Key Facts
- Hepatitis B is a viral infectious disease that affects the liver and occurs in acute or chronic form.
- Transmission of the virus most often occurs perinatally from mother to child, as well as through contact with blood or other biological fluids, in particular during sexual contact with an infected partner, unsafe injection practices, cuts with piercing instruments in medical practice and in domestic conditions, and also among people who inject drugs.
- WHO estimates that in 2022, there will be 296 million people worldwide living with chronic hepatitis B (i.e. positive for hepatitis B surface antigen).
- An estimated 820,000 people died from hepatitis B in 2022, primarily as a result of hepatitis-related liver cirrhosis and hepatocellular carcinoma (primary liver cancer).
- As of 2022, 30.4 million (10)% of all people living with hepatitis B were aware of their infection, and 6.6 million (22%) of all diagnosed patients were receiving treatment. According to the latest WHO estimates, in 2022 the proportion of children under five years of age with chronic hepatitis B has fallen to just under 1%, compared with the decades before the introduction of vaccination (i.e. from the 1980s to the early 2000s). x years) this figure was about 5%.
- According to WHO estimates, in 2022, despite the availability of a highly effective vaccine, the number of people primarily infected with hepatitis B was about 1.5 million people.
- Hepatitis B is preventable through safe, accessible and effective vaccines.
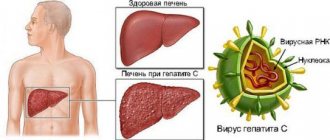
Hepatitis B is a potentially life-threatening infectious liver disease caused by the hepatitis B virus (HBV). This disease is a major health problem worldwide. The infection can become chronic with a high risk of death from cirrhosis and liver cancer.
There is a safe and effective vaccine that provides 98–100% protection against hepatitis B. Prevention of viral hepatitis B helps prevent the development of complications such as chronic hepatitis and liver cancer.
Mechanisms of transmission
In highly endemic areas, hepatitis B is most often transmitted either from mother to child during childbirth (perinatal transmission) or through horizontal transmission (contact with infected blood), especially between infected and uninfected children in the first five years of life. Infants who are infected from their mother, or children who become infected under 5 years of age, very often develop chronic infection.
Hepatitis B is also transmitted through needle sticks, tattoos, body piercings, and contact with infected blood and body fluids, including saliva, menstrual and vaginal fluids, and semen. Infection can also occur through the reuse of contaminated needles and syringes or sharps in medical institutions or in domestic settings, as well as among people who inject drugs. Infection can be transmitted through medical, surgical and dental procedures, tattooing, and the use of razor blades and similar devices contaminated with infected blood. In addition, the hepatitis B virus can be transmitted through sexual contact, especially among unvaccinated individuals who have multiple sexual partners.
Chronic hepatitis B develops in less than 5% of people infected as adults, and in about 95% of those infected during infancy and early childhood. The hepatitis B virus can survive outside the human body for at least seven days. During this period of time, the virus retains the ability to cause infection if it enters the body of an unvaccinated person. The duration of the incubation period for hepatitis B ranges from 30 to 180 days and averages 75 days. The virus is detected in the blood within 30–60 days after infection and can persist in the body, causing chronic hepatitis B, especially if infected during infancy or childhood.
Security measures
It is almost impossible to completely protect yourself from the risk of hepatitis C infection. However, effective preventive measures help maintain health:
- Avoid visiting dental offices, beauty salons and medical clinics with a dubious reputation. Make sure that the establishment uses either disposable or sterilized instruments in your presence;
- Those who received a blood transfusion or organ transplant before 1991 should be tested for HCV;
- Use condoms when having contact with casual sexual partners;
- Use only personal hygiene items;
- Do not use reusable syringes under any circumstances.
Those who come into contact with infected people due to professional duties must wear disposable gloves and take care of the integrity of the skin. Such simple measures help prevent the virus from entering the blood.
