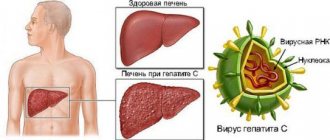
The liver in the human body performs many vital functions: it synthesizes proteins, hormones, enzymes, bile, cholesterol, cleanses the blood of toxins, excessive amounts of hormones, microorganisms and metabolic products, and is actively involved in the metabolism of microelements, vitamins and carbohydrates. A number of factors can lead to liver damage and disruption of its function. With hepatitis, the liver tissue becomes inflamed, areas of necrosis may appear in it, leukocytes accumulate, and a small amount of connective fibrous tissue is formed. Although the structure of the liver lobules is not disturbed, such inflammation may be accompanied by stagnation of bile and disruption of the functioning of hepatocytes.
Causes of hepatitis
Non-infectious hepatitis occurs for various reasons:
- Alcoholic hepatitis occurs due to many years of alcohol abuse. Because of it, the metabolism in hepatocytes is disrupted, and they begin to collapse;
- Non-alcoholic steatohepatitis does not occur due to alcohol intake, but the changes in the liver with it are very similar to those that occur with alcohol;
- Drug-induced hepatitis is formed due to the use of various medications that have a toxic effect on the liver (oral contraceptives, antibiotics and anti-tuberculosis drugs);
- Toxic hepatitis is caused by alcohol substitutes, poisonous mushrooms, arsenic compounds, lead, benzene, toluene and other substances that destroy liver cells;
- Autoimmune hepatitis leads to disruption of the immune system, which begins to destroy normal liver cells;
- Metabolic hepatitis occurs due to various hereditary diseases associated with metabolism. These include Wilson's disease, in which copper metabolism is disrupted in the body, hemochromatosis, in which increased absorption of iron is observed in the intestines, etc.;
- Reactive hepatitis is formed due to exposure to toxins and metabolic products that enter the blood during diseases of other organs (pancreatitis, stomach ulcers, autoimmune and endocrine diseases);
- Primary biliary hepatitis occurs due to obstruction of bile flow and bile outflow, leading to damage to liver tissue.
Viral hepatitis - symptoms and treatment
It is advisable to consider the detailed pathogenesis of each type of viral hepatitis in separate articles. It is enough to understand the options for normal functioning of the liver and the general mechanisms of its pathology.
The formation and metabolism of bilirubin is normal
Bilirubin is a product of the transformation of hemoglobin (Hb), a kind of “waste” that must be removed from the body. It is formed mainly from Hb, which is released from red blood cells (lifespan 120 days). The destruction of hemoglobin and the formation of bilirubin occurs in the cells of the phagocytic mononuclear cell system:
- Vysokovich-Kupffer cells, which capture and process old non-functional liver blood cells;
- splenic phagocytes - cells of the immune system that protect the body by absorbing harmful foreign particles or dying cells.
A brief scheme for the formation of bilirubin looks like this:
Red blood cells (in the spleen) - Hemoglobin (in the spleen) - Verdoglobin (a product of the enzymatic oxidation of the non-protein part of hemoglobin, formed in the cells of the macrophage system) - Biliverdin (an intermediate product of the breakdown of hemoglobin).
Stages of formation and excretion of bilirubin:
- First phase: formation of free (indirect) bilirubin in the spleen and hepatocytes (liver tissue cells).
- The second phase: its entry into the blood and transfer by albumins (simple water-soluble proteins) into hepatocytes.
- Third phase: binding of free bilirubin with glucuronic acid in hepatocytes (formation of bound, or direct, bilirubin).
- Fourth phase: release of direct bilirubin by hepatocytes as part of bile into the bile capillary.
- Fifth phase: entry of bilirubin-diglucoronide (direct bilirubin) into the duodenum in the form of bile.
Bilirubin diglucoronide can undergo two transformations:
- In the large intestine, it is converted into stercobilinogen, a substance created by colonic bacteria. Stercobilinogen is yellow in color and is further excreted in the feces in the form of stercobilin (provides the normal brown color of stool).
