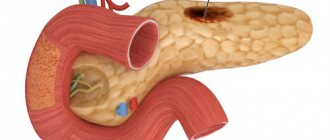
Diseases of the pancreas (pancreatitis, neoplasms, cysts, stones in the ducts) are accompanied by disruption of the general digestive process. And the resulting change in the synthesis of hormones (insulin and glucagon) that regulate blood glucose levels affects the metabolism of the entire body. Therefore, it is important to use the diagnostic capabilities of pancreatic pathology to provide assistance and prevent dangerous consequences.
We will look at how to check the pancreas using available methods. How advisable it is to use the entire scope of diagnostics depends on the patient’s condition and the capabilities of the nearest medical institution.
We warn the reader that the specific choice of method or necessary tests for examining the pancreas remains with the doctor. The same applies to the interpretation of results and conclusions.
Working with the patient
People who underestimate the clarification of a sick person’s complaints and the importance of a personal examination by a doctor are very mistaken. Of course, each person describes his sensations as best he can, but the information received is no less valuable for diagnosis than instrumental research.
Results of patient questioning
The main complaints indicating pathology of the pancreas are:
- stomach ache;
- dyspepsia (nausea, loose stools, bloating, vomiting);
- yellowness of the skin;
- general weakness;
- significant weight loss.
The characteristics of the pain syndrome are described by the patient quite clearly:
- short-term cramping pain is possible 3-4 hours after eating fatty foods or long-term intense pain lasting several days;
- often poorly treated with antispasmodic drugs;
- localization - epigastric zone or left hypochondrium, radiates to the back, covers the entire upper abdomen, patients emphasize the “encircling” nature.
Sudden and very intense pain is characteristic of acute pancreatitis. They are caused by blockage of the main excretory duct of the gland due to inflammation and swelling of the surrounding tissue.
Overstimulation of the solar plexus plays a role in the pain mechanism
What matters about tumors is their persistence and aggravation in the supine position. If cancer of the head of the gland is suspected, the patient describes pain in the hypochondrium on the right, spreading to the back, body and tail - pain in the epigastrium, left hypochondrium, “encircling” character is typical. Prolonged aching pain is possible with chronic pancreatitis. When figuring out what helps during an attack, the patient shows a typical half-bent posture.
Dyspepsia is associated with impaired enzyme composition of digestive juice and a reflex response of other organs.
Patients complain:
- for poor appetite;
- aversion to food, especially fatty foods;
- constant nausea;
- bloating;
- diarrhea with the release of feces, covered with a shiny membrane (“fat stool”), with a fetid odor.
..
Yellowness of the skin has a brownish or greenish tint, accompanied by severe itching of the skin, hemorrhages (bruises). If the patient complains of such signs, then without blood tests it is possible to preliminarily diagnose a tumor in the head of the pancreas or the consequences of chronic pancreatitis (organ sclerosis).
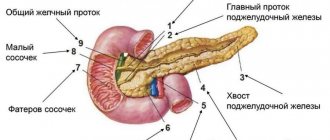
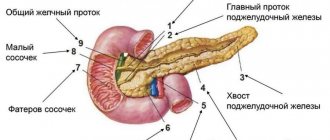
The symptom is caused by compression of the common bile duct leaving the liver. A situation arises when, to check the pancreas, it is necessary to examine the liver and gallbladder. Diagnosis of pancreatic diseases involves identifying the factors contributing to the occurrence of pathology.
The patient must be asked:
- about diet and passion for fatty foods;
- drinking alcohol;
- presence in the medical history of data on chronic cholecystitis;
- hereditary predisposition to tumor growth.
Evaluation of inspection results
Examination of the patient, when carried out skillfully, provides the necessary data for diagnosis. Acute pancreatitis is characterized by pale skin with areas of cyanosis (consequences of intoxication and damage to the capillaries).