Symptoms
In most cases, the primary infection is asymptomatic. However, some patients experience acute symptoms with severe symptoms that persist for several weeks and include icteric discoloration of the skin and sclera, dark urine, severe weakness, nausea, vomiting and abdominal pain. In rare cases, acute hepatitis can lead to acute liver failure with a risk of death.
In some people, the hepatitis B virus can also cause a chronic liver infection, which over time can develop into cirrhosis (scarring of the liver) or liver cancer.
How not to get infected
The virus is not transmitted through breast milk
There is a 90% chance that you cannot become infected through.
- Feces, urine.
- Mother's milk.
- Sperm.
- Household items, if there are no particles of blood or saliva on them, or enough time has passed for the virus to die.
Important! There is a 1% chance of becoming infected with hepatitis C through contact with microparticles of blood and saliva during the life of the virus outside the human body. Minimum 48 hours.
Who is at risk for chronic hepatitis B?
The likelihood of developing a chronic infection depends on the age at which a person became infected with the hepatitis virus. Chronic infection is most likely to develop in children infected with the hepatitis B virus before the age of six.
Infants and young children:
- in infants infected in the first year of life, chronic infection develops in 80–90% of cases;
- Children infected before the age of six develop chronic infection in 30–50% of cases.
Adults:
- in people infected with hepatitis B as adults, in the absence of other concomitant diseases, chronic infection develops in less than 5% of cases;
- if chronic infection develops in 20–30% of adults, the disease leads to cirrhosis and/or liver cancer.
Can you get infected through sexual contact?
There is a 50% chance of transmitting the virus.
- Acidity imbalance in the vagina.
- Unsanitary conditions and other conditions of the body that led to the appearance of microcracks in the anus and vagina.
- Frequent use of contraceptives, condoms with lubricants, flavorings – wounds – bleeding – acidity disorders – suppuration; 90% chance of developing cirrhosis.
Important! To date, no virus has been detected in semen. But until recently, it was not detected in saliva.
Diagnostics
Based on the clinical picture alone, it is impossible to differentiate between hepatitis B and other types of viral hepatitis; Therefore, laboratory confirmation of the diagnosis is extremely important. Several laboratory blood testing methods are available to diagnose and monitor patients with hepatitis B. They can be used for differential diagnosis of acute and chronic infections.
Methods for laboratory diagnosis of infection include detection of hepatitis B surface antigen (HbsAg). To ensure blood safety and prevent accidental transmission of the virus to recipients of blood products, WHO recommends systematic testing of donated blood for hepatitis B.
- Acute HBV infection is characterized by the presence of hepatitis B virus surface antigen (HBsAg) and antibodies to core antigen (HBcAg) - class M immunoglobulins (IgM). During the initial phase of infection, patients also develop hepatitis B virus e antigen (HbeAg). HBeAg is usually a marker of high levels of viral replication. The presence of HBeAg indicates the highly contagious nature of the blood and biological fluids of the infected person.
- Chronic infection is characterized by the persistence of HBsAg for at least six months (with or without the simultaneous presence of HBeAg). The persistent presence of HBsAg is a major marker of the lifetime risk of developing chronic liver disease and liver cancer (hepatocellular carcinoma).
Where can you get infected?
Due to the specific nature of virus transmission, there are a number of establishments with an increased risk of infection.
- Cheap and mid-price catering establishments - blood is less likely to be saliva; infection through microcracks or wounds in conflict situations.
- Public toilets, showers - particles of blood, saliva, sweat from the wearer - microcracks, damaged nasopharyngeal mucosa, recipient's eye mucosa.
- Hairdressers, dental offices.
- Cosmetology salons.
- Production workshops – use of sharp objects.
- Medical institutions where preventive measures for the virus are neglected.
Treatment
There is no specific treatment for acute hepatitis B. Therefore, medical care focuses on maintaining physical comfort and proper nutritional balance, including replacing fluid losses caused by vomiting and diarrhea. It is very important to avoid unnecessary drug treatment. Acetaminophen/paracetamol and antiemetics should not be prescribed to patients with hepatitis A.
