Pancreatitis is an inflammatory process of the pancreas, which is sometimes complicated by necrotic phenomena. It can occur in both acute and chronic forms. Since the importance of the pancreas for the digestion process is very great, a violation of its function can cause a sharp decrease in the quality of life, deterioration of digestion and metabolic failures in the body.
The entire organ or its individual parts can become inflamed, and in cases requiring emergency assistance, tissue disintegration begins, which becomes the cause of suppuration and abscesses.
Causes
Among the reasons that cause pancreatitis more often than others are the following:
- alcohol abuse;
- cholelithiasis and other gallbladder diseases;
- surgical intervention in the stomach or biliary tract;
- ulcer;
- abdominal trauma;
- use of heavy medications;
- infectious phenomena (hepatitis caused by a virus, endemic mumps, etc.);
- parasitic infections;
- congenital disorders of the pancreatic duct;
- endocrine system imbalance;
- metabolic failure;
- genetic predisposition.
Symptoms
Symptoms depend on what form of pancreatitis is observed in the patient.
Acute form of the disease
In the acute form, the inflammatory process develops quickly with a sharp deterioration in the person’s condition. The risk of irreversible anatomical and functional changes in the organ is high, and death can occur if assistance is not provided in a timely manner. The duct into the duodenum becomes so narrowed that the enzyme solution cannot escape and remains inside the pancreas, destroying its epithelium from the inside. Due to cell damage, swelling occurs, which further aggravates the condition.
In acute pancreatitis, the patient feels periodic or constant acute pain in the left hypochondrium, which can be girdling or sharp. After drinking alcohol or fatty foods, the pain becomes stronger and the following symptoms appear:
- pain in the abdomen, under the shoulder blade, or in the back;
- painful prolonged hiccups;
- heaviness in the stomach;
- heartburn, nausea and vomiting with particles of undigested food, and after a while – with inclusions of bile;
- flatulence;
- yellowness of the skin;
- loose stool.
Severe pain may cause fever, cold sweat, and increased heart rate. This is often accompanied by pressure surges, shortness of breath, and hardening of the abdominal muscles. Sometimes the pain is so unbearable that the patient loses consciousness.
With such symptoms, you should urgently call an ambulance, as the patient’s condition is worsening every minute.
Chronic form of the disease
The symptoms that occur in the chronic form are not so painful, but they cause a huge amount of discomfort and no less negatively affect the body:
- after eating fatty, spicy or smoked foods, coffee or dark chocolate, pain appears within a quarter of an hour, lasting from an hour to a day;
- the face acquires a yellowish or grayish tint;
- in the area of the waist and lower back, the skin becomes bluish;
- frequent belching after eating;
- the presence of a yellowish coating on the tongue;
- constipation or diarrhea with whitish inclusions of undigested fatty foods;
- significant weight loss;
- stable loss of appetite;
- dryness and flaking of the skin, as well as brittle nails, reminiscent of manifestations of vitamin deficiency.
What is pancreatitis?
Pancreatitis is inflammation of the pancreas.
Pancreatitis refers to a whole group of diseases and ailments that occur as a result of inflammation of the pancreas or disruption of the functioning of the pancreas.
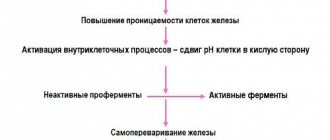
When the disease pancreatitis occurs in the pancreas, a process begins to occur in which the enzymes secreted by the gland are not released into the duodenum, but are activated in the gland itself and begin to destroy it, that is, self-digestion occurs.
The enzymes and toxins released during this process are released into the blood and can cause serious damage to other organs such as the brain, lungs, heart, kidneys and liver.
Which doctor should I go to?
In the chronic form of pancreatitis, the first attacks can be very strong, but over time their intensity weakens. Constant discomfort makes you wonder what to do and who to contact for diagnosis and treatment.
First of all, you should contact a general practitioner, who will listen to complaints and refer the patient to a gastroenterologist. Typically, this doctor will conduct an extensive examination to confirm the suspected diagnosis. During the diagnosis, a meeting with a nutritionist and endocrinologist may be necessary.
