February 1, 2022, 13:19 - Public news service - OSN Honored Doctor of Russia, Professor, Chief Physician of the State Clinical Hospital named after. V. Vinogradova Olga Sharapova named the Public News Service foods that are good for the pancreas and explained the effect of diet on the health of the digestive system.
According to statistics, pancreatic diseases lead among diseases of the digestive tract. In 2022, specialists from Kemerovo State Medical University estimated that over the past 10 years, the number of patients visiting medical institutions in the region with acute pancreatitis has increased by 110% []. At the same time, the number of people with pancreatic necrosis (death of organ tissue) reaches 30% of the total number of hospitalized people.
The City Clinical Hospital named after. V. Vinogradov in Moscow.
“200-300 patients with pancreatitis are admitted to our hospital every year,” notes Olga Sharapova. “Of these, 40-60 patients go through intensive care, and approximately 12-15 people, unfortunately, die. The mortality rate from this pathology is very high.”
Professor, Honored Doctor of Russia Olga Sharapova
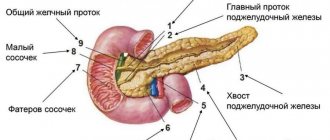
What is the pancreas?
The organ looks like an elongated lobular formation of a grayish color.
Its location is the abdominal cavity behind the stomach. The parameters of the human gland are: 14-22 cm long, 3-9 cm wide, 2-3 cm thick. The pancreas weighs approximately 75 grams. The pancreas is a component of the human digestive organs. The functions of the pancreas are to secrete juice with processing enzymes. In addition, the gland is responsible for hormonal levels. Fat, protein, and carbohydrate metabolism are the responsibility of this organ.
The endocrine functional features of the organ consist of the release of insulin and glucagon into the blood. Groups of cells are responsible for the production of these hormones. The number of cells in healthy people is usually sufficient to regulate carbohydrate (fat) metabolism. The destruction of one or another type of pancreatic cell can trigger the development of diabetes mellitus.
The close relationship with other digestive organs leads to disruption of the metabolism of the entire human system.
St. John's wort
In folk medicine, St. John's wort is recognized as a universal herb that can be used for various pathologies of the pancreas. The plant is used to prepare decoctions, infusions, tinctures and oils. To prepare tea you need one tbsp. l. pour boiling water (300 ml) of chopped St. John's wort and leave for 5 minutes. To improve the taste, the drink can be sweetened with honey.
The decoction is prepared according to the following recipe:
Diet for problems with the pancreas
- One tbsp. l. Pour boiling water (250 ml) over the dry product.
- Heat in a water bath, without bringing to a boil, for 15 minutes.
- Cool, filter.
- Bring the resulting volume to 300 ml by adding cooled boiled water.
To prepare the infusion you need 3 tbsp. l. pour dry St. John's wort with boiling water (500 ml). Insulate the container and leave to infuse for 4 hours. Then filter and take warm. You can prepare an alcohol tincture from St. John's wort. To do this you need:
- Two tsp. dry product, pour 100 ml of vodka.
- Keep the mixture in a dark, dry place for 5 days, shaking occasionally.
- Filter, squeeze out the cake.
Drink 20 drops diluted in 100 ml of water 30 minutes before meals once a day.
What are the symptoms of pancreatic disease?
When inflammation occurs, the pancreas begins to worry about pain in the region of the ribs on the left side. The qualitative characteristics of pain are cutting. Usually occurs after eating. As you know, it enters the duodenum and is digested by gastric juice.
Pancreatitis can be characterized by changes in pain intensity over a long period of time. They sometimes get worse, and sometimes there is no discomfort at all. If a person does not follow the diet, the pain develops into constant pain. Such pancreatic symptoms, in this case, are classified as chronic.
Typically, the symptoms of chronic pancreatitis are eliminated by a specially prescribed diet. If it is not followed, the person will experience flatulence, diarrhea, and heartburn. The process of inflammation causes loss of appetite. Inflammation also applies to the cellular level, since the cells of this organ secrete the juice necessary for the digestive system.
Symptoms
Acute pancreatitis is characterized by attacks of girdle pain, fever, possibly increased temperature, vomiting, stool disorders, both diarrhea and constipation, belching or vomiting, as well as decreased blood pressure, sweating, dry mouth. The skin becomes pale and facial features may become sharper. This condition is life-threatening.
The chronic stage is characterized by intolerance to many foods, inconsistent oily stools, belching, nausea, and abdominal pain, especially after eating. With chronic pancreatitis, vitamin deficiency develops and weight loss is possible. Diabetes mellitus often occurs in those suffering from pancreatitis.
What is the development of pancreatic disease?
Gradually, the number of working cells decreases. Pancreatic cells are replaced by secreting tissue of the pancreas. As a result of digestive disorders, diabetes develops.
This occurs due to disturbances in carbohydrate metabolism, as well as insulin emissions. The ejective nature of the cells leads to low levels of glucose in the blood. The next stage in the development of the disease will depend on the damaging factor. If very few pancreatic cells remain, the process will lead to insulin deficiency.
Receptors may stop accepting glucose, which will lead to excess insulin in the blood. Elevated blood glucose levels lead to diabetes mellitus. The disease is almost always associated with excess body weight.