For chronic hepatitis B, drug treatment may be prescribed, including oral antiviral drugs. Treatment can slow down the development of liver cirrhosis, reduce the risk of developing liver cancer and increase long-term survival rates for patients. WHO estimates that in 2022, 12 to 25% of people with chronic hepatitis B will need drug treatment (depending on setting and eligibility criteria).
WHO recommends prescribing the oral drugs tenofovir and entecavir, which are the most effective drugs for suppressing the replication of the hepatitis B virus. Their use less often leads to the formation of drug resistance, is simple (1 tablet per day) and is not accompanied by significant side effects, and therefore there is no the need for careful monitoring of patients.
Entecavir is not a branded drug. In 2017, all low- and middle-income countries were able to legally purchase generic entecavir, although costs and availability varied widely. Tenofovir is no longer protected by patent in any country in the world. In 2016, the international median price of WHO prequalified generic tenofovir decreased from US$208 to US$32.
For most patients, drug treatment effectively suppresses viral replication but does not completely cure hepatitis B. Therefore, most patients who start treatment for hepatitis B must continue it for life.
In many resource-poor areas, access to hepatitis B diagnosis and treatment remains difficult. In 2022, of the more than 296 million people living with HBV, only 10% (30.4 million) were aware of their diagnosis. Only 22% (6.6 million) of diagnosed patients were treated. Many patients are diagnosed in the later stages of liver disease.
Among the chronic complications of hepatitis B, high rates of morbidity and mortality are associated with advanced liver diseases such as cirrhosis and hepatocellular carcinoma. Liver cancer progresses rapidly and, given the limited treatment options, the outcome is usually poor. In low-income countries, most patients with liver cancer die within a few months of diagnosis. In high-income countries, the lives of such patients can be extended by several years through surgery and chemotherapy. Also in high-income countries, some patients with cirrhosis or liver cancer receive liver transplantation, but success rates for such treatment are variable.
Diet and proper nutrition
In the acute period, bed rest and strict dietary nutrition are indicated. The diet for hepatitis B in the acute period is aimed at maximally sparing the organ with adequate nutrition. The acute process requires adherence to Diet No. 5A, in which food is prepared only grated or well-cooked. Soups can be made with finely chopped vegetables. Some dishes are prepared baked, but without a distinct crust. Diet: 5 times a day.
In case of chronic hepatitis B, adherence to diet No. 5 is not necessary, but when drawing up a menu it is worth keeping a guide to it. Experts say that in the chronic stage it is important to adhere to a healthy diet. Proper healthy eating involves consuming enough proteins, fats, carbohydrates and beneficial microelements
What should you not eat?
It is prohibited to use:
- fresh and rye bread;
- products made from butter or puff pastry;
- millet and all legumes;
- broths;
- fatty meats, fried meats, sausages, smoked meats;
- offal and canned food;
- cream and fat cottage cheese;
- mushrooms, legumes, pickled vegetables, turnips, radishes, cabbage, sorrel, garlic, onions;
- fruits that are sour and rich in fiber;
- cocoa, coffee, chocolate, carbonated drinks.
Allowed foods
Dishes and food allowed for consumption in acute and chronic forms of hepatitis B:
- yesterday's bread;
- unleavened pastries with various fillings;
- biscuits, marshmallows;
- soups cooked in water, milk, low-fat broth;
- chicken ham and sausages;
- from meat - chicken, veal, rabbit;
- from fish - pollock, hake, blue whiting;
- steamed and baked omelettes;
- steamed meatballs and cutlets;
- milk, low-fat fermented milk products;
- all types of cereal porridges;
- vermicelli and pasta;
- vegetable salads seasoned with sunflower oil or low-fat sour cream;
- vegetable fats;
- Bee Honey;
- fruits and vegetables in baked, boiled, raw form;
- non-acidic vegetable, berry and fruit juices;
- green tea.
