Gastritis is one of the most common diseases among all pathologies of the digestive system. This disease is observed in 80-90% of the population. Its main danger is the transition to peptic ulcer disease and the possibility of malignancy.
Gastritis is a specific disease of inflammatory-dystrophic origin of the stomach, in which structural changes occur in its mucous membrane, leading to dystrophy, atrophy or dysregeneration. In the process of these changes, the secretion functions of digestive enzymes (hydrochloric acid and pepsin), synthesis and motility processes of gastrointestinal hormones are disrupted.
Epidemiology
According to statistics, gastritis is registered in 80-90% of adults. Helicobacter pylori associated is recognized as the most common; it accounts for 90% of all diagnoses of chronic hepatitis. The most dangerous form with a high percentage of malignancy is atrophic, occurring in 5% of cases in people under 30 years of age, in 35% in patients 30-50 years of age, in 70% in patients over 50 years of age.
In children, the disease most often develops during puberty and at the age of 4-7 years, when the child is most susceptible to infectious and viral diseases.
Why does hyperacid gastritis develop?
In the oral cavity, carbohydrates, under the influence of enzymes, begin to break down into simple compounds, and proteins and fats are broken down in the stomach under the influence of hydrochloric acid, which promotes the breakdown of pepsinogen into pepsin and will cause denaturation and swelling of proteins.
Hydrochloric acid not only promotes the breakdown of nutrients, it also stimulates the secretory and mechanical functions of the stomach, and destroys bacteria introduced with food. To protect the gastric mucosa, cells produce mucus (mucin), which covers the tissue with a layer of 1.3–1.5 mm. This “film” is an insurmountable barrier to the reverse diffusion of hydrogen ions from the stomach, adsorbs and inhibits enzymes, and neutralizes hydrochloric acid.
Mucin protects the organ from autolysis (self-digestion). However, this barrier can be destroyed due to prolonged exposure to bile acids, salicylates (found in some medications), alcohol, butyric or propionic acid, as a result of increased production of hydrochloric acid.
The acidity of gastric juice is affected by the number of cells secreting hydrochloric acid, as well as the rate of acid production and the degree of its neutralization. At low pH, cell damage occurs and an inflammatory process develops.
Etiology
The development of gastritis is caused by the influence of many factors on gastric tissue. Among the reasons, exogenous and endogenous factors are distinguished.
Exogenous factors include:
- eating disorders;
- bacterial colonization by Helicobacter pylori, less commonly by other bacteria or fungi;
- radiation exposure, chemical damage;
- long-term use of medications that irritate the mucous membrane (the most aggressive are glucocorticosteroids, anti-inflammatory drugs, acetylsalicylic acid, etc.);
- parasitic infestations;
- bad habits (especially alcohol and smoking);
- chronic stress.
Among the endogenous factors are:
- genetic predisposition;
- autoimmune processes;
- duodenogastric reflux;
- metabolic disorders;
- endogenous intoxications;
- endocrine dysfunctions;
- hypoxemia;
- avitaminosis;
- chronic infectious diseases;
Also, the development of gastritis is promoted by various reflex effects from other affected organs.
Causes
To date, it has been proven that the leading cause of the development of gastritis with high acidity is infection of the mucous membrane with Helicobacter. There is a direct connection between the number of bacteria and the severity of gastritis. Helicobacter pylori infection affects only the epithelial cells of the stomach - this is confirmed by many studies in which the bacterium was found in the duodenum only in areas of the epithelium that had metaplasticized into the gastric epithelium.
These bacteria have a special structure and a number of protective mechanisms that allow them to survive and reproduce in the aggressive environment of the stomach. They are able to create an alkaline cocoon around themselves and penetrate deep into the mucosa, destroying stomach cells and protective barriers that prevent gastric juice from affecting its own mucosa. Under the influence of ammonia, which is produced by microorganisms, the secretion of gastrin increases, and the level of somatostatin decreases - all this leads to an increase in the secretion of hydrochloric acid and an increase in the acidity of gastric juice. Also, multiplying bacteria provoke the release of pro-inflammatory prostaglandins and the inflammatory process in the mucous membrane.
