder is performed in the morning on an empty stomach after an overnight fast, no earlier than 12 hours after a meal. In emergency cases, the study can be carried out without prior preparation. For patients with flatulence, concomitant intestinal pathology, 1 - 2 days before the study, it is advisable to exclude from the diet foods that increase bloating (black bread, legumes, sauerkraut, whole milk, grapes, etc.), prescribe enzyme preparations (digestal, Creon 1 - 2 tablets 3 - 4 times a day with meals).
| Rice. 1. Echogram of a normal gallbladder. | Rice. 2. Echogram of the gallbladder with two bends. | Rice. 3. Echogram of the gallbladder with a bend and constriction. |
| Rice. 4. Echogram of a deformed gallbladder. | Rice. 5. Echogram of the gallbladder in acute cholecystitis (the gallbladder is enlarged, the wall has a double contour, the contents are heterogeneous). | Rice. 6. Echogram of the gallbladder with a stone. |
| Rice. 7. Echogram of the gallbladder with two stones. | Rice. 8. Echogram of the gallbladder with sediment (marked with an arrow). | Rice. 9. Echogram of a disconnected gallbladder (the bladder filled with stones is marked with an arrow). |
| Rice. 10. Echogram of cholesterosis of the gallbladder (cholesterol polyps are marked with arrows). | Rice. 11. Echogram of the gallbladder in a patient with ascites. 1 - ascitic fluid; 2- gallbladder; 3 - liver. | Rice. 12. Echogram of the gallbladder in a patient with acute viral hepatitis. 1st day of jaundice (wall thickness 13 mm, volume 1.1 cm3). |
The examination is usually carried out with the patient lying on his back with a breath hold during the deep inspiration phase, if necessary, on the left side, sitting or standing. Normally, the gallbladder is defined as a clearly contoured, free from internal structures, echo-negative formation of a pear-shaped, ovoid or cylindrical shape, located in the right upper quadrant of the abdomen (Fig. 1). Its size varies widely - the length ranges from 6 to 9.5 cm, and the width (diameter) does not exceed 3 - 3.5 cm. The wall of the bladder is represented by a fairly uniform thin (no more than 2 mm) line of moderately increased echogenicity. The outer and inner contours of the bubble are clear and even. As our studies have shown [5], the density of the walls changes (increases) with age. This is explained by the fact that after 60 years, the mucous membrane and muscle layer atrophy and connective tissue gradually develops in them, the wall of the bladder becomes sclerotic and thickens. Therefore, the density of the bladder wall should always be correlated with the age of the subject. Experience in the use of echography shows that it can be successfully used to identify developmental anomalies and diagnose various diseases of the gallbladder. Echographically, partitions, kinks and deformations of the bladder are easily detected. In some regions, kinks are detected in 60 - 75% of those undergoing examination [2], while on echograms the gallbladder can take on a different, sometimes bizarre shape (Fig. 2 - 4). Ultrasound is one of the main methods for diagnosing gallbladder dyskinesia, acute and chronic cholecystitis. With hypomotor dyskinesia, the bladder can be either normal size or enlarged. In the absence of cholecystitis, its wall is not changed. To assess the functional state, motor-evacuation function of the gallbladder, first measure its volume (V) on an empty stomach (in modern devices this parameter is determined automatically) or calculated using the formula proposed by F. Weill [4]: V = P (p/2)2 • l, where p is width, l is length. Then, after taking two egg yolks at equal 5-10 minute intervals, determine the volume of remaining bile over 1.5-2 hours if they want to track the full cycle of emptying and relaxation of the bladder. The motor activity of the gallbladder is considered normal if the volume decreases by 50 - 70% by the 45th minute. In everyday practice, in a simplified version, you can limit yourself to measuring the largest diameter of the bladder on an empty stomach and at the 45th minute, as radiologists do. It should be noted that the data on the motor activity of the gallbladder obtained from oral and ultrasound cholecystography completely coincide. Therefore, to identify gallbladder dyskinesia, it is advisable for patients to undergo ultrasound rather than X-ray (associated with radiation, administration