With cancer, the patient is exhausted, the skin is yellowed, dry with traces of scratching and hemorrhages. Abdominal bulging and bloating are often noticeable. It is very difficult to palpate a painful abdomen. The abdominal muscles are tense. Maximum pain is observed in the epigastrium, less often in the left hypochondrium.
It is possible to palpate an enlarged gland only in 4–5% of cases in female patients, and in 1–2% of male patients. Instead of an even horizontal cylindrical formation, a dense, lumpy strand is determined. During palpation, parts of neighboring organs can be mistaken for the pancreas:
- stomach;
- transverse colon;
- enlarged lymph nodes.
The peculiarity of the organ requires taking into account both exocrine and hormonal functions
Home diagnostics: what symptoms to look out for
At home, it is impossible to conduct a full diagnosis of pancreatic diseases. But knowledge of the main symptoms of its damage is necessary in order to recognize the disease in time and go to the clinic.
Pain
You can find out about the presence of gland pathology at home by the nature of the pain.
Intense pain in the left hypochondrium and epigastric region occurs more often after simultaneous consumption of alcohol and fatty foods. Growing rapidly, they spread to the area of the scapula, lower back, and right hypochondrium. The pain intensifies when a person takes a horizontal position with his stomach up.
The fetal position and applying a cold object to the gland area helps to relieve pain.
During an attack of pancreatitis, pain cannot be relieved with conventional analgesics.
Nausea, vomiting, indigestion
Nausea and vomiting indicate the need to check the condition of the pancreas. Their occurrence is associated with self-poisoning of the body by pancreatic enzymes produced in excess. Severe intoxication occurs when the gland ducts narrow, when enzymes do not enter the intestinal lumen, but begin to digest organ tissue.
In acute pancreatitis, debilitating vomiting does not bring relief. Vomit contains impurities of bile, mucus, particles of undigested food, and coagulated blood. A bitter taste remains in the mouth.
The chronic form of pancreatitis is often accompanied by constant nausea. Failure to follow a diet, excessive physical activity or stress provoke attacks of exacerbation, during which vomiting occurs.
Change in skin color, itching
The reason to check the pancreas and liver is a change in the color of the mucous membranes, skin, cornea of the eyes, as well as rashes and itching.
Characteristic symptoms of dysfunction of important digestive organs include the appearance of icteric and cyanotic spots against the background of general pallor of the skin.
Of particular danger is cyanosis (blue discoloration) of the skin in the navel and chest area, which precedes an attack of acute pancreatitis or an exacerbation of its chronic form.
Excessive pallor of the skin indicates anemia and severe intoxication; jaundice indicates compression of the bile ducts and destruction of the liver parenchyma. These shades can also be signs of breast cancer.
Exacerbation of chronic pancreatitis is often accompanied by the appearance of:
- bruises around the navel, on the thighs and in the groin area;
- vascular angiomas, which look like deep red spots and are located on the back, abdomen and chest;
- urticaria on the back, buttocks and anterior surface of the lower extremities.
Severe itching, accompanied by rashes, frequent urination, thirst, and an acetone odor from the mouth, indicates type 1 diabetes.
Increased body temperature
You can check the condition and determine the stage of inflammation of the pancreas by measuring your body temperature:
- Edematous pancreatitis. Temperatures may rise slightly to subfebrile levels and remain for three days.
- Hemorrhagic pancreatitis. As a result of self-digestion of the gland, penetration of pancreatic enzymes and toxins into the blood, the temperature rises to 38-39°C.
- Total and subtotal pancreatic necrosis. At this stage, a purulent abscess forms, inflammation spreads to neighboring organs, fistulas and cysts form, and bleeding occurs. Temperatures reach 40°C and there is a high probability of death.
An increase in temperature during remission of chronic pancreatitis indicates an inflammatory process and the need for urgent medical attention.
Of particular danger is a decrease in temperature, accompanied by a drop in blood pressure, anemia and weak pulse. These symptoms indicate intoxication or internal bleeding.
