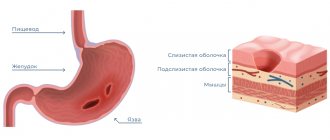
From a modern point of view, peptic ulcer is a chronic disease of the stomach or duodenum, occurring with cyclic alternations of exacerbations and remissions.
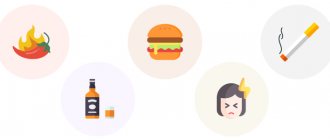
They have a lot in common, in particular, their origin, which is mostly associated with an imbalance between the “aggressive” and “defensive” forces acting in the area of ulcer formation. On the one hand - gastric juice, replete with hydrochloric acid and pepsin, bile acids, alcohol, nicotine, the negative effects of stress, medications, infection with the harmful microbe Heliobacter pylori, unhealthy diet. On the other hand, there is a protective barrier of the stomach and duodenum, resisting destruction of epithelial tissue - mucus, alkaline bicarbonates, hormones, blood supply and restoration of mucosal cells. Seasonal exacerbation of stomach and duodenal ulcers will be discussed in the article. Various diseases proceed in their own way, but both are distinguished by a long-term, chronic, wave-like character. Periods of the so-called possible and “threatened” recurrence of the disease are the most difficult times for ulcer sufferers, since this is not just a recurrence of the disease, but its manifestation in a new quality with the involvement of other organs in the disease, the occurrence of complications of peptic ulcer disease, which cause a poor prognosis of the disease .
Causes of peptic ulcer
The content of the article
Peptic ulcer of the stomach and duodenum is one of the most common gastrointestinal diseases - it affects about 5-10% of adults. Men get sick twice as often, and with duodenal ulcer - four times more often than women.
In the stomach and duodenum, the most important processes of food digestion occur with the participation of hydrochloric acid, pepsin and bile. These are necessary factors, and at the same time aggressive, irritating the gastric mucosa. Fortunately, the body also has protective mechanisms, such as the secretion of mucus and bicarbonate, and the ability to quickly repair the epithelium. If the balance between aggressive and protective factors is disturbed, inflammation, erosion or ulceration develops.
A breakthrough in gastroenterology was the discovery of the bacterium Helicobacter pylori in the stomach. This bacterium is found in 95% of people with duodenal ulcers and in about 75% of people with stomach ulcers. Simply finding the bacteria does not constitute a disease, since it occurs in approximately 50% of healthy people over 50 (and this frequency increases with age).
Helicobacter pylori
Infection occurs through the digestive tract, usually already in childhood. The role of Helicobacter pylori in the formation of ulcers is to increase the secretion of gastrin and hydrochloric acid.
Treatment of exacerbation of gastric and duodenal ulcers
Today there are accepted methods of antiulcer therapy during exacerbation of the disease. These include:
- gastric secretion blockers,
- drugs that activate intracellular protective mechanisms, improve the motor function of the stomach, normalize the nervous system of a sick person,
- course of antibacterial therapy against Helicobacter pylori.
But the selection of medicines is always individual!
A prerequisite for preventive treatment is:
- refusal to take drugs that cause ulcers,
- to give up smoking,
- refusal to drink alcoholic beverages,
- carrying out therapeutic and preventive measures.
Does stress cause ulcers?
The development of gastric and duodenal ulcers is also influenced by a number of other factors, such as:
- genetic predisposition, for example, duodenal ulcers, develops more often in people with blood group 0;
- smoking cigarettes;
- acute or chronic stress;
- numerous injuries, burns;
- stroke;
- taking a lot of painkillers, especially non-steroidal anti-inflammatory drugs, corticosteroids or anti-blood clotting drugs used for cardiovascular diseases.
Rare causes of gastric and duodenal ulcers include: Zollinger-Ellison syndrome, Crohn's disease, hyperparathyroidism, sarcoidosis, HSV - herpes simplex virus and cytomegalovirus.
Stomach ulcer
The symptoms of the disease and its nature are generally similar to the symptoms of gastritis, but its manifestations are more striking and persistent. Standard gastrointestinal pathologies can develop into a gastric ulcer due to increased stress, frequent and unnecessary medications, alcohol and tobacco abuse, or genetic predisposition.
Dental symptoms - swelling of the tongue, plaque on the oral mucosa, enlargement and increased sensitivity of the papillae of the tongue, increased temperature in the mouth, gingivitis and stomatitis
.