Errors in nutrition provoke the progression of Helicobacter pylori infection: eating on the go, in a hurry, dry food, frequent consumption of too cold or hot foods, fried and extracted. Often this type of gastritis occurs in people who abuse alcohol, smoking, and strong coffee. The course of the infection also worsens under the influence of radiation, taking certain medications, and allergies to certain foods. Exacerbations of gastritis often occur against the background of severe stress.
There are a number of internal factors that contribute to the development of hyperacid gastritis: severe chronic infections, metabolic disorders (diabetes mellitus, thyroid diseases, gout and others), oxygen starvation. Duodeno-gastric reflux (reflux of the contents of the small intestine into the stomach through the pylorus) has an important pathogenetic significance - the entry into the stomach of alkaline intestinal contents and especially bile causes additional damage to the gastric mucosa, reducing its resistance to the effects of hydrochloric acid. Often inflammation in the stomach develops against the background of other serious diseases due to reflex effects.
Pathogenesis
The mechanism of pathogenesis is based on characteristic inflammation of the mucous membrane, which leads to its structural restructuring. If predisposing factors and the active influence of causes are present, the process of inflammation begins, which is characterized by a long course.
Chronitization is based on round cell inflammatory infiltration by neutrophils and other cells of the autoimmune system of the mucosa. Under the influence of the inflammatory reaction, the links in the restructuring of the shell structure and the development of active dysregenerative processes in it are triggered with a further transition to dystrophy and atrophy. The result of these processes is a quantitative change in hydrochloric acid.
The leading role is occupied by associated Helicobacter pylori, the second most common is drug-induced gastritis, and then atrophic.
Symptoms of gastritis
All types of inflammation of the gastric mucosa are characterized by universal syndromes that are present in any form of the disease:
Pain syndrome in which there is a feeling of fullness directly in the stomach, colic in the intestines. Unpleasant symptoms are associated with food intake - they worsen and disappear before or immediately after food, depending on the form and location of the inflammation.
Dyspeptic syndrome, expressed in nausea, vomiting, diarrhea or constipation, flatulence. With hyperacid gastritis, patients are bothered by heartburn and sour belching. With the anacid form of inflammation, rotten belching appears, an unpleasant taste in the mouth, and the stool becomes foul-smelling.
In the chronic course of the disease, the manifestation of a neurological syndrome is characteristic, which is caused by an acute lack of nutrients. The patient is worried about headaches and dizziness, apathy and weakness, irritability.
Also, in the chronic form of the disease, signs of dysfunction of the cardiovascular system appear in the form of arrhythmia, unstable blood pressure, and chest pain. The reason why gastritis affects not only the gastrointestinal tract, but also other organ systems is an imbalance of water and electrolytes and a lack of vital substances.
Infectious inflammation of the gastric mucosa in adults and children causes fever, which is combined with dyspeptic and pain syndrome. The atrophic form of chronic inflammation provokes the emergence of a symptom complex combining dyspeptic and neurological disorders.
Symptoms of the disease
Clinical symptoms can be divided into pain, dyspeptic disorders, and general symptoms of malaise.
Pain syndrome
Quite often it is the leading link in the clinical picture of the disease, since it is with this that patients seek help.
As a rule, pain is localized in the epigastrium, in other parts of the abdomen much less often. With gastritis with high acidity, a typical pain syndrome develops 1-2 hours after eating, the pain is acute and cutting in nature.
Dyspeptic manifestations
This syndrome is characterized by a violation of the digestion process, which is manifested by the following symptoms:
- decreased appetite;
- discomfort after eating;
- heartburn (may worsen when changing position);
- nausea;
- belching, flatulence;
- gagging - sometimes vomiting;
- sour or metallic taste.
With gastritis with high acidity, the symptoms are most often mildly expressed and become more active in combination with provoking factors (significant pauses between meals, severe stress, overeating, violation of the temperature regime of food, etc.).
General symptoms of illness
As a rule, with uncomplicated forms of pathology, the general condition changes to an insignificant extent. As the inflammatory process increases, changes can be quite pronounced. The most commonly observed symptoms are:
- severe general weakness;
- hypotension, dizziness;
- irritability;
- increased sweating;
- intolerance to certain foods;
- reduction in body weight by more than 5% of total weight within six months;
- hypovitaminosis.
Patients with Helicobacter pylori with hyperacidity may develop ulcer-like symptoms, which indicate a probable pre-ulcerative condition.
