Types of enterocolitis
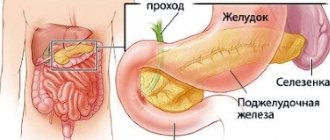
Enterocolitis is a condition caused by inflammatory processes in the small and large intestines.
Spicy option. Inflammation does not spread to deep tissues; the intestinal mucosa usually suffers. Usually the condition is combined with acute gastritis. Acute enterocolitis can have different origins.
There are infectious and non-infectious nature of the course. In addition to infectious diseases, allergic conditions and various poisonings (medicines or poisons) can be provoking factors.
Chronic enterocolitis. Such a diagnosis can be made to a patient after poor or insufficient treatment of an acute condition. Chronic enterocolitis is dangerous because the deep layers of the intestine are involved in the inflammatory process. This disease causes serious disturbances in the functioning of the intestinal tract. The classification of the disease depends not only on the specifics of enterocolitis, but also on the type of provoking cause.
Bacterial infection is responsible for the development of bacterial enterocolitis. Pathogenic flora are salmonella and staphylococcus. Parasites can also cause inflammation. Giardia, Trichomonas and helminths provoke the development of parasitic enterocolitis. Toxic enterocolitis is provoked by various poisonings.
The prevention of intestinal diseases is proper nutrition. Lack of nutrients in food and abuse of harmful foods contribute to the formation of alimentary enterocolitis. Frequent constipation is dangerous; it is responsible for the development of mechanical enterocolitis.
A person who has problems with the gastrointestinal tract may develop secondary enterocolitis.
Grocery list
If treatment of gastrointestinal diseases using the fourth table according to Pevzner is carried out at home, be sure to have an accurate list of foods allowed and prohibited for this diet.
If some foods and dishes are in doubt, the best option is to consult with your doctor.
Why does enterocolitis occur?
Infection with helminths is one of the factors of enterocolitis.
Several factors are responsible for the formation of this disease:
- The course of acute intestinal infections;
- Infection with helminths;
- Deviation from the basics of healthy eating: undereating or overeating;
- Allergies to foods, medications (often the body reacts to taking antibiotics);
- Existing diseases of the gastrointestinal tract;
- Immunity disorders;
- Dysbacteriosis, vitamin deficiency.
As a result of the predominance of pathological microflora in the human body, a chronic course of enterocolitis begins to form. There is a pattern: enterocolitis and dysbiosis are interrelated conditions.
Recipes for diet number 4
Steamed fish balls from carp fillet.
Ingredients: 1 egg, 20 g wheat bread, 80 g carp fillet. Pass the carp fillet through a meat grinder, add wheat bread pre-soaked in water and squeezed out, salt and egg, mix, pass through a meat grinder and beat thoroughly. Steam the cut meatballs.
Pike perch meatballs.
Ingredients: 50 ml water, 15 g butter, 15 g rice, 120 g pike perch. Cook and cool the sticky rice porridge. Pass the porridge together with the pike perch pulp through a meat grinder twice, add about five grams of melted butter, beat well, form into meatballs and steam until cooked.
Steamed meatballs with rice.
Ingredients: 20 g rice, 100 g beef. Turn the prepared meat through a meat grinder three times. Rice must be washed, sorted and boiled. After the rice has cooled, you need to rub it through a sieve and add it to the minced meat, then add salt and beat thoroughly. Cut the mixture into balls and steam.
Liquid semolina porridge on water.
Ingredients: 5 g butter, 5 g granulated sugar, 250 ml water, 50 g semolina. Gradually pour semolina into boiling water, stirring it constantly, add granulated sugar and salt, cook over low heat for 15-20 minutes. Before serving, add a piece of butter.
Mashed potatoes.
Ingredients: 50 ml water, 5 g butter, 200 g peeled potatoes. Wash the peeled potatoes, cook them in salted water until tender, drain the water. Grind and mash the potatoes, dilute with hot water and add butter.