Treatment:
similar to the treatment of chronic gastritis or gastroduodenitis.
Ulcers cause abdominal pain, burning and chest pain
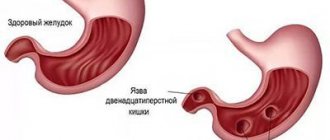
Gastric and duodenal ulcers can present as sudden, severe ulcers, such as in response to stress, or as a chronic, recurring disease. This is especially true for duodenal ulcers.
The main symptom is pressure or pain in the epigastric region, which appears 1-3 hours after eating.
For duodenal ulcers, pain during fasting or night pain is more typical, but an accurate diagnosis cannot be made on this basis. A special examination is required - gastroscopy.
Gastroscopy
Clinical aspects of pyloric helicobacteriosis
| Figure 1. Prepyloric ulcer secondary to atrophic gastritis associated with Hp |
In 1983, B. Marshall and D. Warren described a spiral-shaped bacterium isolated from a biopsy specimen of a patient with antral gastritis, which was named Helicobacter pylori (Hp). Currently, 9 types of HP have been described and it has been established that these are gram-negative, non-spore-forming microorganisms that produce some enzymes (for example, urease) and toxins and have a destructive effect on the tissues of the stomach and duodenum, due to which they are able to overcome the protective barriers in the stomach cavity and colonize the mucous membrane. In addition to local alkalization, a local decrease in the viscosity of gastric mucus occurs around bacterial cells; as a result of the destruction of mucin by mucinase, epithelial cells are injured, causing their dystrophy and reducing functional activity, opening the way for Helicobacter to penetrate deep into the mucous membrane.
In addition, the secretion of gastrin increases and the production of somatostatin is suppressed, the secretion of hydrochloric acid increases, which increases the aggressiveness of gastric juice in the initial stage of helicobacteriosis and leads to active antral gastritis. An inflammatory infiltration forms in the submucosal layer. In addition, a bacterial cell is, in fact, a complex of antigens capable of inducing an immune response, i.e., the body’s production of antibodies.
| Figure 2. Prepyloric erosions |
An important role in the development of chronic gastritis is played by inflammatory mediators, which are either produced by Hp itself, or they are released from destroyed cells of the inflammatory focus. During the formation of antibodies and during phagocytosis, cytotoxins are released, which mutually stimulate the participants in the inflammatory reaction. For example, mast cells release histamine, which increases vascular permeability and facilitates the migration of new cells that make up the infiltrate from the bloodstream to the site of inflammation.
Anti-Hp antibodies synthesized in the submucosal layer effectively bind to bacterial cells and contribute to their death. Thus, a dynamic balance can be established between the Helicobacter population, on the one hand, and factors of natural resistance to infection, on the other. Typically, the protective factors of the macroorganism are not enough to completely destroy the bacterial population, and gastritis becomes chronic.
| Figure 3. Duodenal bulb ulcer |
HP under unfavorable conditions (activation of immune factors, antibacterial therapy, etc.) can transform into an atypical coccal form, which is characterized by the loss of many surface antigens and is less vulnerable. Under favorable conditions, if the destructive effect on the population disappears, HP again turns into a full-fledged S-shaped form, capable of producing toxins (vacuolating, hemolyzing, etc.), under the influence of which the mucous membrane of the stomach or duodenum can undergo “necrotizing” changes with the formation erosions and ulcers. If the HP strain is not able to synthesize the toxin, then the likelihood of ulceration of the mucous membrane is negligible. In these cases, chronic gastritis will remain active either for life or for decades.
Excess hydrochloric acid, which inevitably occurs in the early stage of gastritis, enters the duodenal bulb and strongly acidifies its contents, resulting in the development of gastric metaplasia of the mucous membrane, i.e., a transition to a structural variant resembling the surface epithelium of the antrum of the stomach. On the altered mucous membrane of the bulb, receptors for Hp adhesins appear, on which it colonizes, causing the development of duodenitis, or more precisely, gastroduodenitis. If the strain can synthesize a toxin, the likelihood of ulceration of the mucous membrane of the bulb during exacerbation of gastroduodenitis becomes extremely high.
So, chronic gastritis (gastroduodenitis) and peptic ulcer disease can be represented as a single pathogenetic disease, where HP plays the leading role.