of contrast agents) cholecystography. In acute cholecystitis, the gallbladder may be enlarged, normal, or even reduced in size, and one of the main echographic signs is wall thickening and the appearance of a double contour (Fig. 5). In this case, sharp pain is detected when the device sensor presses on the area of projection of the gallbladder (positive ultrasonic Murphy's sign). Using echography, it is possible to identify complications of acute cholecystitis: empyema, gangrene, wall perforation. The following signs are most characteristic of chronic cholecystitis: compaction and thickening of the wall, unevenness and deformation of the contour of the bladder, decreased or absent movement during breathing, inhomogeneity of the contents, “bile” sediment, positive ultrasound Murphy’s sign. To establish a diagnosis of chronic cholecystitis, it is certainly necessary to compare the results of ultrasound with the clinical signs of the disease. Echography is of greatest importance for diagnosing cholelithiasis; the accuracy of the method reaches 98 - 99% (the accuracy of oral cholecystography does not exceed 70%). A stone in the gall bladder looks like a dense formation, followed by an ultrasonic shadow, located, as a rule, on the back wall of the bladder, shifting when the patient’s body position changes (Fig. 6, 7). The smallest size of stones diagnosed by ultrasound is 1 - 2 mm. In some cases, it is possible to detect sediment (sand) in the gallbladder (Fig. 8). It should be noted that the size of the stones on ultrasound does not correspond to their true size; they look somewhat larger. With multiple stones, it is not always possible to determine their exact number. Unfortunately, echography does not allow us to determine the composition of the stone (pigment or cholesterol) or the degree of its calcification. Ultrasound allows you to diagnose a disabled gallbladder when it is filled with stones, and free bile in the lumen is not detected. In this case, in the area of the projection of the bubble, a conglomerate of dense echo structures is visualized, giving an acoustic shadow (Fig. 9). Echography allows you to diagnose hypertrophic diseases of the gallbladder, such as adenomyomatosis and cholesterosis. The polypoid form of gallbladder cholesterosis is especially well identified (Fig. 10), and it is always necessary to carry out a differential diagnosis with cholelithiasis. The main difference is that the cholesterol polyp(s) do not produce an acoustic shadow and do not move when the patient's body position changes. Note that in patients with ascites, on echograms the gallbladder protrudes into the ascitic fluid, is atonic, the contents are often heterogeneous, the walls are dense, thickened, and a double contour appears (Fig. 11). Primary cancer of the gallbladder is considered a fairly rare disease; it mainly occurs in elderly and senile patients who have suffered from cholelithiasis for a long time. Although clinical recognition of this suffering is extremely difficult, the accuracy of ultrasound diagnosis is 86 - 88%. It is interesting to note that by examining the gallbladder, a diagnosis of acute viral hepatitis can be established with a high degree of reliability. It has been proven that in the first days of jaundice, the volume of the gallbladder decreases sharply (from 3 - 4 cm3 to 0.5 - 1.0 cm3), while the wall appears sharply thickened (Fig. 12). Thus, echography provides significant assistance in the diagnosis and differential diagnosis of gallbladder diseases. Summarizing the data presented in this article, we can conclude that the indications for ultrasound examination of the gallbladder are: suspicion of impaired motor-evacuation function, typing the type of dyskinesia; acute and chronic cholecystitis (determining the functional state of the bladder, the condition of the walls, size, shape, presence of anomalies); suspicion of cholelithiasis (detection of stones in the gall bladder); jaundice of various origins (to determine the genesis of jaundice, differentiate obstructive jaundice from parenchymal jaundice); pancreatitis of various origins (to identify a concomitant disease, and in case of reactive pancreatitis - the main one). The use of echography allows you to make a correct diagnosis in the shortest possible time, determine subsequent treatment tactics, and begin timely conservative or surgical treatment.