Dried blueberry drink.
Ingredients: 15 g granulated sugar, 250 ml water, 20 g dried blueberries. Rinse the dried blueberries with cold water, add hot water, and boil for 10-15 minutes. Leave for 3-4 hours, then strain the drink and add sugar.
Symptoms
Rumbling in the stomach is one of the main symptoms of this disease.
The main symptom that interferes with the normal life of patients with enterocolitis is diarrhea. It is accompanied by other unpleasant phenomena - flatulence, nausea, problems with appetite, a feeling of fullness in the abdomen.
If the small intestine suffers more, the patient complains of aching pain in the lateral peritoneum. Acute enterocolitis develops rapidly and is characterized by the following symptoms:
- Rumbling in the stomach;
- Nausea, vomiting;
- Pain in the abdominal area;
- Coated tongue;
- Diarrhea.
When diagnosed with “infectious colitis”, other unpleasant symptoms are added to the listed symptoms:
- Temperature increase;
- Weakness;
- Muscle pain and headaches;
- Intoxication.
In the chronic course of the disease, during the period of remission, the patient feels tolerable, but during an exacerbation, unpleasant sensations again remind themselves:
- Stomach ache;
- Stool disorders;
- Fast weight loss;
- Bloating;
- Dyspepsia.
Recommendations
In order to correctly follow table number 4, you need to know some of the nuances of preparing dishes and consuming a number of products:
- Cook soups only with low-fat, non-concentrated broth. If possible, they should be slimy and not thick.
- Porridge - ground. Cook mainly in water, with the addition of a small amount of milk.
- Remove all fat layers, tendons, skin and fascia from meat and fish. You cannot serve it in pieces - only minced through a meat grinder, which must have a minimum hole diameter.
- Allowed vegetables are only after heat treatment. Preferably in soups. In limited quantities.
- Milk cannot be drunk separately, only when added to dishes (porridge, omelettes, puddings).
- Non-carbonated mineral water of a certain brand is prescribed by the attending physician.
It is not easy to follow treatment table 4, since you will constantly want to chew something hard, in one piece. Mashed potatoes and grated porridges quickly get boring. However, it is even more difficult to prepare dishes for him, since there are too many prohibitions and nuances.
It is for this reason that this diet is recommended to be followed in a hospital or medical sanatorium. A professional nutritionist will be able to correctly calculate both the daily calorie intake and the BJU ratio and provide for the daily intake of salt, sugar and oil. At home, it is extremely difficult to take into account all these details and do everything correctly. And every mistake can result in a worsening of the patient’s condition.
How is chronic enterocolitis treated?
To treat chronic enterocolitis, you need to establish a nutritional regimen and an appropriate diet.
To alleviate the patient’s condition, it is necessary to cope with the cause that provokes the progression of the inflammatory process in the intestines. The following events are shown:
- Setting a nutritional regime and an appropriate diet;
- Stop taking medications that aggravate the situation;
- Getting rid of parasitic or bacterial infection;
- Therapeutic procedures related to gastrointestinal diseases.
- When the root cause causing this condition goes away, measures are taken to get rid of dysbacteriosis and correct digestive disorders.
- Using a diet gives good results. Outside of exacerbations, diet 2 is prescribed; diet 3 will help regulate bowel function and eliminate constipation; if the patient is bothered by diarrhea, diet 4 is prescribed.
- With obvious progression of dyspepsia, foods responsible for putrefactive processes are limited: meat, fish, fermented milk products, coarse fiber. You should refrain from eating rye bread, whole milk, sugar and cabbage.
- If the small intestine suffers, it is worth enriching the table with proteins, microelements and vitamins. It is worth removing products that have a negative effect on the mucous membranes. It is better for patients with enterocolitis to avoid sour, fried, spicy and salty foods.
- To improve the chronic inflammatory process, drug therapy is used.