- In the small intestine it is converted into urobilinogen, a colorless product of the reduction of bilirubin, formed under the action of small intestinal bacteria. It is excreted through the kidneys with urine in the form of urobilin, and also enters the portal vein system into the liver with subsequent destruction.
Pathology of bilirubin metabolism in viral hepatitis
Damage to hepatocytes leads to a weakening of the uptake of free bilirubin and disruption of the process of addition of glucuronic acid to it (phase 3). As a result, the content of free bilirubin in the blood increases. Impaired transport of conjugated bilirubin into the bile capillary (phase 4) leads to an increase in conjugated bilirubin in the blood. At the same time, intrahepatic cholestasis is observed, i.e., the level of both free and bound bilirubin in the blood increases, and there is more of the latter (the skin turns yellow).
Bound bilirubin (the urine becomes dark in color) and bile acids penetrate from the blood into the urine, which reduce the surface tension of the urine and cause it to foam easily. Little bound bilirubin enters the intestines - the stool becomes discolored. Due to intrahepatic cholestasis and impaired bile secretion, little bile enters the intestine. Since bile is necessary for the digestion of fatty foods and the absorption of fat-soluble vitamins, due to its lack, a lot of fat remains in the stool (steatorrhea), and the absorption of vitamin K is impaired. Due to the low level of vitamin K, the synthesis of prothrombin in the liver decreases, as a result, blood clotting worsens .
General pathogenetic mechanisms in the liver during hepatitis
Cytolysis syndrome (cytolytic syndrome) is a set of signs indicating a disruption of the liver due to a violation of the integrity of liver cells and the release of liver enzymes into the blood. The degree of increase in the activity of aminotransferases (enzymes that reflect the functionality of the human liver) indicates the severity of the cytolytic syndrome, but does not directly indicate the depth of the dysfunction of the organ.
There is an empirical de Ritis coefficient - AsAT/AlAT. It reflects the ratio of the activity of serum AST (aspartate aminotransferase) and ALT (alanine aminotransferase). The de Ritis coefficient approximately indicates the predominant damage to one or another parenchymal organ. For hepatitis, its value is less than 1.33. In a healthy person it is in the range of 0.91-1.75.
Cholestasis syndrome is characterized by a violation of the outflow of bile. It lingers in the intrahepatic bile ducts, causing the liver tissue to swell and swell. There is an accumulation of bilirubin, cholesterol, β-lipoproteins and alkaline phosphatase in the blood. Also characteristic is the appearance of cholemia, a pathological syndrome characterized by the accumulation of bile acids in the blood. Normally, the acid content in the blood is 5-25 mmol/liter. If their number increases, cholemia develops, which is accompanied by itching, scratching, damage to the central nervous system (CNS) and staining of the skin through bile (80% bile acids + bilirubin).
Mesenchymal-inflammatory syndrome - damage to the liver parenchyma, connective tissue stroma, reticuloendothelium. Clinically expressed by enlarged liver and spleen, increased body temperature, acute phase parameters, as well as the level of autoantibodies, thymol test, β and γ proteins.
Immunosuppressive syndrome (secondary immunodeficiency) is a temporary or permanent depression of the immune system that develops under the influence of certain chemical and physical influences on the body, as well as due to certain infectious processes.
Biliary dyskinesia syndrome is a violation of their motility. It may occur due to changes in the innervation of the biliary tract due to the relative predominance of the tone of the vagus or sympathetic nerve.
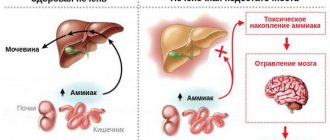
Hepatic cell failure is a pathological process in which massive death of liver cells occurs. This condition is characterized by a decrease in albumin (manifested by edema syndrome) and a decrease in prothrombin (manifested by lethargy, fatigue, nausea, vomiting, hemorrhagic rash) [2][3][5][7][9].
Symptoms of hepatitis
In the early stages, hepatitis can occur completely unnoticed without specific symptoms. The intensity of symptoms usually depends on the cause of hepatitis, on the activity of the pathological process and its duration.