In general, the clinical picture is determined by the specificity of gastric secretion disorders and the degree of motor-evacuation dysfunction. The initial period is characterized by symptom-free symptoms, then, as the inflammatory process progresses, a pain syndrome develops with the addition of dyspepsia.
What is a disease
Stomach pain due to high acidity is common.
Hyperacid gastritis, translated from Latin, roughly translates as follows: replenishment of the stomach, accompanied by increased acidity. If you remember school, biology, or rather, lectures on anatomy, then you know that hydrochloric acid and other digestive juices produced in the stomach are involved in the process of digesting food. But if acid is produced in excess of normal, it begins to destroy the walls of the stomach.
This is why high acidity causes harm to humans. The most “innocent” disease that can result from excess acid is gastritis, but the consequences will be much more serious if a stomach ulcer appears. If a patient diagnosed with gastritis has not completed the full course of treatment, then the disease is complicated by a stomach ulcer, which is not so easy to get rid of, and in advanced cases, surgical intervention, that is, surgery, is simply necessary.
Classification, stages of the disease
In clinical practice in Russia, the working classification based on the developments of S. M. Ryss and the Sydney classification is most often used.
Working classification
According to etiology and pathogenesis:
- Type A
: characterized by autoimmune fundic atrophic processes, including those associated with Addison-Bearman anemia;
- Type B
: specific bacterial antral non-atrophic process associated with Hp;
- Type C
: a chemical form associated with reflux of lysolecithin, duodenogastric reflux, and also due to the use of medications;
- Type AB
: characteristic combined atrophic pangastritis, characterized by the involvement of all parts of the stomach in the process.
In addition, there are alcoholic, drug, radiation, lymphocytic, granulomatous eosinophilic and other forms of the disease.
According to topographer-morphological features
By localization:
- fundal;
- astral;
- pangastritis.
According to morphological criteria:
- surface form;
- interstitial;
- atrophic (mild, moderate or severe);
- with complete or partial intestinal metaplasia (small or large intestine).
According to specific morphological characteristics
According to the severity of inflammation:
- minimum;
- insignificant level;
- moderate;
- expressed.
By degree of activity:
- not active;
- mild;
- average;
- heavy.
According to the severity of coolant contamination:
- not expressed;
- lungs;
- average;
- tall.
According to the features of the clinic:
- with a predominance of pain (type B);
- with a predominance of dyspeptic disorders (type A);
- latent (asymptomatic).
According to functional criteria:
- with preserved secretion;
- with increased;
- with secretory insufficiency.
According to endoscopic criteria:
- erythematous (exudative);
- with flat (sharp) erosions;
- rising erosions (chronic);
- hemorrhagic;
- complicated by reflux gastritis;
- hyperplastic.
Separately, gastritis of unknown origin is distinguished, as well as of mixed origin.
The course of chronic hepatitis is characterized by two stages: relapse (exacerbation) and remission, gradually replacing each other.
specialist
Our doctors will answer any questions you may have
Tumasova Anna Valerievna Gastroenterologist
Stages of the disease
The disease occurs in 4 main stages:
- Hyperemic.
At the initial stage, the mucous membrane acquires a reddish color, and slight swelling appears.
- Hypertrophic.
At this stage, thickening of the mucosa occurs with a parallel decrease in hydrochloric acid. Changes are likely both in tissues and at the cellular level (dysplasia), as well as the accumulation of leukocytes (metaplasia).
- Atrophic.
As a result of a long-term ongoing process of inflammation, the mucous membrane becomes thinner, regenerative capacity decreases, and epithelial cells die off and are subsequently replaced by scar tissue.
- Erosive and/or ulcerative.
Due to thinning of the mucous membrane, focal lesions of varying depths form on the inner surface of the stomach.
With each subsequent exacerbation, these lesions deepen and grow, and the symptoms increase accordingly.
General information
Gastritis with high acidity is an inflammatory process that occurs in the stomach under the influence of H. pylori infection. Provoking factors that cause acute hyperacid gastritis or exacerbation of chronic gastritis can be errors in nutrition, stress, or taking certain medications. Gastritis with high acidity most often occurs in young people, often in children. This is due to changes in nutritional culture - more and more people eat on the go, fast food, irregularly, which as a result leads to severe stomach damage.