During the examination for pancreatitis, the following tests are performed:
- general clinical tests of blood, feces and urine;
- biochemical blood parameters;
- Ultrasound and x-ray of the abdominal organs;
- esophagogastroduodenoscopy (EGDS);
- cholangiopancreatography;
- endoscopy;
- MRI and/or CT scan of the pancreas;
- gastroscopy of the pancreas.
Treatment
After a detailed examination, the attending physician prescribes a course of treatment for pancreatitis, consisting of many components:
- drug therapy, which includes antispasmodics, M-anticholinergics and H2-blockers;
- anti-enzyme drugs to stop processes that destroy the gland - cytostatics and proton pump blockers;
- pancreatic enzymes;
- medications to normalize the acid-base balance;
- vitamin therapy with complex preparations including lipoic acid and cocarboxylase;
- oral prokinetics.
In case of severe attacks of pancreatitis, it is necessary to observe a regime of rest and rest. To normalize digestion and the general condition of the patient, nutrition is provided through a dropper with the introduction of electrolytes and essential amino acids.
An important place is occupied by dietary nutrition according to the special Pevzner diet - diet No. 5. At the time of rehabilitation, sanatorium treatment shows good results.
Acute pancreatitis is treated exclusively in a hospital setting. If the case is advanced and cannot be treated, then the surgeon performs pancrectomy - surgical treatment of pancreatitis, after which there will be a long recovery and a lifelong diet.
Consultations with a doctor online Taking care of your health is a life priority for everyone.
Communicate with doctors online and receive qualified assistance without leaving your home. Try it Please note! The information on this page is provided for informational purposes only. To prescribe treatment, you must consult a doctor.
Chronic pancreatitis
In population studies, it was noted that men develop chronic pancreatitis more often than women. The proportion of alcoholic pancreatitis increased from 40 to 75%. This cause of chronic pancreatitis is more common among men. There is also an increase in the incidence of pancreatic cancer, which develops against the background of chronic pancreatitis.
As you know, diabetes is literally becoming the disease of the century. At the same time, more and more facts are accumulating about the connection between chronic pancreatitis and diabetes mellitus. Chronic inflammation and scarring (replacement of gland tissue with connective tissue) in the pancreas leads to disruption of the production of adequate amounts of digestive enzymes (amylase, lipase) necessary for digesting food. In addition, insulin production decreases, which can cause the development of diabetes.
Causes of chronic pancreatitis The main cause of chronic pancreatitis, as well as acute pancreatitis, is alcohol abuse. Other reasons include:
- High calcium levels in the blood (hypercalcemia);
- Congenital anomalies of the pancreas;
- Cystic fibrosis (hereditary disease of the endocrine glands, characterized primarily by damage to the gastrointestinal tract and respiratory organs);
- High levels of triglycerides in the blood (hypertriglyceridemia);
- The use of certain medications (hormonal drugs (estrogen-containing drugs, corticosteroids), thiazide diuretics (hypothiazide) and azathioprine);
- Long-term difficulty in the outflow of pancreatic juice containing digestive enzymes as a result of scar changes in the area of the major duodenal papilla (the location of the anastomosis of the pancreatic duct and the common bile duct) or blockage with gallstones;
- Autoimmune damage to the pancreas - with this pathology, the immune system reacts to the structures of the pancreas’s own tissues as if they were foreign.
Hereditary pancreatitis, which develops as a result of genetic mutations, can also be observed. In some cases, the cause of chronic pancreatitis cannot be determined; such pancreatitis is called idiopathic.
Symptoms of chronic pancreatitis Chronic inflammation of the pancreas can lead to damage to both the gland itself and adjacent tissues. However, it may take years for clinical manifestations of the disease (symptoms) to appear. There is a certain proportion of patients with chronic pancreatitis who do not notice any pronounced symptoms of the disease, however, most people suffering from this disease experience periodic attacks of abdominal pain, which can be quite severe. Sometimes the pain can be constant. In addition to pain, the following symptoms may cause concern in chronic pancreatitis:
- Feeling sick and vomiting;
- Increased body temperature;
- Weight loss, even if you maintain your appetite and eat regularly;
- Fatty and foul-smelling stools (steatorrhea) resulting from poor digestion of fats.