Weight loss, lack of appetite
The first sign of inflammation or cancer of the gland is sudden weight loss. This is due to several reasons:
- frequent nausea, leading to decreased or complete absence of appetite;
- vomiting, preventing food from entering the body;
- lack of entry into the intestines of pancreatic enzymes involved in the breakdown and absorption of nutrients;
- removal of vitamins, minerals and other food components in undigested form.
Without receiving the required amount of energy, the body begins to break down glycogen and subcutaneous fat. Replenishment of protein deficiency occurs by removing them from muscle tissue. Gradually this leads to dystrophy.
Change in natural functions
Due to the fact that pancreatic enzymes do not enter the duodenum, carbohydrates and lipids cease to be broken down, pieces of food are excreted undigested, and diarrhea occurs. The feces become discolored, liquid, and foul-smelling. The resulting steatorrhea (fatty stool) often indicates the presence of a malignant tumor in the pancreas.
Urine with pancreatitis turns dark due to increased levels of amylase and bilirubin.
Other signs
Signs of incipient gland disease may be:
- flatulence;
- belching, accompanied by the smell of acetone or an unpleasant taste;
- dizziness, loss of consciousness;
- excessive dryness of the skin;
- decreased visual acuity.
What studies are included in the diagnostic scheme?
If, during questioning and examination, signs suspicious for pancreatic diseases are identified, the doctor prescribes a full examination of the pancreas. For this we use:
- blood test for biochemical tests;
- biochemical examination of urine, revealing the level of diastase;
- stool analysis for scatology to identify undigested food residues, fats (steatorrhea);
- Ultrasound helps in detecting the size, shape, tumors and cysts;
- diagnostic tests provide information about the impaired functional abilities of the organ;
- X-rays, magnetic resonance imaging (MRI) and computed tomography of the pancreas and neighboring organs are used as additional sources in the search for indirect signs;
- tissue biopsy.
How to diagnose acute pancreatitis?
For acute pancreatitis, health care workers examine the fluid by puncturing the abdominal wall. Laparoscopy is prescribed - an operation performed using a laparoscope through small openings in the internal organs. An endoscopy and x-rays are also performed. Ulcers are found using radiography or tomography. Examinations are carried out in different ways, taking into account the patient’s well-being.
Diagnosis of pancreatitis involves taking blood, stool and urine tests. Patients are prescribed radiography and fluoroscopy. To find out the causes of the disease, a comprehensive examination of the internal organs is carried out. Patients undergo tests of stool, saliva, urine, as well as a blood test for pancreatitis.
The importance of biochemical tests of blood and urine for enzymes
Methods for examining the pancreas usually begin with the most simple laboratory tests. The essence of their results is the identification of increased levels of specific enzymes in the blood and urine, which have entered an unusual environment due to impaired outflow of secretions into the duodenum.
[node:field_field_doprekl]
An increase in the concentration of enzymes indicates pancreatic pathology:
- lipases,
- amylase,
- trypsin.
The pancreas produces about 20 enzymes. But most often, patients are recommended to donate blood and urine for the first 2 types; trypsin is rarely tested.
Amylase normally enters the blood in small quantities from the salivary glands. In 78% of patients with pancreatitis, amylase levels are increased by 2 or more times. Biochemical methods for detecting amylase are based on the reaction of starch breakdown. Wolgemuth and Smith-Roy methods are used.
The result of the determination of amylase is electrophotocolorimetry of the colored compound
Lipase is determined by stalagmometry. It shows the change in surface tension generated by fatty acid lipase in a sensitive tributyrin solution. The blood contains several types of lipases. In the diagnosis of the pancreas, the ethoxyl-resistant type is of greatest importance; it is elevated in 90% of patients.
It is important to evaluate both results; if amylase is elevated and lipase is at normal levels, you need to think about another pathology. A blood test is taken on an empty stomach. Urine should be collected in a clean container. No special preparation is required. If necessary, an analysis is performed to examine the pancreas for emergency indications at any time of the day.