Long-term chronic gastritis with increased acidity can lead to serious complications, in particular gastric or duodenal ulcers. A big problem that provokes worsening of the condition with gastritis is self-medication with the uncontrolled use of drugs and folk remedies that have antacid properties. Taking these medications without the prescription and supervision of a gastroenterologist can cause a serious disorder of gastric secretion, which will ultimately provoke atrophy of the gastric glands and mucous membrane and lead to irreversible consequences.
Chronic gastritis is considered the most common disease in modern gastroenterology - it affects at least 50% of the population. It is known that histological signs of mucosal inflammation are found in half of the subjects who have never complained of dyspeptic disorders, and in those who complained of dyspepsia, such changes are found in 45% of patients.
Gastritis with high acidity
Possible complications
If the doctor’s recommendations are not followed or therapy is inadequate, gastritis can be complicated by the following pathological conditions:
- digestive disorders in the form of malabsorption and dyspepsia;
- vitamin B deficiency;
- peptic ulcer: most often develops with the erosive form of gastritis;
- gastric bleeding: occurs with ulcers and erosions. Clinical signs will include pallor, weakness, cold and sticky sweat, shortness of breath, tachycardia, the presence of blood in the vomit, black stools. This condition requires immediate hospitalization;
- atrophic gastritis: the glands of the mucous membrane almost completely stop producing secretions, the process of replacement with scar tissue begins, it refers to a prenatal condition, the likelihood of malignancy is extremely high;
- iron deficiency anemia (develops with low production of Castle factor);
- stomach cancer.
During an exacerbation, severe complications can develop within several days, and sometimes even one day.
What can a patient do on his own?
A drug to reduce stomach acidity
Drug treatment is prescribed only by a doctor. But the patient can improve his condition on his own if he adheres to an appropriate diet. The diet for gastritis is very strict, as it is forbidden to include fatty, smoked and fried foods, fresh white bread, sour vegetables and fruits in your menu. In addition to the prohibited foods listed above, the diet suggests that the patient should drink little by little, but often, every 3-4 hours.
Treatment
Basic treatment is based on the complete or maximum possible exclusion of “aggression” factors that negatively affect the gastric mucosa. Therapy during an exacerbation period begins with following a gentle diet according to Pevzner (table No. 1 and No. 2).
Diet for gastritis
In case of relapse of the disease, a gentle diet is used, and the preparation option is pureed. The basic principles of therapeutic nutrition include:
- mechanical sparing:
is carried out thanks to the choice of products according to the degree of coarse fiber content, digestion time in the stomach, as well as through the process of thorough culinary processing (steam cooking, stewing, giving food the consistency of puree);
- thermal sparing:
is ensured by the exclusion of excessively hot and cold foods that can injure the mucous membrane. The most optimal temperature for hot dishes should be in the range of +30-40 degrees;
- chemical sparing:
consists of increasing vegetable fats and animal proteins against the background of the physiological norm of vitamins, microelements, and all carbohydrates. This is due to the ability of fats to slow down gastric secretion, and on the part of proteins - inactivation of hydrochloric acid;
- limiting the amount of food taken at one time (the “often, but little” principle):
Meals should be 5-6 times a day, in small portions. The best option would be to match food intake with the process of activating the production of hydrochloric acid.
In addition, foods that have a medium and low level of stimulation of acid production are excluded from the diet: berries, fruits, meat, soft-boiled eggs, white bread crackers, cereals, sweet fruits and vegetables.
During a gentle diet, the range includes:
- pureed vegetable soups (excluding cabbage soup and borscht), milk and cereal or noodle soups;
- unleavened cottage cheese, low-fat and non-spicy varieties of cheese;
- boiled pureed vegetables: Brussels sprouts and cauliflower (white cabbage is prohibited), zucchini, carrots, beets, tomatoes;
- compotes with pureed dried fruits;
- dried wheat bread.
All dishes are cooked strictly by steaming, boiling until soft, grinding and serving warm.
During the period of remission, it is advisable to adhere to the principles of a healthy diet. It is important to exclude spices, spicy foods, smoked meats and marinades, and strong meat broths. You should limit pastry, tea, drinks with a high carbon dioxide content, and chewing gum. It is strictly forbidden to drink alcoholic beverages, coffee, and smoking is also prohibited.