Diabetes mellitus associated with excess insulin is classified as type 2. The development of the disease can be prevented by eliminating certain foods from the diet. By the way, pancreatitis can also be treated with proper nutrition, but only in the initial stage of the disease.
If the diet is not followed, excess insulin will have a destructive effect on all organs, and especially on the human digestive system. At the same time, some processes, for example, necrotic ones, will be irreversible.
Defective folding
- In recent years, defective folding in the ER has been implicated as a cause of several chronic diseases, including: diabetes mellitus;
- non-alcoholic fatty liver disease (NAFLD);
- cancer;
- Alzheimer's disease.
- Ca deposition;
- They found that in the presence of prediabetes, proinsulin synthesis in β-cells occurs more actively, and due to this, protein folding is disrupted. Misfolded proteins accumulate in the ER, causing stress.
- insulin resistance (IR);
- causes ER stress in β cells;
- CCAAT/ homologous protein binding enhancer gene;
How can you avoid pancreatic disease?
Pancreatitis is a disease of people who are prone to systematic overeating. In this case, fat metabolism is disrupted, and the risk of disease increases significantly. Sometimes an inflammatory process in the pancreas can occur due to injury, for example, a wound to the abdomen.
A diet for diabetes mellitus accompanied by chronic pancreatitis involves reducing the consumption of carbohydrates. Fast carbohydrates are a source of glucose. If they are removed from the menu, glycemia will return to normal. The negative effect on the pancreas will stop. Some types of pancreatitis occur due to allergies to foods or medications. To avoid the development of the disease, it is enough to avoid their use.
Failure to adhere to the diet can lead to complete disruption of the functioning of the pancreas. In this case, the dead organ is removed surgically.
To prevent surgery, medications that affect hormones are prescribed. The action of medications is aimed at easing the functioning of the inflamed organ.
How foods affect pancreatic health
The pancreas performs several significant functions in the human body. This body is involved in:
- processing sugar, producing insulin;
- digests food by producing digestive enzymes.
The food we include in our diet affects the health of the organ. If a person adheres to the wrong diet, an inflammatory process called pancreatitis may begin in his tissues.
“Pancreatitis can occur in young people, middle-aged people, and pensioners,” comments Olga Sharapova. — The disease spares no one and often leads to death. Its cause is poor nutrition, spicy and salty foods, fast food, and alcohol. The disease can occur even after three spoons of adjika, a jar of pickles and 100-200 grams of vodka. And you don’t have to eat fatty, salty and spicy foods all the time. You can plant the pancreas even after one feast.”
Just one party can lead to pancreatitis (Photo: pexels.com)
How is pancreatic disease treated?
Since the development of pancreatic inflammation varies, medications should never be taken independently. Therefore, the doctor must tell you how to treat the pancreas. Taking pills on your own can have serious consequences.
If the development of the disease follows the first type of diabetes, then dietary nutrition is also prescribed. The diet for this variant of the disease involves reducing the consumption of fats, carbohydrates, and flour. Blood sugar may be elevated by these foods. As a result of their consumption, the pancreas begins to secrete excess insulin. The lifespan of the organ is significantly reduced.
To avoid irritation of the gastric mucosa, it is often recommended to exclude apples and smoked products from the diet. Products available for consumption should be divided into 4-5 meals a day. In this way, the pancreas symptoms of the disease will be reduced to zero, and pancreatic juice will be released evenly at a certain time and in the right amount.
To avoid nutritional deficiencies, food must contain vitamins and minerals in proper quantities.
The correct treatment for the pancreas is proper nutrition. If you follow the regimen, you will not be bothered by complications and unpleasant symptoms. The main complication of chronic pancreatitis is diabetes mellitus. In most cases, its occurrence can be prevented. Timely treatment and preventive measures can alleviate the symptoms that appear. Timely contact with specialists will even help delay the occurrence of complications. Regeneration of pancreatic cells is enhanced to a sufficient extent only with correct and timely therapy.
Chamomile
An effective natural remedy for pancreatic diseases is chamomile. Among the main capabilities of the plant it is worth highlighting:
- anti-inflammatory effect;
- analgesic, disinfecting effect;
- protection of the mucous membranes of the gastrointestinal tract (gastrointestinal tract) from the aggressive influence of acid produced by stomach receptors.
Chamomile tea will help heal the pancreas. Two tbsp. l. Pour boiling water (200 ml) over the dried flowers of the plant. Infuse the drink for 15 minutes. Filter. Tea can be slightly sweetened with honey.
Important! In acute pancreatitis, tea intake is strictly limited. In case of a chronic course of the disease, the course duration is one to two months.
Chamomile tea is one of the effective treatments for chronic pancreatitis
Read also: What is pancreatic necrosis
The next form of remedy is chamomile decoction. In a saucepan you need to put 2 tbsp. l. dry product and pour boiling water (200 ml). Place the dishes in a water bath and simmer for 15 minutes. Pour the product into a thermos and leave to infuse for 60 minutes. Filter.
Add boiled water to bring the volume of the drink to 200 ml. Drink a third of a glass of the decoction strictly before meals. Duration of treatment is two to four weeks. Chamomile decoction can be used in the treatment of pancreatitis in childhood.
To prepare an infusion of chamomile, you need one tbsp. l. put flowers and herbs in a thermos and pour boiling water (200 ml), leave for two to three hours, filter. Take the product warm between meals up to four times a day. Dose – ½ cup.