Typically, the main symptoms of hepatitis are:
- Decreased appetite;
- Vomiting, nausea, heaviness in the abdomen;
- Yellow color of sclera and skin;
- Malaise and weakness;
- Pain in joints and muscles;
- Fever.
Signs of chronic hepatitis
Chronic hepatitis is characterized by weakness and fatigue, and asthenic syndrome manifests itself. The patient's condition worsens significantly if liver cirrhosis develops. Then the signs of chronic hepatitis become jaundice (yellowness of the sclera, icteric skin tone, darkening of urine, discoloration of feces, etc.), the abdomen enlarges. Sometimes hepatic encephalopathy develops; when the brain is damaged, its activity is disrupted, and hallucinations may occur.
Signs of chronic hepatitis do not appear immediately in patients; the first stages of the disease can be asymptomatic, which makes it especially dangerous. Chronic hepatitis is often detected during examination in connection with other diseases.
Diagnosis of hepatitis
Manifestations of hepatitis vary and depend directly on the cause of liver damage. There are cases when hepatitis does not have specific symptoms or is completely asymptomatic. Only a detailed survey and thorough examination of the patient allows a specialist to establish hepatitis in such cases. But in order for the diagnosis to be confirmed as final, additional research may be needed.
Laboratory diagnosis of hepatitis includes the following tests:
- Clinical blood test;
- Gamma-GT;
- Coagulogram;
- Direct and total bilirubin;
- AST;
- ALT;
- alkaline phosphatase;
- Albumin (code 79) and total protein in serum;
- Transferrin (code 28);
- Copper in the blood;
- Ceruloplasmin (code 110);
- Ferritin (code 30);
- Total cholesterol;
- HBsAg (code 833 or code 839);
- Anti-HCV, antibodies, ELISA;
- Cytological examination of punctates, as well as scrapings of other tissues and organs;
- A screening study to detect the presence of psychotropic, narcotic and potent substances.
Additional tests to diagnose hepatitis include an abdominal ultrasound.
Immunoprophylaxis
Immunoprophylaxis may include active immunization using vaccines and passive immunization.
Routine vaccination against hepatitis A and B is recommended for all children and adults.
Immunoglobulins prevent or reduce the severity of hepatitis A virus infection and should be given to family members and people in close contact with people who are sick. Hepatitis B immunoglobulins probably do not prevent infection, but they do prevent or relieve clinical symptoms.
There are no immunoprophylaxis methods for hepatitis C virus or hepatitis D virus. However, prophylaxis against hepatitis B virus infection prevents infection with hepatitis D virus. Modification of the hepatitis C virus's own genome prevents the development of a vaccine.
Hepatitis treatment
To treat acute hepatitis, it is first necessary to stop the impact of the pathological factor on the liver, to avoid the disease becoming chronic. Most acute hepatitis can be cured completely.
Depending on the cause of its occurrence and the activity of the process, chronic hepatitis lasts from six months to several years. Its long course requires regular visits to a specialist for examinations, strict adherence to medical recommendations, as well as changes in the patient’s lifestyle. This is necessary to prevent liver failure, cancer and cirrhosis of the liver.
Chronic persistent hepatitis
The most benign form. There may be complaints of minor aching pain or heaviness in the right hypochondrium, intermittent general weakness, and fatigue. Often patients do not feel their illness, there are no complaints at all. The liver is slightly enlarged, slightly painful, the spleen is rarely enlarged, there is no jaundice. treatment of chronic hepatitis Changes in biochemical blood tests - increased transaminases, thymol test only during an exacerbation. The course is perennial and does not progress. With a rational lifestyle (diet, alcohol prohibition), recovery is possible.
Treatment. Meals should be 4 times a day with the complete exclusion of mushrooms, canned, smoked and dried foods, fried foods, chocolate products, cream and pastries, alcohol, and limit the consumption of animal fats (fatty meats, duck, goose, pork). 1-2 times a year courses of vitamin therapy (group B, ascorbic acid, rutin). Taking choleretic drugs is not recommended. Once every 6-12 months, the patient undergoes a blood test for liver tests.