Literature:
1. Clinical guide to ultrasound diagnostics / in 2 volumes, ed. V.V. Mitkova. / Volume I M.: Vidar, 1996. - 336 p. 2. Clinical ultrasound diagnostics: A guide for doctors in 2 volumes. Ed. N.M. Mukharlyamova. - M.: Medicine, 1987. - Volume I. - 328 p. 3. Dvoryakovsky I.V., Chursin V.I., Safronov V.V. Ultrasound diagnostics in pediatrics. - L.: Medicine, 1987. — 160 s. 4. Weill FS. Ultrasonography of digestive diseases. Second edition. St. Louis - Toronto - London. The CV Mosby Co, 1982. 5. Burkov S.G. Changes in the biliary system /according to echography/ in elderly and senile patients // Rus. honey. magazine. - 1996. - Vol. 4. - No. 7. — P. 418-20.
Gallstone disease stage II. Causes and factors for the formation of cholesterol stones
Among the reasons contributing to the formation of biliary sludge (BS), there are four main groups of risk factors that characterize gallstone disease.
Factors contributing to the oversaturation of bile with cholesterol:
- Age, often female, during pregnancy the contractile function of the gallbladder often suffers, which contributes to the formation of biliary sludge, heredity.
- Taking oral contraceptives and estrogen-containing drugs during menopause increases the risk of gallstone formation by 2-2.5 times. Calcium supplements increase the risk of developing BS.
- Excess body weight is an important risk factor for BS, contributing to increased cholesterol synthesis and its excretion through the biliary tract. It should be noted that low-calorie diets, which are used for weight loss, in 25% of cases are accompanied by the formation of BS and the formation of stones.
- Nutrition. Foods low in dietary fiber slow down its movement through the intestines, increase the absorption of secondary bile acids and change the quality of bile. Eating fatty foods containing a lot of cholesterol and refined (purified) foods increase the level of cholesterol in the bile. Small doses of alcohol, on the contrary, reduce its content in bile.
- Liver diseases. With viral hepatitis A, B, G, TTV, an opinion is expressed about the possibility of the formation of gallstones. Diseases of the small intestine (celiac disease, resection of the small intestine), Crohn's disease, etc. disrupt all types of metabolism, including the absorption of bile acids.
- Impaired contractile function of the gallbladder is one of the leading factors in the formation of biliary sludge and stone formation.
Thus, supersaturation of bile with cholesterol is a prerequisite for the formation of BS, but not the only one. An important role is played by the disruption of the quality of bile, all its components, the formation of mucus and the deposition of cholesterol crystals, and disruption of the contractile function of the gallbladder.
Diagnosis of biliary sludge
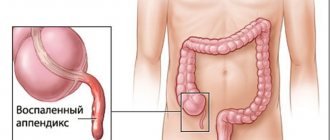
Biliary sludge (BS) can be a source of stone formation in the gallbladder, a cause of biliary pancreatitis, a marker of early cancer of the gallbladder, stenosing papillitis (duodenal papilla through which bile enters the intestine).
Biliary sludge (thick bile with microlites) passes through the entire human biliary system, which has a huge number of pain receptors and causes pain.
- Clinical manifestations are similar to those of dyskinesia; they are described in detail here in the paragraph “Biliary dyskinesia - clinical manifestations.” The long-term existence of BS not only causes clinical manifestations and contributes to the development of complications such as: acute cholecystitis, “disabled gallbladder”, cholangitis (inflammation of the bile ducts), acute pancreatitis. Biliary sludge can also be asymptomatic, but given the prognostic features - the possibility of stone formation, which can subsequently lead to surgical treatment - removal of the gallbladder, examination of the gallbladder and biliary tract should be included in the clinical examination program.
- Biochemical liver tests, pancreatic enzymes of blood, urine, feces.
The main method of examination is ultrasound, which should be carried out after 3 days of preparation for a routine examination or for urgent indications. Ultrasound examination of gallbladder function. More details in the ultrasound section.