Drug treatment
The use of medications is aimed at reducing the active production of hydrochloric acid, regenerating the mucosa and increasing the protective functions of the mucous-bicarbonate barrier. The main groups of drugs used include:
- proton pump inhibitors: the principle of action is based on reducing the formation of hydrochloric acid, they are not addictive (omeprazole, pantoprazole, esomeprazole, etc.);
- H2-histamine receptor blockers: drugs block the effect of histamine on the parietal and parietal cells, resulting in a decrease in the synthesis of pepsin and hydrochloric acid. There is also an increase in the formation of prostaglandins, which increases the protective properties of the mucosa and stimulates regenerative processes. With prolonged use, addiction occurs;
- cytoprotectors: bismuth preparations, sucralfate, misoprostol are prescribed;
- antibacterial therapy: used in a combination of 2-3 drugs, the goal is eradication of Helicobacter pylori (penicillins, niroimidazole derivatives, macrolides);
- prokinetics: prescribed to reduce the frequency of reflexes (itopride hydrochloride, cerucal, domperidone);
- antispasmodics: the mechanism of action is to relieve spasticity (mebeverine, no-spa, hyoscine butyl bromide);
- replacement therapy: prescribed for the atrophic form and achlorhydria (enzymes and gastric juice drugs).
Other groups of drugs are prescribed for the treatment of concomitant pathologies and complications.
Gastritis and its treatment
Stress is not the only cause of increased acidity. Scientists in the last century identified the bacterium Helicobacter pylori, which causes the disease. After which, in addition to drugs that reduce acidity, patients were prescribed antibiotics, after which the symptoms of the disease began to subside.
When sick, patients must be prescribed a diet.
But it also happens that after some time the disease appears again, and with the same force. In this case, gastritis is considered chronic, which means that a person must adhere to a diet for life, and during an exacerbation of the disease, treatment is carried out according to the standard regimen. But, despite this, gastroenterologists do not recommend self-medication, even if you have studied your illness “in and out.” Chronic gastritis can lead to
Prognosis and prevention
The prognosis is usually favorable. Complications, especially bleeding and malignancy, pose a danger.
To prevent the occurrence and progression of gastritis, it is necessary:
- maintain an optimal diet;
- to refuse from bad habits;
- carry out regular sanitation of the oral cavity;
- promptly identify and treat other pathologies of the digestive system.
Patients with a severe course and atrophic form should be registered at the dispensary with annual endoscopic monitoring, and also undergo anti-relapse treatment in the fall and spring.
Diagnostics
Correct diagnosis of gastritis with increased acidity of gastric juice requires a series of clinical, functional and instrumental examinations. Changes in clinical tests are nonspecific for gastritis - an increase in inflammatory elements may be noted. With concomitant damage to other organs, corresponding changes appear in the biochemical blood test. If there are erosions in the stomach and bleeding from them, occult blood is determined by a special analysis in the stool. Research is required to search for H. pylori: urease breath test, ELISA and PCR analysis to detect antibodies and DNA of the microorganism, respectively. Also, a large number of bacteria can be detected during endoscopic biopsy of the gastric mucosa and histological examination.
If gastritis is suspected, it is mandatory to perform gastroscopy, or better yet, FEGDS - a special instrument with a video camera is inserted into the stomach, allowing you to examine the esophagus, stomach and duodenum, identify the inflammatory process, erosions and ulcers. During the study, tissue must be taken for biopsy from several places. pH-metry is also carried out - measuring the acidity of gastric juice; if it is less than 1.5 - they speak of hyperacid gastritis. Pieces of tissue taken during a biopsy are examined by histologists - signs of inflammation are determined, and a huge number of Helicobacter bacteria can be detected.
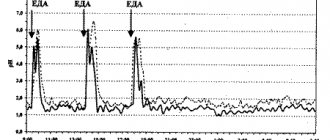
The pressure in the stomach cavity is measured, electrogastroenterography is carried out - they help identify duodenogastric reflux, which also aggravates the course of the disease. As auxiliary diagnostic methods, it is possible to perform ultrasound, CT or MSCT of the abdominal organs, but for gastritis they are not of decisive importance; they only allow to identify concomitant damage to other organs.