It is advisable to identify several typical clinical and morphological forms of pyloric helicobacteriosis.
Acute gastritis.
At the onset, this form can manifest itself as pain, nausea, vomiting (sometimes mixed with blood), and diarrhea. Gradually, the symptoms of the disease stop and gastritis, as a rule, becomes chronic. Adequate antimicrobial therapy can ensure recovery.
Latent gastritis.
Practically healthy people who do not have complaints related to gastrointestinal diseases. Hp infection can occur as a “carrier” for many years, however, histological examination of gastrobiopsy always reveals changes characteristic of hCG associated with Hp.
Chronic active gastritis.
There are antral (early) and diffuse (late) stages. The main diagnostic criteria for these stages (forms) are given in the table.
Table The main criteria for antral and diffuse forms of CG associated with HP
| Criteria | Forms of hCG | |
| antral - early stage | diffuse (pangastritis) - late stage | |
| Age | Most often young | Most often elderly |
| Subjective manifestations during exacerbation | Often ulcer-like symptoms: periodic pain, including hunger pain, heartburn, sometimes sour belching, constipation | General weakness, feeling of heaviness, dull pain in the epigastric region, unpleasant taste in the mouth, decreased appetite, nausea, belching of air, unstable stool |
| Abdominal palpation results | Local soreness | Diffuse pain (resistance in the pyloroduodenal zone in the epigastrium) |
| Endoscopic results | Against the background of hyperemia and edema of the antrum, submucosal hemorrhages and erosions (flat, raised), hyperplasia of the folds, antral stasis, pyloric spasm are often visible | Pallor, smoothness, thinning, sometimes spotty hyperemia, erosion, transillumination of blood vessels, increased vulnerability of the body and gastric antrum. Hypotension, hypokinesia, bile reflux |
| Results of histological examination of the biopsy specimen | Active antral gastritis, many HP on the surface and in the depths of the pits | Atrophy of the glandular epithelium, intestinal metaplasia, a small amount of HP, minimal activity and severity of inflammation |
Chronic active gastroduodenitis,
most often antropylorobulbit. A form of chronic Helicobacter inflammation involving the duodenum, mainly its proximal part (up to the papilla of Vater). Clinically, it resembles chronic active antral gastritis, and upon endoscopic examination, changes are detected not only in the stomach, but also in the duodenum.
Peptic ulcer
(PU) with the localization of a recurrent ulcer or a long-term non-scarring ulcer in different parts of the stomach and (or) duodenum most often occurs against the background of chronic active Helicobacter gastroduodenitis. The absence of CO from the antrum of the stomach Hp in the biopsy specimen is grounds to assume other, more rare causes of gastroduodenal ulcerations: drugs, Zollinger-Elisson syndrome, hyperparathyroidism, ulcerated cancer, as well as secondary ulcers that occur against the background of certain diseases and external influences.
Infection is a risk factor for gastric carcinoma and lymphoma. In gastric carcinoma and lymphoma, infection of the mucous membrane reaches almost 100%. In recent years, many studies have been carried out aimed at elucidating the role of HP in the occurrence of these diseases. For example, most patients experience regression of gastric lymphoma after drug suppression of CO HP infection. Based on a thorough review of the literature, the WHO team concluded that Hp infection is a risk factor for gastric cancer. However, the possibility of preventing the development of gastric carcinomas and lymphomas by early destruction of the infection is limited due to the lack of ideal therapy and the wide variety of Hp strains.
- DIAGNOSTICS of HP infection
There are histological, cytological and urease tests.
The histological research method has become widespread, as it allows one to detect HP in biopsy specimens and at the same time study the morphological changes that occur in the mucous membrane. The simplest and most accessible method is Giemsa staining of histological preparations without differentiation. HP turns dark blue; bacteria are clearly visible both on the surface of the epithelium and in the depths of the pits. To assess the condition of the mucous membrane and detect HP, 2-3 biopsies (from the antrum and body of the stomach) are sufficient. It is necessary to examine targeted biopsy specimens with pronounced hyperemia of the mucous membrane, but not from the bottom of erosions and ulcers. The frequency of detection of HP using the histological method correlates with other methods and reaches at least 80%.
Recently, new methods have been developed, among which the most sensitive is immunocytochemical using monoclonal antibodies.