- Antibacterial agents (furazolidone, enterofurin) will help get rid of pathological microflora;
- Such therapy necessarily includes taking enzymes containing drugs;
- Prescription of prebiotics and probiotic preparations is indicated.
- A good effect is achieved by means that normalize intestinal motility.
- Herbal enemas have proven themselves to be excellent as a local treatment. St. John's wort, bird cherry and oak help get rid of diarrhea. Sea buckthorn can help with constipation, and chamomile is said to be the best remedy against flatulence.
- Vinilin is used as a wound healing agent for the development of ulcers or erosions. It helps stop bleeding. The disease can bring psychological suffering, so consultation with a psychiatrist will alleviate the patient’s condition.
- For patients with bowel problems, consultation with a physiotherapist is recommended. In the treatment of enterocolitis, manipulations that help cleanse the intestines, magnetic therapy and reflexology are used.
- High results are obtained by visiting balneological resorts and staying in sanatoriums. The general condition improves and the results obtained from the main treatment are consolidated.
At the moment of exacerbation of the disease, a person must reduce activity and devote all his efforts to improving the condition. The period of remission should be accompanied by regular exercise; aerobics has a positive effect on overall well-being. The digestive system begins to work smoothly if the patient is inclined to an active lifestyle. It is worth abandoning traumatic sports that can injure a vulnerable area.
Patients are shown exercises for the abdominal muscles: they help regulate pressure and have a beneficial effect on the intestines.
Nutrition and Inflammatory Bowel Disease: General Questions
DIETS STUDYED IN IBD
As we said earlier, the Pevzner diet No. 4 has not been studied for IBD. But it is clinical studies that currently form the basis for proving the effectiveness (or ineffectiveness) of a particular treatment method, incl. and diets. The most “weighty” in evidence-based medicine are randomized clinical trials (in which patients have the same opportunity to receive the study or control drug (comparator or placebo)), systematic reviews and meta-analyses of clinical trials (conducts a summary analysis of studies on a specific problem).
Of course, there are other types of research, but their results cannot be considered as a guide to action. In particular, quite a lot of surveys of patients with IBD have been published regarding foods that they tolerate well or poorly. Back in 2012, a group of American researchers led by Cohen AB published the results of such a survey (more than 2300 patients with IBD). Yogurt and rice were most often associated with a decrease in the severity of symptoms of the disease, while a huge list of foods (vegetables, legumes, seeds, nuts, milk, alcohol, fried foods, etc.) were associated with worsening health according to patients. The authors conclude that a large list of poorly tolerated products may indicate individual intolerance, i.e. improvement or worsening of intestinal symptoms does not at all indicate a decrease or increase in inflammatory activity.
Clinical studies on dietary therapy for IBD are few, but this does not reduce their value. Below we look at the main diets that are offered to patients with ulcerative colitis and Crohn's disease.
Low-FODMAP diet.
The acronym FODMAP stands for a group of fermentable (F) carbohydrates – oligo- (O), di- (D) and monosaccharides (M), as well as polyols (P); The English word “low” means that in this diet these carbohydrates should be reduced or eliminated. These carbohydrates are poorly absorbed in the small intestine, have high osmotic activity and are actively broken down by intestinal bacteria. As a result, a significant amount of gases is formed, and due to osmotic activity, loose stools, abdominal pain, and rumbling can develop.
FODMAP carbohydrates include lactose, fructose, fructans and galactans, as well as polyols (polyhydric alcohols).
Insufficient activity of lactase, the enzyme that breaks down the milk sugar lactose, is a common situation in adulthood. In addition, lactase activity may decrease during exacerbation of Crohn's disease with damage to the small intestine, bacterial overgrowth syndrome (SIBO), intestinal resections, etc.