It makes sense to check the endocrine function of the gland to maintain optimal blood glucose levels with the help of insulin and glucagon in all patients, since experience shows that it is impaired in 75% of patients with pancreatitis and tumors.
The study is carried out using methods of determining blood glucose once on an empty stomach, testing for glucose tolerance with stress tests, and assessing glucosuria in 24-hour urine.
How is stool examination performed?
If there is loose stool, a stool test for scatology is prescribed. Both macroscopic signs (consistency, smell, color) and a smear under a microscope are examined. You can identify the consequences of impaired digestion: undigested muscle fibers (from meat foods), neutral fat.
If pancreatic pathology is suspected, examination should establish steatorrhea. Up to 15 g of fat per day is quantitatively detected from the intestinal contents, although normally it contains only 6 g (94% is absorbed). In the feces of chronic pancreatitis, a decrease in chymotrypsin activity is detected.
Possible diseases of the pancreas
Depending on the cause of occurrence, all gland diseases are divided into the following categories:
- inflammation (acute and chronic pancreatitis);
- oncology (benign and malignant tumors);
- stones (calcifications);
- cysts;
- pseudocysts;
- functional disorders (endocrine insufficiency, diabetes mellitus);
- parasitic infestations;
- infectious processes (syphilis, tuberculosis);
- pathologies of the vascular system;
- pancreatic necrosis.
Among the neoplasms, insulinoma of the pancreas is considered separately, the diagnosis of which is difficult due to symptoms that are not specific to diseases of this organ.
Ultrasound capabilities
Ultrasound examination has found wide application in practical healthcare. It is especially significant with the ability to check the pancreas without any tests when the organ is located deep.
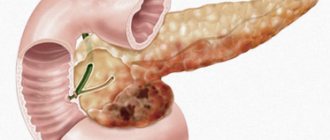
The complexity of ultrasound is due to the individual characteristics of the location and size of the gland, the presence of gases in the intestines. Therefore, in 10% of subjects it is not possible to identify the organ. This is especially true for overweight patients. The method confirms the presence and location of the tumor in 80% of cases, and diagnoses cysts in almost 100% of cases if they are more than 15 mm in size.
[node:field_field_doprekl2]
General rules for preparing for analysis
Before you take pancreatic tests, you need to know how to do it correctly. Doctors usually instruct patients because errors in collecting biological material can lead to significant deviations in the results obtained.
General recommendations come down to several points:
- Studies are carried out on an empty stomach, in the first half of the day. A few days before the tests, you should avoid junk food (fried, spicy, fatty, salty, canned food, coffee, alcohol, carbonated drinks). It is also not recommended to consume legumes that can cause increased gas formation;
- Before taking blood, you must refrain from smoking for at least two hours;
- For problems such as constipation, care should be taken to ensure that toxins retained in the intestines do not affect the test result;
- All containers must be sterile and hands must be thoroughly washed with soap;
- When collecting urine, women must perform genital hygiene, after which it is better to use a tampon to guarantee the purity of the collected material;
- To study a general urine test, you need to take an average portion.
These simple recommendations will help you get tested correctly and avoid possible false results. However, it is worth remembering that sometimes laboratories make mistakes, so if you have the slightest doubt, you should undergo the examination again.
How are diagnostic tests performed?
Examination of the pancreas, if necessary, can be supplemented with diagnostic tests to identify non-hormonal functions of the organ (exocrine). All methods are divided into:
- those requiring the use of an intestinal tube;
- non-invasive (probeless).
The advantage of tests (especially probeless ones) is convenience for the patient and low cost.
The disadvantage of the tests is that results appear only with a significant decrease in the secretory capacity of the pancreas, so they are considered insensitive
The following tests are used in practice:
- pancreozymin-secretin;
- Lund test;
- hydrochloric acid;
- elastase.
Pancreozymin-secretin test
For the patient on an empty stomach, a probe is inserted into the duodenum with two holes. Aspiration of gastric and duodenal secretions is carried out step by step. Then secretin and pancreozymin are administered intravenously. After the injection, new samples are taken to study the concentration of bicarbonates and trypsin activity. The rate of secretion is calculated.