Publications in the media
Chronic gastritis is a long-term disease characterized by the development of a number of morphological changes in the gastric mucosa and accompanied by various disorders of its basic functions. Prevalence. 50–80% of the entire adult population, the incidence of chronic gastritis increases with age. Incidence of gastritis and duodenitis: 287.2 per 100,000 population in 2001.
Classification
• By etiological factor • Microbial: Helicobacter pylori, etc. • Non-microbial •• Autoimmune •• Alcoholic •• Post-resection •• Caused by exposure to NSAIDs •• Caused by exposure to chemical agents • Unknown factors, incl. microorganisms.
• By type • Non-atrophic (type B, superficial, diffuse antral, hypersecretory) • Atrophic (type A, diffuse gastric body, associated with B12-deficiency anemia) • Special forms •• Chemical •• Radiation •• Lymphocytic •• Giant hypertrophic ( Ménétrier's disease, adenopapillomatosis) •• Granulomatous •• Eosinophilic •• Other infectious.
• By localization • Antral gastritis • Body gastritis • Pangastritis.
Etiology • Chronic non-atrophic gastritis in 85–90% of cases is caused by Helicobacter pylori • The development of chronic atrophic (autoimmune) gastritis is associated with the genetically determined production of autoantibodies to the lining cells of the gastric mucosa • The most common causes of chemical (reactive) gastritis are bile reflux and long-term use of NSAIDs • The etiology of eosinophilic gastritis is unknown, some patients have a history of bronchial asthma, eczema and other allergic diseases • Granulomatous gastritis is found in 10% of patients with sarcoidosis, 7% of patients with Crohn’s disease, with tuberculosis, mycoses, foreign bodies in the stomach • Etiology of giant hypertrophic gastritis is unknown.
Clinical picture
• Chronic non-atrophic gastritis • The pain syndrome often resembles that of duodenal ulcer (pain in the epigastric region that occurs on an empty stomach, but is usually less intense). The pain can be acute, cramping or aching, not intense; sometimes occur soon after eating • Dyspeptic syndrome - heartburn, sour belching, less commonly nausea, vomiting of gastric contents.
• Atrophic gastritis • Often combined with B12-deficiency anemia, thyroiditis, thyrotoxicosis, primary hypoparathyroidism • Sometimes the disease is latent • The most common manifestations are heaviness in the epigastric region after eating, a feeling of overeating, fullness of the stomach, belching of food and air, unpleasant taste in the mouth , loss of appetite, possible flatulence, unstable stool.
• Chemical (reactive) gastritis • Characterized by a triad of symptoms: pain in the epigastric region, intensifying after eating, vomiting with bile, bringing relief, weight loss.
• Giant hypertrophic gastritis • Pain in the epigastric region of varying intensity, often aching, occurs after eating and is accompanied by a feeling of heaviness in the stomach • Vomiting and diarrhea are possible; appetite is often reduced, sometimes even to the point of anorexia • In most patients, body weight decreases (by 10–20 kg) • In 25–40% of patients, peripheral edema is detected due to significant loss of protein with gastric juice (more than 8 g/day) • Gastric bleeding from erosions • Gastric carcinoma develops in 10% of cases.
Diagnostics
• OAC: B12-deficiency anemia in chronic gastritis type A
• Stool analysis: possible presence of hidden blood, as well as undigested food debris with reduced secretory activity of the stomach.
• X-ray examination does not allow diagnosing the main forms of chronic gastritis; but with its help it is possible to identify ulcers, cancer, polyposis, duodenal gastric reflux, giant hypertrophic gastritis, chronic obstruction of the duodenum • Chronic obstruction of the duodenum - delay of the contrast mass in the intestinal lumen for more than 45 s, expansion of the intestinal lumen, the presence of duodenum gastric reflux •• Giant hypertrophic gastritis (Menetrier's disease) - pronounced thickening of the folds of the mucous membrane in a limited area (with a local variant) or throughout the stomach (with a diffuse variant). The stomach wall in the affected area is elastic, peristalsis is visible.