Scheme 1. Seven days
| 1. pylorid (ranitidine bismuth citrate) 400 mg x 2 times a day 2. clarithromycin (clacid and other synonyms) 250 mg x 2 times a day 3. metronidazole (Trichopol and other synonyms) 500 mg x 2 times a day day |
The results obtained by detecting HP by DNA hybridization in conventional paraffin media are very encouraging. The technique is not only sensitive, but also highly specific, with its help it is possible to identify different strains of Hp and understand the nature of re-infection after successful treatment.
For cytological examination, fingerprint smears (1-2 or more) obtained from biopsy specimens of the gastric antrum are used. The biopsy is taken specifically from areas with the most pronounced visual deviations from the norm (hyperemia, edema), but not from the bottom of ulcers and erosions.
When HP is detected in fingerprint smears, cellular infiltration is usually also detected, characterized by the presence of lymphocytes, plasma cells, neutrophils and eosinophils. By the predominance of certain cellular elements, one can indirectly judge the activity and severity of inflammation. In addition, cytological examination allows us to detect the presence of proliferative processes, metaplasia (intestinal in the stomach and gastric in the duodenum), dysplasia and the degree of their severity, and malignant neoplasm cells in the cells of the mucus. However, the cytological method does not provide information about the structure of the test mucus.
Scheme 2. Ten-day
| 1. ranitidine (Zantac and other synonyms) 150 mg x 2 times a day 2. potassium salt of dibasic bismuth citrate* (108 mg in a tablet) x 5 times a day with food 3. tetracycline hydrochloride* (250 mg in a tablet .) x 5 times a day with food 4. metronidazole* (200 mg in a tablet) x 5 times a day with food * are part of a drug registered in Russia under the name “gastrostat”. |
In terms of the speed of detection of persistent Hp in CO, the cytological method is not inferior to the express method based on the urease activity of Hp, called the campi test. The test consists of a carrier gel as a pH indicator. The indicator changes color from yellow to crimson when, under the action of urease, urea is hydrolyzed to form ammonia, which shifts the pH of the medium to the alkaline side. A change in the color of the medium occurs only if the biopsy sample contains urease, “accumulated” Hp. The time of appearance of crimson coloring indirectly indicates the number of viable bacteria. The appearance of crimson staining during the first hour corresponds to a significant infection of CO Hp (+++), during the next two hours - moderate (++), by the end of the day - insignificant (+), if staining occurs at a later date, the result is considered negative .
False-negative results can occur in patients with weak CO contamination. False-positive results occur when endoscopes and biopsy forceps are handled incorrectly.
Scheme 3. Seven days
| 1. omeprazole (Losec) 20 mg x 2 times a day (at 8 a.m. and 8 p.m.) 2. clarithromycin (Klacid and other synonyms) 250 mg x 2 times, or amoxicillin 1000 mg x 2 times a day, or tetracycline 500 mg x 3 times a day 3. metronidazole (Trichopol and other synonyms) 500 mg x 2 times a day with food. The eradication rate reaches 95%. |
Among additional methods for diagnosing HP, microbiological, immunological and radionuclide methods should be noted. For example, 12-C-urease breath test. In most countries of the world it is considered as the main test for detecting HP infection. The method is non-invasive, absolutely safe and allows you to determine the degree of colonization of CO Hp, and is the optimal way to monitor the effectiveness of eradication therapy.
In a regular laboratory, these methods are not readily available and are rarely used in practice.
- THERAPY
The absolute indications for eradication therapy are the following: peptic ulcer of the stomach and duodenum (exacerbation and remission), ulcerative bleeding, gastric lymphoma, gastritis with pronounced endoscopic and histological changes, conditions after surgical treatment of early gastric cancer.
Scheme 4. Ten-day
| 1. ranitidine (Zantac and other synthetics) 300 mg x 2 times a day (at 8 a.m. and 8 p.m.) 2. colloidal bismuth subcitrate* 108 mg x 5 times a day after meals 3. metronidazole* 200 mg x 5 once a day after meals 4. tetracycline hydrochloride* 250 mg x 5 times a day after meals The eradication rate reaches 85-90% * included in a combination drug registered in Russia under the name “gastrostat”. |
Relative indications include: functional dyspepsia after a complete examination, long-term treatment with proton pump inhibitors, esophageal reflux disease, condition after surgical treatment of peptic ulcer (vagotomy, drainage operations, etc.), the wishes of the patient for asymptomatic (latent) infection Hp.