Esophagogastroduodenoscopy (GDS) with mandatory examination of the major duodenal papilla!
- Modern diagnostic methods - hepatobiliscientigraphy with 99mTc, magnetic resonance cholangiopancreatography (MRCP), bile microscopy are carried out in specialized hospitals.
Bend diagnostics
Diagnosing a bend is not difficult. The most informative method for diagnosing pathology is ultrasound. It allows not only to identify pathology, but also to determine the functional state of the organ, the exact location of the bend, and also to evaluate the anatomical features of the walls, neck, and body.
Determining the cause of the pathology is more difficult. To differentiate a congenital disease from an acquired one, an ultrasound examination of the gallbladder is performed twice: on an empty stomach and after eating egg yolks, which cause increased secretion of bile. When the inflection of the bladder is a congenital pathology, the deformation of the organ remains unchanged.
Treatment and prevention of biliary sludge
Therapeutic tactics are discussed with the attending physician, taking into account clinical manifestations, ultrasound examination data, duration of existence, and causative factors of biliary sludge.
1 group of patients
If eliminating the causative factor leads to the disappearance of BS, then drug treatment may not be required; it is enough to streamline your diet and reduce body weight. But if the patient does not have clinical manifestations of BS, but BS persists on ultrasound for 3 months, then a course of conservative treatment is indicated.
Group 2 patients
Based on the pattern of gallstone formation and the appearance of complications, therapeutic measures are required, based on the characteristics of the course and manifestations of BS.
Group 3 patients
Patients with a high risk of developing purulent complications that sometimes require surgical intervention.
All patients with biliary sludge should follow a diet - eating every 3-4 hours. Not to starve! The diet should be balanced, contain proteins, carbohydrates, fats (depending on the function of the gallbladder), dietary fiber (bran, pectin, grains, vegetables).
The main objectives of conservative therapy for patients with biliary sludge:
- improving the quality of bile,
- elimination of dysfunctions of the gallbladder and sphincter of Oddi, duodenum, small and large intestines,
- normalization of digestion and absorption,
- correction of the normal composition of intestinal microflora.
To solve these problems, the course of conservative treatment includes different groups of drugs. The basic drug is ursodeoxycholic acid drugs, choleretic drugs, antispasmodic drugs, enzyme preparations, a course of antibacterial drugs according to indications, biological drugs (Enterosan).
The course of conservative treatment is determined by the doctor based on the results of the examination individually, taking into account concomitant diseases and therapy for them, the results of dynamic studies of the effectiveness of treatment.
The duration of the course is from 1 to 3 months or more, and then transition to preventive treatment (dietary regimen, individual nutrition, short courses of choleretic drugs according to indications, probiotics, “on demand” enzymes, antispasmodics.
Do you need a diet?
A bent gallbladder is a fairly common problem.
Dietary nutrition is designed to alleviate the main symptoms of the pathology and help restore impaired organ function. The diet involves adherence to the principles of fractional nutrition, which will ensure normal outflow of bile and prevent stagnation. The patient is recommended to eat small portions of 250-300 grams at least five times a day.
The therapeutic diet involves the inclusion of protein products of plant origin, a small amount of vegetable fats and butter in the diet. The consumption of animal fats, products containing essential oils, for example, garlic, onions, radishes, radishes, etc., hot sauces and marinades, vegetable pickles, smoked meats and fish, fatty soups and broths, whole milk, easily digestible carbohydrates, etc. As for the heat treatment of dishes, it is important to give preference to boiled and baked dishes, fried foods irritate the gallbladder and liver and significantly increase the symptoms of the pathology.
It is important to ensure that the patient drinks plenty of fluids. The approximate daily fluid intake is 1.5-2 liters.
Cholelithiasis. Clinical symptoms
Asymptomatic cholelithiasis can be a finding of ultrasound examination during medical examination or manifest itself as symptoms of damage to other organs and systems.
Symptomatic cholelithiasis can manifest itself as pain in the upper abdomen, attacks of biliary colic, obstructive jaundice, and biliary dyspepsia.