• FEGDS •• Non-atrophic (superficial) gastritis: the mucous membrane is shiny (sometimes with a coating of fibrin), edematous, hyperemic, submucosal hemorrhages •• Atrophic gastritis: the mucous membrane is thinned, pale gray in color, with translucent blood vessels, the relief is smoothed •• Reflux -gastritis: the pylorus is gaping, the gastric mucosa is hyperemic, edematous; bile is present in the stomach •• Giant hypertrophic gastritis: there is a large amount of mucus in the stomach, the mucous membrane is easily vulnerable, erosions and hemorrhages are often found.
• Study of the secretory function of the stomach •• Chronic non-atrophic gastritis, reflux gastritis: the secretory function is normal or increased •• Chronic atrophic gastritis, giant hypertrophic gastritis: the secretory function of the stomach is reduced.
• Detection of Helicobacter pylori •• Invasive methods: it is necessary to perform FEGDS with a biopsy of the gastric mucosa; at least five biopsies are taken (two each from the antrum and fundus and one from the angle of the stomach). To confirm the success of eradication, the study is carried out no earlier than the 5th week after completion of the course of treatment ••• Bacteriological method ••• Histological method (detection of bacteria during microscopic examination of stained preparations) ••• Biochemical method (urease test) •• Non-invasive tests •• •Immunological methods (detection of antibodies to Helicobacter pylori) •••Breath test ••PCR diagnostics in biopsy samples of the gastric mucosa (invasive method) and in the patient’s feces (non-invasive method).
• Detection of antibodies to parietal cells and intrinsic factor and hypergastrinemia are a sign of atrophic autoimmune gastritis.
• Floor manometry of the upper gastrointestinal tract: with reflux gastritis, an increase in pressure in the duodenum to 200–240 mm water column is detected. (normally - 80–130 mm water column).
TREATMENT
Chronic non-atrophic gastritis
• Diet: for hypo- and achlorhydria, diet No. 2 is prescribed, for hyperacid conditions - diet No. 1.
• For gastritis caused by Helicobacter pylori - eradication (course of therapy - 1-2 weeks) •• Triple therapy ••• bismuth tripotassium dicitrate 120 mg 4 times / day for 28 days ••• metronidazole 200 mg 4 times / day in for 10–14 days ••• tetracycline 500 mg 4 times/day for 10–14 days •• Quadra-therapy ••• omeprazole 20 mg 2 times/day ••• tripotassium bismuth dicitrate 120 mg 4 times/day •• • tetracycline 500 mg 4 times a day ••• metronidazole 500 mg 3 times a day.
• In the absence of Helicobacter pylori and increased secretory function of the stomach •• Antacids, preferably non-absorbable, 1-2 hours after meals 3-4 times / day and before bed • Selective m-anticholinergic blockers (pirenzepine - 50 mg 2 times / day) • Blockers Histamine H2 receptors: ranitidine (150 mg 2 times a day orally or intramuscularly), famotidine (20 mg 2 times a day orally or intravenously) •• H+,K+-ATPase blockers (proton pump blockers) ) - omeprazole, rabeprazole 20 mg 2 times / day, lansoprazole 30 mg 2 times / day.
• Drugs that protect (envelop) the mucous membrane •• Sucralfate •• Bismuth tripotassium dicitrate (also has an antimicrobial effect against Helicobacter pylori).
Chronic atrophic gastritis • Drug therapy is carried out only during the period of exacerbation • Replacement therapy for secretory gastric insufficiency: natural gastric juice, pepsidil, hydrochloric acid with pepsin, acidin-pepsin (these drugs are contraindicated in the presence of erosions of the mucous membrane) • Replacement therapy for decreased excretory function of the pancreas glands (cholenzyme, pancreatin + bile components + hemicellulase, pancreatin, panzinorm forte) • Treatment of B12-deficiency anemia • Herbal medicine: herbal remedies that have an anti-inflammatory effect - infusion of plantain leaves, chamomile, mint, St. John's wort, valerian (1 tbsp. per glass of water) orally, 1/3–1/4 glass 3–4 times a day before meals for 3–4 weeks; plantain juice 1 tbsp. or plantaglucide 0.5–1 g 3 times a day • Drugs that improve tissue trophism and enhance reparative processes: nicotinic acid (1% solution IV from 1 to 10 ml for 10 days or IM 3–5 ml 20 days), solcoseryl 1–2 ml IM 20 days, inosine 0.2 g 3 times a day 40 minutes before meals 20–30 days, thiamine, pyridoxine, folic acid • Blockers of central and peripheral dopamine receptors for pain and severe dyspeptic symptoms (see below Reflux gastritis).