Treatment of diseases associated with pyloric helicobacteriosis should be comprehensive, but with the obligatory inclusion of antibacterial agents - etiotropic therapy. Indications for prescribing complex therapy are the severity of clinical and morphological manifestations of various forms of gastritis, gastroduodenitis and ulcer, and etiotropic therapy is confirmation of infection of the coolant with the help of appropriate diagnostic tests.
- TREATMENT OBJECTIVES: HP eradication, healing of erosions and ulcers, prevention of exacerbations and complications
For gastritis and gastroduodenitis associated with HP, there are several drug treatment regimens (schemes 1 and 2).
In addition, symptomatic treatment is carried out using antacids and prokinetics.
The duration of inpatient intensive treatment is 10 days, but taking into account the etiology and severity of clinical and morphological manifestations of the disease, they can be changed.
Scheme 5. Fourteen days
| 1. omeprazole (Losec) 20 mg x 2 times a day (at 8 a.m. and 8 p.m.) or ranitidine 150 mg x 2 times a day 2. colloidal bismuth subcitrate (Ventrisol, de-Nol) 120 mg x 3 times for 30 minutes before meals and the 4th time 2 hours after meals before bed) 3. metronidazole 500 mg x 3 times a day after meals or tinidazole 500 mg x 2 times a day after meals 4. tetracycline or amoxicillin (flemoxin solutab, etc. syn.) 500 mg x 4 times a day after meals. The eradication rate reaches 95%. |
Requirements for treatment results: absence of clinical symptoms, endoscopic and histological signs of inflammatory activity and infectious agent (complete remission) or cessation of pain and dyspeptic disorders, reduction of signs of process activity without eradication of HP. Patients with active gastritis (gastroduodenitis) associated with HP and autoimmune gastritis are subject to dispensary observation.
Drug treatment of gastroduodenal ulcers associated with HP involves the use of one of the schemes (see schemes 3, 4, 5).
After the end of combination therapy, continue treatment for another 6 weeks using one of the following drugs:
1.
ranitidine (Zantac and other synonyms) - 300 mg at 19-20 hours 2.
famotidine
(gastrosidine, quamatel, ulfamide) - 40 mg at 19-20 hours.
3.
Sucrat gel - 1.0 x 2 times a day 30 minutes before meals.
4.
Maalox - 15 ml x 3 times a day 2 hours after meals.
The duration of inpatient treatment for stomach ulcers and gastrojejunal ulcers is 30 days, for duodenal ulcers - 10 days. The general course of drug therapy, including outpatient treatment, averages 8-12 weeks.
Requirements for treatment results: relief of clinical and endoscopic manifestations of diseases (complete remission) with two negative tests for Hp (histological and urease), which are carried out no earlier than the 4th week after discontinuation of drug treatment.
In case of partial remission, which is characterized by the presence of an unhealed ulcer, it is necessary to analyze the patient’s discipline in the treatment regimen and continue drug therapy with appropriate adjustments.
To prevent exacerbations of gastric ulcer and especially duodenal ulcer, and therefore their complications, two types of therapy are recommended: continuous and “on demand”.
Continuous (months or even years) maintenance therapy with an antisecretory drug in half the dose, for example, taken daily at 20:00 150 mg of ranitidine (Zantac and other syn.) or 20 mg of famotidine (gastrosidine, quamatel, ulfamide) is indicated for:
— ineffectiveness of the eradication therapy; - complicated course of peptic ulcer (history of peptic ulcer bleeding or perforation); — concomitant diseases requiring the use of non-steroidal anti-inflammatory drugs; — erosive and ulcerative reflux esophagitis accompanying ulcerative ulcer; - patients over 60 years of age with annually recurrent peptic ulcer disease, despite adequate course therapy.
When remission of a peptic ulcer occurs, there is no active gastroduodenitis and infection of the gastric mucosa, Hp therapy is stopped, and when symptoms of an exacerbation of the disease appear, it is carried out “on demand”, i.e. from the first days of an exacerbation:
— stricter adherence to the dietary regime; - stopping smoking (for smokers), taking “ulcerogenic” medications;
If after a 14-day course of antiulcer therapy the symptoms of exacerbation completely disappear, then therapy should be stopped, but if the symptoms do not disappear or recur, then esophagogastroduodenoscopy and other studies must be repeated.
