Pancreatitis is inflammation of the pancreas.
The pancreas is the second largest gland in the digestive system (after the liver). It plays an extremely important role in the digestion process.
The pancreas produces pancreatic juice, which contains more than 30 different enzymes. It contains components necessary for the breakdown of fats, proteins, and carbohydrates. Up to 800 grams are produced daily. pancreatic juice, which flows through the pancreatic duct into the duodenum. To prevent the juice from corroding the tissue of the pancreas itself, enzymes are initially produced in an inactive form. To transform them into an active form and start the digestive process itself, it is necessary to interact with bile, which normally should occur in the duodenum. If bile enters the pancreatic duct or if the outflow of pancreatic secretions is obstructed, premature activation of enzymes occurs, which leads to the process of self-destruction of the pancreas. The gland begins to digest itself - tissue necrosis begins, pancreatitis occurs.
What role does the pancreas perform in the body?
The content of the article
The pancreas performs an important function in the human body: it is involved in digestion. Undoubtedly, the digestion of food is of great importance for the existence of a living organism.
The structure of the pancreas
As you know, destructive or restorative processes constantly occur in the body. This requires building materials, which people take in the form of food. But food must be properly processed and supplied to the body in the form of final products necessary for life. In this process, the lion's share of the special substances necessary for digestion comes from the pancreas. If the pancreas is damaged, the digestive process will not work properly.
How to detect the disease?
First, the doctor examines the patient, palpates, asks about symptoms, and studies the medical history.
Then he gives a referral for instrumental and laboratory diagnostics:
- blood tests: general, biochemical and glucose;
- urine amylase test;
- coprogram;
- radiography;
- endoscopy;
- ultrasound examination (ultrasound);
- angiography;
- retrograde cholecystopancreatography;
- electrocardiography (symptoms of the abdominal form of infarction are similar to those of pancreatitis);
- computer and magnetic resonance imaging (CT and MRI).
Where does pancreatitis come from?
Acute inflammation of the pancreas is largely due to a violation of the diet - eating too spicy, fatty foods, prolonged hunger. This problem is mainly found in low-income countries where the population is exposed to unhealthy foods. A feature of modern cuisine is connected with this: in our country they eat mainly fatty, spicy dishes.
Alcohol also affects the function of the pancreas, especially counterfeit drinks, which are widespread in our market.
Dangerous consequences of pathology
What to do if the pancreas is enlarged? Look for the cause of inflammation, and at the same time change your lifestyle and diet. Sometimes an enlargement of the pancreas in a child occurs during therapy with antibiotics and metronidazolam, as a side effect of the drugs. The doctor’s response when treating pancreatitis without symptoms is to observe and study the dynamics of the pathology. Treatment is necessary to avoid the development of complications.
Acute inflammation is fraught with diabetes mellitus, peritonitis, the appearance of cysts, and damage to neighboring structures. Chronic pancreatitis provokes enzymatic deficiency, disrupts the flow of bile, and increases the risk of stone formation. Complications relate to cell changes - cancer, ascites, chronic pain. The disease is becoming younger and is detected before the age of 5 years.
What are the signs of pancreatitis?
The main symptom of pancreatitis is pain, which is localized in the epigastric region (stomach), has a calming character and sometimes spreads to the neck area. In addition, inflammation of the pancreas is characterized by dry mouth, bloating, nausea and frequent vomiting.
Bloating
Nausea
If you have any of these signs, you should definitely consult with a gastroenterologist, who will diagnose using abdominal ultrasound and other additional examinations and prescribe adequate treatment.
Power control
In order for treatment to be effective, it is necessary to identify the reason why the gland could increase in size. In any case, prescribing a diet is the first point in treatment. Most often, the diet consists of protein foods with a limited amount of fats and carbohydrates. The patient should forget about such products as:
- alcohol;
- dairy products with a high percentage of fat;
- broth and soups prepared with it;
- vegetables and fruits that have not undergone heat treatment;
- sweets and baked goods.
Products that are allowed:
- poultry, fish;
- fermented milk products;
- dietary bread;
- any cereals and pasta;
- steamed vegetables;
- weak tea;
- baked fruits.
When the pancreas greatly increases in size, a proper diet may not have any effect. For example, in cases of the development of cystic formations, only surgical intervention can help. This also applies to pancreatitis, which cannot be cured with diet alone.
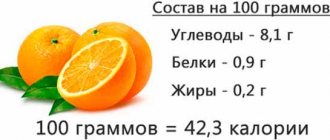
When choosing products for cooking, you can rely on the following table:
| Forbidden | Allowed |
| Sweet products, creams | Natural sweets, dried bread, jam, honey, crackers, marshmallows |
| Fried, smoked, spicy | Chicken, lean fish |
| Legumes, all mushrooms | Low-fat lactic acid products |
| Sorrel, onion, garlic, radish | Porridge cooked in water |
| Carbonated drinks, alcohol | Dried fruit compote, jelly, sweet tea |
Below is a menu with which you can provide yourself with a complete and varied diet:
| Breakfast | Snack | Dinner | Afternoon snack | Dinner |
| Semolina porridge with apple and green tea; rice porridge with orange; oatmeal and jelly; rice porridge with crackers; barley porridge with honey | Pumpkin puree; baked apple; cottage cheese with honey and tea; steam cutlet and rosehip infusion; grated apple with cottage cheese and biscuits | Vegetable broth with boiled meat, crackers; carrot soup with other vegetables and meatballs, compote; vegetable puree soup, meatballs; low-fat steamed fish, mashed potatoes; rabbit cutlets, stew | Low-fat cottage cheese with fruit; low-fat yogurt with crackers, honey and apple; steam omelette; cottage cheese casserole; baked apple | Beef cutlet, compote; potato casserole with minced meat, jelly; baked fish with vegetables; mashed potatoes, steamed fish; vegetable casserole, boiled chicken |
At the end of the acute period, the patient can eat quite varied, the main thing is a gentle cooking regime.