The pain can be dull, aching, and often an attack of biliary colic occurs, which is a pathognomonic sign of cholelithiasis.
Biliary colic is characterized by sharp, spastic pain that intensifies with inhalation and positioning on the left side, and decreases slightly on the right side. The patient is tossing about in bed due to pain, there is tachycardia (palpitations), increased sweating, nausea, slight vomiting that does not bring relief to the patient, and bloating. With biliary colic, the pain is localized in the right hypochondrium or epigastric region, radiating under the scapula on the right, or the collarbone. Pain can radiate to the chest and to the heart area, simulating pain in the heart (angina) - cholecystocardiac reflex.
An attack of biliary colic requires emergency care, the pain should not be tolerated, an ambulance must be called, possibly hospitalization, an assessment of the patient's condition and indications for surgical treatment or conservative management of the patient are given.
After biliary colic, which can last from ten minutes to several hours, jaundice may appear - yellowness of the sclera and skin, darkening of urine, discolored feces.
Simultaneously with or without an attack of biliary colic, biliary (bilious) dyspepsia may occur, which is manifested by a feeling of bitterness in the mouth, nausea, especially in the morning, sometimes vomiting that does not bring relief, bloating, and a tendency to constipation. These phenomena are transient and can occur independently or during an attack of pain in the right hypochondrium.
Correct and timely diagnosis allows you to clarify the disease, exclude the involvement of other digestive organs and complications and outline adequate ways to manage the patient
Treatment
People with congenital bending of the bladder can live with it all their lives and discover the pathology by chance during an ultrasound of the abdominal organs. In such cases, the pathology does not require treatment. Treatment for a bent bladder that appears as a result of any disease takes quite a long time. The patient is prescribed medication, physiotherapy and mandatory adherence to a gentle diet.
Drug treatment involves taking choleretic drugs, which must be taken in courses. The duration of each course is 10-14 days, but you need to complete at least four courses. Most often, for the treatment of pathology, gastroenterologists prescribe the drug Flamin, the active ingredients of which are flavonoids and glycosides of immortelle sandy, Odeston, which accelerates the evacuation of bile into the intestinal lumen and relieves spasm of the bile ducts, Aritohol, Chophytol, Tsikvalog, etc.
Physiotherapy is effective in the treatment of biliary obstruction. To relieve symptoms of pathology, electrophoresis with novocaine and ultrasound are prescribed. After symptoms are relieved, it is advisable to attend physical therapy groups.
Folk remedies are a good addition to traditional methods of treatment. The use of certain medications can alleviate the patient's condition and speed up recovery. As a rule, to normalize the function of the bladder and improve the outflow of bile, decoctions and infusions of medicinal herbs that have a choleretic effect are used. Such herbs include corn silk, calendula, peppermint, chamomile, etc.
Cholelithiasis. Indications for surgical treatment
If stones have formed in the gallbladder, there are two treatment approaches:
- try to dissolve them, if these stones are “soft” cholesterol,
- surgical treatment.
Drug dissolution of gallstones
X-ray negative cholesterol stones are treated with urosodeoxycholic acid preparations under the following conditions:
- the size of the stones does not exceed 15-20 mm in diameter,
- with complete preservation of the contractile function of the gallbladder,
- absence of stones in the common bile duct,
- filling the gallbladder with stones up to half its volume,
- complete patency of the cystic duct.
Contraindications for dissolving stones are:
- radiopaque stones, stone diameter more than 2 cm,
- frequent attacks of biliary colic,
- non-functioning gallbladder,
- acute cholangitis, liver diseases,
- chronic pancreatitis,
- peptic ulcer (especially for henofalk),
- inflammatory diseases of the large and small intestines,
- diabetes,
- pregnancy.
Indications for surgery
- frequent attacks of biliary colic,
- the presence of chronic calculous cholecystitis,
- non-functioning gallbladder,
- large size kamnpi,
- development of complications.