- PREVENTION
Prevention of pyloric helicobacteriosis is not fundamentally different from preventive measures carried out for other infections: timely diagnosis, sanitary and hygienic regime, sanitation of the mucous membrane of the stomach and duodenum, anti-epidemic measures at the source of infection. The development of a set of specific recommendations specifically for this infection is a matter of the near future. It is clear, however, that first of all you should pay attention to those stages where the risk of infection is highest, gastroenterological clinics and hospital departments.
The priority tasks include conducting screening epidemiological studies to establish the level of Hp infection in different age and social groups of the population, the frequency of infection becoming manifest forms and the role of Helicobacteriosis in gastroduodenal pathology.
Adequate treatment of patients with gastritis, duodenitis and peptic ulcers associated with HP is of utmost importance in the prevention of helicobacteriosis.
Diet for peptic ulcers
Foods that increase stomach and duodenal problems include raw fruits, spicy, sour, fried and baked foods. The pain is relieved by drinking milk or taking antacids.
Sometimes the pain can spread to the back, for example with ulcers that penetrate the pancreas. Patients may experience flatulence or heartburn. There is also a seasonality of the disease with exacerbations in spring and autumn. Sometimes an ulcer does not produce any symptoms, and in extreme cases, the first symptom is gastrointestinal bleeding.
Prolonged peptic ulceration, alternating with active and healing ulcers, can cause pyloric stenosis, which significantly impedes the movement of gastric contents. Patients often experience profuse vomiting, gradual loss of body weight, cachexia, and anemia. Complications also include gastrointestinal bleeding and ulcer perforation.
Treatment
Treatment depends on whether helicobacter is detected in the patient’s body or not. In the first case, the doctor prescribes two types of antibiotics, because one does not kill her, as well as drugs that create unfavorable conditions for the life of bacteria. Sometimes, after destroying the bacteria, the ulcer itself does not heal, then the patient is prescribed drugs that reduce secretion and improve tissue trophism. If helicobacter is not detected, antibiotics are not prescribed.
The course of treatment usually lasts 14 days, in certain cases it takes longer. Thus, a callous ulcer (large, advanced, with a diameter of more than 5 cm) can heal in 2-3 months. Usually, the defect grows to such a size in older people who have been taking non-steroidal drugs for years and have not checked their stomach. First of all, to heal it, the doctor stops the medications that cause peptic ulcers.
Operation
Treatment of peptic ulcers rarely requires surgery. It is only necessary in case of complications. For example, a perforated (perforated) ulcer can only be cured through surgery. The operation is also performed for massive bleeding, when it cannot be stopped conservatively, and for spinosis (narrowing of the duodenum).
Nutrition
To heal the defect, in addition to drug treatment, you must follow a diet. It consists of following a diet: a person should eat small portions 4-5 times a day, excluding spicy, salty, fried, smoked foods. All food must be boiled or steamed. When the ulcer heals, you no longer need to follow a diet, but you should still not abuse spicy, fried, smoked and salty foods. It is also important to eat regularly, without skipping meals, to prevent exacerbation. Alcohol is contraindicated for any gastrointestinal disease. Products that are best avoided: baked goods, brown bread, tomatoes, coffee, strong tea, lard, lamb fat, margarine, chocolate. The diet can include: dried wheat or yesterday's bread, crackers, savory cookies, milk soups, beef, chicken, pike perch, pike, perch, water porridge with the addition of milk (semolina, buckwheat, oatmeal, pearl barley, rice).
Helicobacter Pylori Study
Diagnosis of gastric and duodenal ulcers is usually based on gastrofibroscopy, during which Helicobacter pylori can be tested and samples taken for histopathological examination. The test is positive if the color of the reagent changes after contact with a segment of the gastric mucosa.
Histopathological examination, in turn, is important for differentiating peptic ulcers from gastric cancer, which can also take the form of an ulcer.
X-ray examination is practically not carried out when diagnosing an ulcer, since it is less accurate and does not provide the above diagnostic capabilities, and also exposes the patient to radiation.
You can replace gastroscopy with a breath test for Helicobacter pylori. This is a modern study that takes literally a couple of minutes. The advantages of the technique are non-invasiveness, absence of contraindications and ease of implementation.