How does autoimmune pancreatitis manifest?
The pancreas produces digestive juices that contain active enzymes. It is through them that proteins, fats and carbohydrates are digested in the intestinal lumen. In addition to participating in digestion, pancreatic juice is also beneficial for the mucous membranes of the intestinal tract.
The decomposed tissue soon turns into a new one - the mucous membrane immediately undergoes regeneration. There is also a saying: “A man has breakfast with one mucous membrane and lunch with another.” If the process of tissue self-renewal is disrupted, the mucous membrane in the intestinal lumen becomes ulcerated.
During pancreatitis, digestive juices are not found in the intestinal lumen, but in other places, for example, in the abdominal cavity or in the pancreatic tissue itself, where the regenerative process is not as intense as in the intestines, so the aggressive juice significantly damages the body. The process of autolysis begins - pancreatic juice absorbs its own tissue.
During the inflammatory process, digestive juices produced by the pancreas can also enter the bloodstream (here digestive enzymes begin to digest the wall of the blood vessel), through which it reaches the brain, subcutaneous adipose tissue, and so on.
If a fulminant form develops during pancreatitis, the person will die within a few hours due to the above pathological processes.
As you can see, there are several forms of acute pancreatitis. A fulminant form of inflammation of the pancreas leads to death (death) in just six hours. In addition, there are forms that worsen as a result of treatment, the acute process becomes chronic, and the person must live with the pathology for the rest of his life, following a special diet.
Methods for diagnosing pancreatitis
The greatest difficulty is in diagnosing chronic pancreatitis.
.
Chronic pancreatitis often develops as an independent disease, and not as a complication of acute pancreatitis. At the same time, it is better to start treatment of chronic pancreatitis at an early stage, without leading to acute attacks.
For timely detection and diagnosis of chronic pancreatitis, it is necessary to undergo an annual preventive examination, as well as consult a gastroenterologist at the first suspicion of the disease.
The following diagnostic methods can be used to diagnose pancreatitis:
General blood analysis
A general blood test for pancreatitis reveals an increase in leukocytes (tens of times), a significant increase in ESR.
More information about the diagnostic method
Blood chemistry
In pancreatitis, the main indicator of biochemical analysis is pancreatic amylase (its level increases tenfold during the disease). An increase in other pancreatic enzymes, glucose and cholesterol is also expected.
More information about the diagnostic method
Biochemical urine analysis
In the case of pancreatitis, an increase in a biochemical urine test such as disstase (alpha-amylase) should be expected. The most indicative analysis of fresh urine (in CITO mode).
More information about the diagnostic method
Stool examination
For pancreatitis, a stool examination (coprogram) is performed. The study determines the degree of indigestion of food, as well as the ratio of digestive enzymes. Bacteria can be identified that have multiplied as a result of disruption of the intestines and the accumulation of food debris in it.
Ultrasound
Ultrasound of the pancreas allows you to confirm the diagnosis (detect an inflammatory process in the pancreas). Using ultrasound, you can evaluate the size of the pancreas, the condition of its tissue and ducts.
More information about the diagnostic method
X-ray of the abdominal cavity
X-rays can detect stones in the pancreas and its ducts. Currently, the preferred research method is computed tomography of the abdominal organs.
More information about the diagnostic method
MSCT of the abdominal cavity
Computed tomography of the abdominal cavity can identify complications of pancreatitis - such as stones, cysts and tumors (benign or malignant), and damage to neighboring organs.
More information about the diagnostic method
Magnetic resonance imaging (MRI)
MRI is the most informative method for examining the pancreas in cases of suspected pancreatitis. The method makes it possible to detect chronic pancreatitis in the early stages, even before the appearance of changes in soft tissues. Using MRI, differential diagnosis of chronic and acute pancreatitis is possible.
More information about the diagnostic method
Gastroscopy
Gastroscopy for pancreatitis makes it possible to assess the involvement of the stomach and duodenum in the pathological process. In some cases, gastroscopy can be used to determine what triggered the development of acute inflammation.
More information about the diagnostic method
Sign up for diagnostics To accurately diagnose the disease, make an appointment with specialists from the Family Doctor network.
What is the principle of treatment for pancreatitis?
Unfortunately, medicine does not yet know how to influence aggressive enzymes in pancreatitis. There are medications that prevent the formation of the final corrosive product, but once such a substance is already produced, it is impossible to get rid of it.
The initial stages of pancreatitis are treated with a special diet, enzymes and other medications.
Diet
The main treatment for acute pancreatitis is surgery. Its essence is as follows: doctors limit the juice secreted by the pancreas so that it does not damage organ tissue. Aggressive sap can be removed by drainage, but only partially. In fact, the operation is palliative - there is no complete cure, doctors only alleviate the person’s condition.
The main causes of gland enlargement
When a person has an enlarged pancreas, this is not considered a disease. In most cases, this may be a congenital trait that is harmless from a health point of view. To find out the exact diagnosis of the disease, you need to see a doctor and perform the appropriate studies and tests. Pancreatic enlargement can be divided into 2 types:
- Total, when the gland increases evenly over the entire surface.
- Local, when one part or area of the surface suffers. For example, when (the head of the pancreas is enlarged).
Reasons for complete enlargement of the gland:
- hereditary anomaly;
- toxic effects due to alcoholic beverages or the effect on the body of certain medications;
- damage to nearby internal organs.
Local enlargement of the pancreas:
- when cysts form;
- purulent contents;
- pancreatitis.
And this is an inexhaustible list of reasons for the development of this disease. Only the attending physician can identify the real cause by diagnosing the whole organism.