Reflux gastritis • Treatment is aimed at normalizing gastrointestinal motility and binding bile acids • To prevent the reflux of duodenal contents into the stomach, dopamine receptor blockers are prescribed (domperidone, metoclopramide, cisapride 10 mg 3 times a day 30 minutes before meals for 2-3 weeks ) • To neutralize bile acids that have a damaging effect on the gastric mucosa, chenodeoxycholic and ursodeoxycholic acids are used • To protect the mucous membrane from bile acids - antacids in the usual daily dose (aluminum-containing antacids have the ability to bind bile acids, so they are more effective).
Giant hypertrophic gastritis • Long-term treatment (2-3 months) • High-calorie, protein-rich diet • Antisecretory therapy • For treatment-resistant hypoproteinemia, repeated bleeding, surgical treatment (gastric resection) is indicated.
ICD-10 • K29 Gastritis and duodenitis
Application. Eosinophilic (allergic) gastroenteritis is a chronic disease characterized by predominantly eosinophil infiltration of the lamina propria of the gastric antrum mucosa, epithelium, pit glands with the formation of eosinophilic abscesses; characterized by damage to the small and large intestines, esophagus; often accompanies allergic diseases. Clinical picture: chronic diarrhea, abdominal pain, nausea, vomiting, weight loss, eosinophilia. Treatment: exclusion of allergy-provoking foods; diet No. 1; GCs provide long-term remission. ICD-10. K52.8 Other specified non-infectious gastroenteritis and colitis.
How to treat
To prevent the progression of the pathology, first of all, it is necessary to find out what provoked the increase in the acidity of gastric juice and why the protective mechanisms are not effective.
To visually assess the condition of the mucosa, specialists perform fibroesophagogastroduodenoscopy (FEGDS).
The study also allows you to take a tissue sample for histological analysis, test for the presence of Helicobacter pylori infection, and determine the acidity of gastric juice. A flexible tube with a camera is inserted through the mouth into the stomach of the person being examined, which allows one to see how inflamed the tissue is and whether there are any neoplasms or ulcers.
Only by eliminating factors that provoke increased production of hydrochloric acid and getting rid of Helicobacter pylori infection can you speed up the regeneration of the gastric mucosa
Drug treatment
Treatment of hyperacid gastritis includes taking medications, diet therapy, following a meal schedule (skipping meals is unacceptable), and physical procedures may be prescribed. You cannot treat the disease with pills or traditional medicine yourself, as this can harm the body and contribute to the transition of acute gastritis to chronic.
Any actions must be agreed with a gastroenterologist.
Helicobacter eradication
If acid-fast bacteria are present in the stomach, the patient is prescribed antibiotics that are not neutralized in an acidic environment. This may be Tetracycline, Azithromycin, Metronidazole, Levofloxacin, Amoxicillin, Clarithromycin, Tinidazole.
Triple therapy is considered standard, in which the patient takes two antibacterial drugs simultaneously with medications that suppress the production of hydrochloric acid (proton pump inhibitors). Bismuth-based agents can be added to this regimen to protect the gastric mucosa from the negative effects of acids.
The type of antibiotic and frequency of administration is determined by the doctor, based on the patient’s health condition and his or her tolerance to the medications. Duration of treatment is 7–14 days. If the three-component regimen does not work, then an additional antibacterial agent is recommended to the patient, and in extreme cases, the sensitivity of the bacterium to all antibiotics is checked and individual treatment is developed.
Restoring the pH of gastric juice
The treatment regimen for hyperacid gastritis includes drugs that normalize the acidity of gastric juice. These are drugs that inhibit the production of hydrochloric acid or neutralize it and protect the gastric mucosa.
The treatment regimen is determined individually by the doctor and may include taking several medications at the same time.
The following drugs may be prescribed to reduce the production of hydrochloric acid:
- histamine blockers (“Ranitidine”, “Famotidine”, “Cesera”);
- proton pump blockers (Lansopazole, Omeprozole, Esomeprazole);
- antacids (“Phosphalugel”, “Almagel”, “Maalox”);
- anticholinergics (“Gastrotsepin”).