Pancreatitis is characterized by a decrease in secretion, a decrease in the level of bicarbonates, and an increase in the concentration of enzymes. It is possible to identify false-positive data in patients with diabetes mellitus, biliary tract dysfunction, hepatitis and cirrhosis of the liver.
Lund test
It is distinguished by the use of a standard food mixture as a food irritant to the gland. In the morning, the patient is inserted into the duodenum with a weight attached to the end, through which a food mixture (vegetable oil, milk powder with dextrose) is inserted. Sample aspirates are collected within two hours. Then the level of amylase in them is determined. The option is simpler and cheaper, and does not involve injections.
Hydrochloric acid test
It differs from the previous ones in the type of irritant used - a solution of 0.5% hydrochloric acid in olive oil. Further actions are the same. The disadvantages are general.
Elastase test
Based on the study of elastase in the patient’s stool. Gives a positive result for chronic pancreatitis, liver diseases, gallstones, diabetes.
How to check the pancreas in the clinic
Despite the manifestation of characteristic symptoms, an accurate diagnosis of the gland is only possible in a clinical setting.
Palpation of the abdomen
The initial examination of the pancreas includes inspection, palpation and percussion.
With pancreatitis, superficial palpation of the abdomen reveals painful tension in the abdominal muscles in the area of the left hypochondrium and epigastrium.
A deep examination of the pancreas by palpation is very difficult due to the delicate consistency of the organ and its deep location. Therefore, palpation is carried out only on an empty stomach in the morning after preliminary use of a laxative.
Normally, the gland is palpable in the form of a soft, stationary cylinder, the diameter of which does not exceed 3 cm. With inflammation and tumors, it takes the form of a dense cord with uneven contours.
Blood tests
To check the pancreas, you need to donate blood for clinical and biochemical analysis.
When the gland is inflamed, there is an increase in the number of band and segmented neutrophils. When the process is complicated by a purulent infection, the leukocyte formula shifts to the left. An increase in ESR serves as a characteristic indicator of the presence of a focus of inflammation in the body.
Biochemical blood parameters during laboratory diagnosis of the gland, indicating problems:
- ALT - more than 45 U/l;
- AST - more than 40 U/l;
- amylase - exceeds 50 U/l tens of times;
- elastase, lipase - more than 190 U/l;
- trypsin - more than 60 µg/l;
- glucose (fasting) - more than 5.5 mmol/l.
C-reactive protein also appears in the blood, which is absent in a healthy body. When the liver is involved in the pathological process, the level of bilirubin and alkaline phosphatase increases.
There are no specific methods for diagnosing pancreatic cancer based on blood counts. The presence of a malignant tumor can be suspected by a significant decrease in the level of hemoglobin and platelets. If the cause of malignant formation in the pancreas is hepatitis C or B, then the ESR decreases sharply.
Urine and stool tests
Urinalysis is the main method to check the functioning of the pancreas. An increase in the level of alpha-amylase (another name is “urine diastasis”) above 64 U/L in a single collection or 600 U/L in all portions per day indicates pancreatitis.
A sharp decrease in urine diastase to 100 U/l indicates the death of significant areas of the organ and the development of pancreatic necrosis.
Coprogram is an informative method for diagnosing gland pathologies. Deviations from the norm when assessing external indicators of feces:
- liquid or semi-liquid consistency;
- marsh, greenish, yellow color;
- foul odor;
- greasy shine;
- additional inclusions in the form of strands of mucus, blood, pus, and unprocessed pieces of food.
Microscopic examination of stool reveals:
- vegetable fiber;
- muscle fibers;
- starch grains.
Fatty acids are identified using staining. If appropriate reagents are available, the laboratory additionally performs a quantitative assessment of pancreatic enzymes.