With hepatitis, the processes of bile formation are disrupted, which leads to impaired absorption of vitamin K in the gastrointestinal tract and its deficiency. Foods containing vitamin K:
- parsley,
- watercress,
- basil,
- cilantro,
- cabbage (broccoli, Chinese cabbage, white cabbage),
- celery root,
- prunes,
- avocado,
- cashews, pine nuts.
Prevention
The main method of preventing hepatitis B is vaccination. WHO recommends that all newborns be vaccinated against hepatitis B as soon as possible after birth, within the first 24 hours of life if possible, followed by two or three doses of the vaccine at least four weeks apart to ensure full vaccination. Timely vaccination of children immediately after birth is an effective way to reduce the incidence of mother-to-child transmission of hepatitis B.
According to the latest WHO estimates, the proportion of children under five years of age with chronic hepatitis B worldwide has fallen to just under 1% in 2022, compared with the decades before the introduction of vaccination (i.e. from the 1980s to early 2000s) this figure was about 5%.
This has achieved one of the Sustainable Development Goal targets for viral hepatitis elimination: reducing the prevalence of HBV infection among children under five years of age to less than 1% by 2022. This success was achieved in a number of regions with the exception of sub-Saharan Africa.
Increasing hepatitis B vaccination coverage worldwide over the past two decades has been a major public health achievement and has contributed to a decline in the incidence of hepatitis B infection among children.
In 2022, three-dose vaccine coverage reached 85% worldwide, up from around 30% in 2000. However, rates of newborn immunization against hepatitis B remain variable. Thus, the average rate of vaccination coverage with the first dose of hepatitis B vaccine immediately after birth is 43% worldwide, but in the WHO African Region it is only 6%.
A full course of vaccination produces protective antibodies in more than 95% of infants, children and young adults. Immunity acquired through vaccination lasts for at least 20 years and probably throughout life. Therefore, WHO does not recommend booster vaccinations for people who have completed the three-dose vaccine.
In countries with low or moderate endemicity of hepatitis B, vaccination is indicated for all unvaccinated children and adolescents under 18 years of age. In these countries, high-risk groups are more likely to become infected and should also be vaccinated. These risk groups include:
- individuals who frequently require blood or blood products, dialysis patients, and solid organ transplant recipients;
- prisoners in places of deprivation of liberty;
- injection drug users;
- persons who have household and sexual contact with people with chronic HBV infection;
- persons with multiple sexual partners;
- healthcare workers and other persons who may have contact with blood and blood products while on duty;
- International travelers who have not completed a full course of HBV vaccination and who are eligible for vaccination before departure to HBV-endemic areas.
The vaccine has an excellent safety and efficacy record and has reduced the proportion of children under five years of age with chronic HBV infection to just under 1% in 2022, compared with the decades before the introduction of the vaccine (i.e. since the 1980s). until the early 2000s), this figure was about 5%.
In addition to infant vaccination, which includes a timely first dose immediately after birth, WHO recommends prophylactic antiviral therapy to prevent mother-to-child transmission of hepatitis B. Pregnant women with a high concentration of HBV DNA (high viral load) and/or the presence of HBeAG in the blood are at high risk of transmitting the virus to their unborn child, even if the child receives the first dose of vaccine immediately after birth and completes the full course of vaccination against hepatitis B. Therefore, pregnant women with high The concentration of HBV DNA during pregnancy may indicate a prophylactic course of antiviral therapy to prevent perinatal HBV infection and protect the unborn newborn from the disease.
In addition to infant vaccination and prevention of mother-to-child transmission, HBV transmission can be prevented through blood safety measures, including quality screening of all donated blood and blood products used for transfusion. Globally, 97% of donated blood units were screened and quality controlled in 2013, but gaps remain. Effective measures to prevent the transmission of hepatitis B virus include ensuring safe injections and avoiding unnecessary injections and injections performed in unsafe conditions. Between 2000 and 2010, the rate of unsafe injections worldwide fell from 39% to 5%. In addition, one of the effective measures to prevent infection is to improve the safety of sexual intercourse, including minimizing the number of sexual partners and the use of barrier contraception (condoms).