- Diagnosis of chronic pancreatitis
If the patient notices long-lasting pain in the upper abdomen (especially with chronic alcohol consumption), then you should consult a doctor to rule out chronic pancreatitis or other diseases.
The doctor prescribes diagnostic procedures, the main of which include:
- Blood test;
- General stool analysis;
- Ultrasound examination (ultrasound).
Chronic pancreatitis is indicated by changes in the size and compaction of pancreatic tissue. Ultrasound diagnostic methods also include endoscopic ultrasonography (EndoUS). This study uses an endoscope with an ultrasound transducer at the free end. An ultrasound probe inserted in this way allows a more detailed image of the gastrointestinal tract and pancreas to be obtained.
- Computed multislice tomography (MSCT)
This research method is based on obtaining layer-by-layer X-ray images of the human body with their subsequent processing on a computer. During this study, the patient lies on a special table, and the device itself moves along the body, taking many pictures. CT allows you to determine in relatively detail the structure of the pancreas and adjacent tissues.
- Magnetic resonance imaging (MRI)
The method of performing MRI is similar to CT, but it is based not on the use of X-rays, but on the effect of nuclear magnetic resonance.
- X-ray examination of the biliary tract and pancreas
The test is called endoscopic retrograde cholangiopancreatography (ERCP) and involves the introduction of a radiopaque substance (a substance that is clearly visible on radiographs) using a thin plastic tube under the control of an endoscope (an optical flexible instrument) into the major duodenal papilla (the junction of the common bile duct and the pancreatic duct ). This diagnostic method allows you to obtain an x-ray image of the pancreatic duct and common bile duct and determine their damage or narrowing. ERCP is a relatively dangerous diagnostic method as it can provoke an exacerbation of pancreatitis.
- A study of the ability of the pancreas to produce digestive enzymes.
If there are disturbances in the process of digesting food and weight loss, the doctor may prescribe special tests to evaluate the function of the pancreas. These diagnostic tests involve the introduction of special stimuli that stimulate the production of various enzymes by the pancreas, with their subsequent quantitative determination.
Treatment of chronic pancreatitis The main goals of treatment of chronic pancreatitis are to eliminate the cause of pancreatitis (for example, stopping alcohol consumption), control (reduce) pain and improve digestion of food. For chronic pancreatitis caused by alcohol consumption, stopping drinking is the most important step in treating the disease. In the early stages of the disease, even just one refusal to drink alcohol can lead to relief of even severe pain. Continued consumption of alcohol during chronic pancreatitis leads to progression of the disease and a significant increase in the risk of complications and death. Unlike acute pancreatitis , in which the pain often disappears within a few days or a week, the pain of chronic pancreatitis may persist for a longer period of time. In some cases, pain may be relieved by administration of enzyme medications, which reduces the burden on the pancreas and may reduce pain. To improve food digestion, they resort to prescribing enzyme preparations. The point of this type of treatment is the additional introduction of missing enzymes, which is necessary for digesting food and restoring normal body weight. Enzyme preparations should be taken immediately before or during meals. Also in treatment, it is important to observe some dietary features (food should be taken in small portions, food should not be fatty) to reduce the load on the pancreas.
Prevention of chronic pancreatitis Despite the fact that the development of pancreatitis cannot always be prevented, there are still a number of measures to reduce the risk of this disease:
- non-alcohol abuse - increased consumption of alcoholic beverages is the main cause of chronic pancreatitis and a provoking factor for exacerbations of pancreatitis;
- stopping smoking - smoking tobacco increases the risk of pancreatitis, especially in combination with alcohol;
- limiting the consumption of fatty foods - eating fatty foods leads to an increase in the level of fats in the blood.