Fructose is found in large quantities in honey, fruits, and corn syrup. The absorption of fructose depends on the presence of glucose, so products in which the ratio of fructose to glucose is 1:1 are absorbed quite well. products in which the amount of fructose is significantly greater than glucose (apples, mangoes, pears, cherries, artichokes, etc.) are poorly absorbed, which can cause the symptoms described above. Fructans are carbohydrates found in foods such as wheat, onions, garlic, etc. They are not absorbed in the intestine.
Galactans are also carbohydrates that are practically not absorbed in the intestines due to the lack of the necessary enzyme. They are found in beans, red beans and lentils. Polyols are found in some vegetables and fruits, mushrooms, as well as in sweeteners (xylitol, sorbitol, etc.), which can be added to chewing gum, cough drops, and syrups (including medicinal ones).
The low-FODMAP diet consists of eliminating foods high in these substances from the diet (effectiveness is assessed over a period of 3-6 weeks, although the effect usually occurs sooner).
Traditionally, this diet has been recommended for patients with bloating and irritable bowel syndrome (IBS), but has subsequently been evaluated in IBD. There are few controlled studies assessing the effectiveness of the low FODMAP diet for acute IBD. One of the few randomized studies of the effects of a fructooligosaccharide elimination diet was performed in 103 patients with active Crohn's disease. Unfortunately, there were no significant differences in achieving remission or clinical response compared with placebo.
Regarding the effect of the low-FODMAP diet on gastrointestinal symptoms in patients with IBD in remission, encouraging results were obtained. A meta-analysis (as the most reliable type of clinical evaluation of effectiveness) conducted by Zhan YL et al in 2022 showed that symptoms such as loose stools, bloating, abdominal pain, nausea and vomiting were significantly less severe in patients with the disease Crohn's and ulcerative colitis in remission if they followed a low-FODMAP diet. A recent study by SRCox et al. (2020) demonstrated a decrease in the severity of IBS symptoms in patients with ulcerative colitis and Crohn's disease in remission, but the IBS severity index did not differ significantly in the comparison groups.
Thus, we can recommend this diet (including modifications in the presence of individual intolerance to certain foods) to those patients with IBD in remission who have bloating, occasional abdominal pain, and nausea. Naturally, after excluding complications and exacerbation of the disease.
Specific (special) carbohydrate diet (SUD), in the English version - specific carbohydrate diet.
SUD was developed and proposed by the American pediatrician Sidney Valentine Haas back in 1924 for patients with celiac disease. Much later, the diet gained popularity among patients with ulcerative colitis thanks to the book “Breaking the Vicious Cycle: Gut Health through Diet” by biochemist Elaine Gottschall. This diet is based on the assumption that some carbohydrates (disaccharides and polysaccharides), when insufficiently digested and absorbed, cause the growth of opportunistic bacteria in the intestine, which not only changes the qualitative and quantitative composition of the intestinal microbiota, but also helps maintain the inflammatory process in the intestinal mucosa.
Complex carbohydrates (found mainly in cereals and potatoes) are excluded from the diet and simple carbohydrates such as glucose, fructose and galactose are limited. The diet requires strict adherence, but for most patients it is quite difficult to adhere to it for a long time. In this regard, an open study of SUD in children suffering from mild to moderate IBD is indicative (Cohen SA et al., 2014). 38% of participants were unable to begin the study for various reasons, of which half of the cases were due to the “excessive strictness” of the proposed diet.
As of 2022, the information available on the effectiveness of SUDs in IBD is limited by the poor quality of studies: these are either online surveys, or retrospective assessments of symptoms and tests, or a small number of patients in the study groups. To date, several small studies have shown a reduction in Crohn's disease symptoms in pediatric patients. More significant are studies that evaluate not only the symptoms of the disease, but also the healing of the gastrointestinal mucosa. At the time of publication of this article, a comparison of SUD and the Mediterranean diet in patients with Crohn's disease is being conducted, but the work has not yet been completed and the results of the study have not been published.