Ultrasound
Ultrasound diagnostics of the gland reveals:
- change in the contours of the affected organ;
- the presence of areas of parenchyma degeneration;
- neoplasms;
- stones, other foreign inclusions;
- the nature of diffuse tissue changes;
- violation of the echogenicity of structural elements.
Diagnosis of the liver and pancreas using ultrasound is also aimed at detecting stones in the gall bladder or blockage of the excretory ducts.
Biopsy
If a tumor is detected on ultrasound, the specialist directs the patient to check for pancreatic cancer using a biopsy. It is carried out using a fine-needle puncture method, followed by examination of preparations from the affected tissues under a microscope. This is a very accurate differential method. diagnosis of pancreatic formations, on the basis of which a final diagnosis is made.
Endoscopy
An informative method for diagnosing tumors of the pancreas and biliary tract is endoscopy. It makes it possible to identify cancer, scar tissue degeneration of the pancreatic and bile ducts, and their blockage with stones.
X-ray
X-ray diagnostics of pancreatic diseases makes it possible to detect compactions and mechanical inclusions in the parenchyma and ducts of the organ.
CT and MRI
The most accurate examination method is an MRI of the pancreas. With its help, the doctor examines the structure of the organ layer by layer, identifying pathological changes. The study must be carried out before surgery, as well as when assessing the quality of treatment during the rehabilitation period.
Computed tomography is prescribed if cysts, neoplasms, or metastases are suspected.
Other instrumental methods
Additional methods for diagnosing the gland include:
- Endoscopic cholangiopancreatography. It is based on the detection of a contrast agent localized in tumor tissues.
- Selective angiography. It consists of an X-ray examination of the vessels of the affected organ after the administration of a contrast agent.
Sometimes it becomes necessary to check pancreatic function using stress tests (iodolipol, proserine, secretin-pancreozymin). The patient is administered a specific drug, and after a certain period of time its appearance in the blood or urine is assessed.
X-ray signs
An x-ray of the abdominal organs may reveal indirect signs or consequences of damage to the pancreas. These include:
- rare detection of stones or lime salts in the pancreatic ducts at the level of the upper lumbar vertebrae (a sign of chronic pancreatitis);
- a large cyst in the form of a homogeneous formation with clear boundaries;
- deformation and displacement of the bend of the duodenum with an enlarged head of the pancreas;
- filling defects along the posterior wall or greater curvature of the stomach with a tumor (cyst) in the body or tail area.
In order to improve visibility, before the examination, the patient is injected with an atropine solution, which reduces the tone of the duodenum, then a barium suspension is administered through a probe.
X-ray is not a very suitable method for examining the gland
A more targeted study is retrograde pancreatography, Wirsungography. The contrast must be injected directly into the pancreatic duct. Then photographs are taken that reveal its expansion or sharp narrowing to a complete break (stone). Angiographic examination is highly complex. In this case, a contrast agent is injected through a catheter into the aorta and celiac artery through the femoral approach.
What does a tissue biopsy provide?
The biopsy method means taking a sample of pancreatic tissue for histological examination. This is an uncommon procedure. It is carried out as a last resort in order to exclude cancer, in differential diagnosis.
It can be an independent study or part of the surgical procedure. This requires special equipment and needles. The tool looks like a pistol with a knife end for cutting tissue.
The biopsy is performed under the control of computed tomography under local anesthesia; if the suspected tumor is small, it is difficult to get into it
Using the laparoscopic method under anesthesia, the doctor inserts a thin endoscope into the abdominal cavity, examines it for metastases, the size of the infiltrate during inflammation, and effusion into the peritoneum. A tissue sample is taken with special forceps. During surgery, material can be collected from the head of the gland using a needle through the duodenum.
Further histological examination allows us to confirm or reject the assumption of a malignant lesion, shows the degree of the inflammatory reaction, and the replacement of functioning tissue with scars. To examine such a complex organ as the pancreas, one method is not enough. The doctor needs the results of a comprehensive study, his own examination and analysis of complaints.