Summary : Despite the fact that, in general, many patients noted an improvement in symptoms (continuing to receive basic therapy), a number of patients were forced to abandon the diet due to difficulties in adherence to it and weight loss. The results of studies on SUD should be recognized as encouraging, but larger studies are required to recommend it to patients with exacerbation of IBD.
Paleolithic diet or paleo diet.
This type of diet was proposed by gastroenterologist Walter L. Voegtlin, who in his work described the basic principles of the paleo diet. The Paleo diet is an approach to nutrition that consists primarily of plant and animal foods and is based on the supposed ancient diet of humans during the Paleolithic (a historical period that ended approximately 10,000 years ago). The modern Paleolithic diet consists of foods available today and includes fish, meat and poultry, preferably grass-fed, vegetables, fruits, rhizomes and nuts. Excluded from the diet:
- cereal grains (including quinoa);
- legumes;
- dairy products;
- eggs;
- seeds (including coffee, as well as spices such as coriander, cumin, seed products - vegetable oils);
- vegetables of the nightshade family (tomatoes, sweet peppers, hot peppers, eggplants, potatoes)
- food colorings, food additives
- sugar and sweeteners (such as stevia)
- alcohol.
This diet is even more difficult to follow, and restricting a large list of important foods can cause nutritional deficiencies.
In the English-language literature you can also find the name of this diet as “autoimmune protocol” or autoimmune protocol, which is a modification of the paleo diet.
Available research regarding the effectiveness of the Paleo diet and autoimmune protocol for ulcerative colitis and Crohn's disease is limited. In 2022, the results of the only work studying the effect of an autoimmune protocol on the activity of IBD in 15 (!) patients were published. It was shown that among patients who followed the diet and received therapy (including biological therapy), in some cases there was a decrease in the severity of symptoms and a decrease in the activity of inflammation according to endoscopic examination. The authors believe that controlled studies are needed to confirm the effectiveness of this diet.
Anti-inflammatory diet.
One of the mechanisms for the development of IBD, as mentioned above, is the development of dysbiotic disorders, including under the influence of food components. Undoubtedly, the greatest role belongs to carbohydrates, which are a nutrient substrate for bacteria (including opportunistic ones) of the intestine. The anti-inflammatory diet includes 5 steps:
- Modification of the carbohydrate composition of the diet (including lactose and refined carbohydrates)
- Introducing foods with prebiotic activity into the diet (soluble fiber, onions, fermented foods)
- Emphasis on consumption of polyunsaturated and saturated fats
- Assessment of food intolerances, identification and correction of nutritional deficiencies
- Modification of culinary processing (for example, wiping food and dishes as necessary). In patients in the acute phase, this phase begins simultaneously with the first.
The diet consists of lean meat, poultry, fish, eggs, selected fruits and vegetables, flour, nuts and legumes, a limited amount of aged (with active enzymes) cheeses, fresh yogurt, kefir, honey, etc. Prebiotics come in the form of soluble fibers (containing inulin - bananas, oats, ground chicory root and flaxseed meal).
The authors of the diet published the results of a study in 2014, according to which 33% of patients were unable to comply with it. Among the remaining patients, a decrease in endoscopic activity of IBD (both Crohn's disease and ulcerative colitis) was observed. Scientists have suggested that this diet may have an effect on IBD activity, but controlled studies are required.
Elimination diets for Crohn's disease.
Elimination diets usually refer to diets from which individual foods or food groups are excluded. To date, there are works that are devoted to assessing the effectiveness of an elimination diet for Crohn's disease. It involves eliminating a number of foods that provoke the appearance or intensification of symptoms of the disease in a particular patient. results
studies were summarized in the conclusion of ESPEN experts and voiced in recommendations for dietary therapy for IBD: there is no convincing evidence of the effectiveness of any elimination diets for Crohn's disease and ulcerative colitis.
It should be noted that a recent randomized controlled trial of an elimination diet combined with partial enteral nutrition (50% enteral formula nutrition) showed the effectiveness of the nutritional approach in achieving remission (including without steroids) of Crohn's disease in children. The diet was well tolerated and was more effective than total enteral nutrition.
CD-TREAT diet (Crohn's disease treatment with eating).
This diet is essentially an approach to nutrition that mimics the effects of total enteral nutrition. It has long been known that in children with mild Crohn's disease, taking only enteral formulas (without natural food) increases the likelihood of achieving remission. The authors of the diet studied a diet based on ordinary foods, the composition of which was close to the composition of the enteral formula (Modulen mixture was taken as a sample). This diet recreates the effect of full enteral nutrition by eliminating certain components (eg, gluten, lactose, and alcohol). At the same time, macroelements, vitamins, minerals and fiber were retained in the same quantities as in the enteral formula. Maltodextrin, an artificial glucose polymer—the most common form of carbohydrate in enteral formulas—is not found in natural foods, so it has been replaced by high-starch, low-fiber foods. Patients received microelements by taking additional multivitamins.
We currently have data on the effect of this diet on the microbial composition of the intestine and the content of some key molecules in the stool (primarily short-chain fatty acids) in adult volunteers. The CD-TREAT diet significantly reduced fecal calprotectin levels in children with Crohn's disease.
Summary : This diet appears to have promise for use in Crohn's disease, but additional randomized controlled trials are required.
Other diets.
In addition to the listed diets, many different diets have been and are being studied - a diet high in fiber and limited in simple carbohydrates, diets high in omega-3 fatty acids, a diet with limited calcium, etc. Alas, the quantity and quality of work leaves much to be desired. A 2022 comprehensive analysis of the results of studies of these diets did not show their effectiveness in inducing and maintaining remission, reducing the number of operations and healing the intestinal mucosa.
Acute enterocolitis
In acute enterocolitis, gastric lavage is used.
Severe manifestations of acute inflammation require hospitalization. The type of enterocolitis affects the distribution of patients - they can end up in infectious diseases departments or be treated in poison control centers. Therapy involves bed rest. Treatment of different types of acute enterocolitis involves:
- Gastric lavage. The procedure can be performed with or without a probe. Boiled or distilled water is used. Sometimes sodium bicarbonate is used.
- Intestinal cleansing with a saline laxative is practiced, then enteresorption is carried out. Patients take 5 grams several times a day. enterodesis (per 100 ml of water); Polyphepan is prescribed in a dosage of 10-15 g. Pediatric therapy prefers activated carbon or lignosorb.
What procedures work against intoxication? A mild degree of contamination with toxins requires a special drinking regimen; severe disorders require the appointment of infusion therapy. To relieve symptoms, it is better for the patient to fast and drink more fluids. Relaxation is allowed on day 2 - you can eat liquid soups and cereals. Improvement in well-being entails a gradual expansion of the patient's table.
Treatment of infectious enterocolitis requires the prescription of antiviral drugs, antiparasitic agents and antimicrobial compounds. For disinfection measures, Quiniofon, Quezil, Intestopan, Enteroseptol, Chlorquinaldol, Mekaza have proven themselves well. Acute conditions can be stabilized on day 7. Relief occurs on the second day.
Nutrition for diarrhea (diarrhea)
- Food should be taken at least 4-5 times a day at the same hours.
- All food is only boiled or steamed; frying food is prohibited. Cold and hot dishes are not allowed.
- Table salt is somewhat limited, all dishes are under-salted.
- Drink 1.2 – 1.5 liters of liquid.
Method of preparation and consumption of products: for example, raw pureed apples help normalize stool, and when taken as part of a mixed diet, they enhance intestinal motility, and fats taken in a mixture with other products (porridge, vegetable purees) have practically no laxative effect.
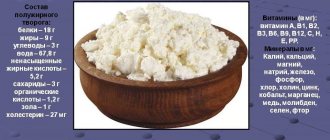
Features of nutrition during illness
During illness, you can consume dairy products and lean meat.
Products allowed for consumption:
- Dairy products: cream, milk, cheese, cottage cheese, kefir, yogurt, a small amount of sour cream.
- Eggs: omelet, soft-boiled.
- Oils: butter, vegetable (it is better to choose olive oil).
- Porridge: the best option is semi-viscous boiled cereal in water. It is allowed to add milk in small quantities.
- Small and large ones are welcome on the menu.
- Baked goods: day-old bread, savory rolls, dry cookies.
- Soups with a second broth with the addition of cereals and vegetables.
- Lean meat. The best cooking method is boiling. Frying process is allowed.
- Sauces.
- Vegetable dishes: puddings, cutlets, casseroles. Preferred vegetables: potatoes, beets, zucchini, cauliflower and carrots. Individually, tomatoes, peas or white cabbage may be allowed.
- Fruits: jelly, jellies, compotes. Some patients are allowed: watermelons, oranges, grapes.
- Tea, cocoa, coffee.
- Sweets: honey, sweets, jam, sugar.
- Possible snacks: cheese, fish aspic, ham, boiled sausage, fish and vegetable caviar, vegetable salads.
Excluded from the diet:
- Warm yeast products.
- Fatty fish, meat.
- Smoked, salted, pickled products.
- Pork lard.
- Cold drinks, ice cream.
- Spicy seasonings.
- Chocolate.
- Berries with rough skin.
- Grapes, kvass.
- Vegetables: garlic, cucumbers, radishes, radishes, sweet peppers and legumes.
Menu for the week: what you can eat
Options for a weekly menu for each meal according to the “4 table” diet:
1st breakfast options:
- oatmeal with water, soft-boiled egg, tea;
- semolina porridge with water, rosehip decoction, small crackers;
- rice porridge with water, 100 grams of lean pureed cottage cheese, tea;
- semolina porridge with water, steam omelette, tea;
- buckwheat porridge with water, 1 boiled egg, apple broth;
- rice pudding with egg, low-fat cottage cheese, tea;
- steamed buckwheat pudding with cottage cheese, fresh apple puree, green tea.
Options for 2nd breakfast:
- a portion of low-fat cottage cheese;
- applesauce;
- quince jelly;
- dogwood jelly;
- baked apple;
- blueberry decoction, crackers;
- warm blueberry and bird cherry jelly.
Lunch options:
- low-fat meat broth with semolina, rice and steamed chicken quenelles, apple broth;
- rice soup with meatballs, buckwheat porridge, turkey cutlets, quince broth;
- chicken broth with rice and egg flakes, boiled rabbit meatballs, pureed buckwheat, blackcurrant infusion;
- pureed rice, potato and carrot soup, veal meatballs, compote;
- slimy soup with rolled oats and egg flakes, steamed pollock fillet meatballs, tea;
- semolina soup with chicken fillet meatballs, crackers, rosehip infusion;
- potato-semolina soup, boiled rabbit, compote.
Afternoon snack options:
- quince jelly;
- jelly, small cracker;
- warm jelly, a small cracker;
- oatmeal jelly;
- semolina pudding;
- rice water;
- decoction of pears, crackers.
Dinner options:
- potato and zucchini puree, softened boiled hake fillet;
- steam omelette, rice and fish meatballs, green tea;
- pureed rice porridge, steamed lean fish dumplings, tea;
- one poached egg, buckwheat porridge puree, green tea;
- curd and rice casserole, boiled veal soufflé, rosehip infusion;
- curd pudding, soft-boiled egg, oatmeal jelly;
- rice porridge with sugar and a piece of butter, 1 poached egg, green tea.
Options for the night:
- rosehip decoction;
- carrot juice (diluted);
- oatmeal-blueberry jelly;
- apple juice (diluted);
- jelly.
From the above dish options you can create a varied diet for every day.