We are waiting for the birth to begin
Are you expecting a baby? Congratulations! One of the most important events in life is already close, and many mothers worry in vain, expecting severe pain or worrying about the process itself. Your body is specially created for childbirth and is completely ready for it. And experienced doctors will take care of you, their knowledge, skills and attention will help the baby be born.
But I still wonder on what day there will be one more person on our planet. How to calculate the due date? The approximate date of the expected birth is known to every expectant mother from the very beginning, from the moment the doctor calculates it. But you need to know that childbirth can occur from the full 37th to the end of the 42nd week, that is, on average, pregnancy lasts from 260 to 293 days, so for sure “that very” day cannot be known to anyone, except perhaps the baby himself.
How do you know when labor is approaching? You can identify indirect signs, but remember that everything is individual.
- Abdominal prolapse. For those expecting their first child, the belly drops 2 to 4 weeks before giving birth; for mothers who are not giving birth for the first time - the day before. This happens because the baby feels ready to be born and changes position in the abdomen, occupying the presenting part (that is, the one that is now located at the bottom of the uterus) in the pelvis. At the same time, the navel protrudes.
- Heartburn goes away. Thanks to this, the feeling of pressure on the diaphragm goes away, breathing becomes easier, and the symptoms of heartburn and belching go away.
- Increased urge and change in stool. At the same time, the urge to go to the toilet becomes more frequent, and about a week before birth, the stool becomes liquid - due to the pressure of the fetus on the rectum and the effect of activated hormones on the intestines.
- Pain in the lower back. There may be nagging, painful, sometimes cramp-like sensations in the perineum and pelvis due to pressure and stretching of the tissues of the sacrum. During this period, the expectant mother may find it uncomfortable to walk and sit, and it may be difficult to find a comfortable position during sleep. “False” contractions may be felt, but if they are irregular and the interval between them does not decrease, then it is too early to talk about the onset of labor.
- Lack of appetite. Most often, before giving birth, expectant mothers do not even want their favorite food. As a rule, 1–2 weeks before the birth of a child, pregnant women lose up to 2 kg due to excess fluid. This is how the body prepares for childbirth, when the mother will need additional flexibility and lightness.
- Changeable mood. More and more hormones are released, and the pregnant woman’s mood changes hour by hour. The periods when the expectant mother is active and cheerful are replaced by a desire to retire and be in silence.
- The baby moves less. His new position—usually head down—makes him uncomfortable to move.
- Mucous discharge. During pregnancy, the cervix is closed by a mucus plug, and shortly before the baby is born, it comes off. This can happen right before childbirth, at the beginning of labor, and 1 - 2 weeks before it. It is thick, transparent, slightly yellowish, often mixed with blood. This is normal, however, if the discharge is bloody, you need to go to the doctor as soon as possible to make sure that there are no complications, or to deal with them quickly.
Not everyone knows that water can leak or break before birth.
Some unpleasant sensations can cause discomfort and ruin your mood, but try to concentrate on the joyful anticipation: all these are temporary phenomena, and besides, very soon you will meet your baby for the first time!
The stomach "sinks"
About 2 to 3 weeks before giving birth, a woman who is giving birth for the first time may notice that her stomach has moved downward. In a woman giving birth again, the stomach usually drops immediately before childbirth. Moreover, as a rule, the lowering of the abdomen is very noticeable: if previously it began right under the chest, now you can place your palm between it and the beginning of the abdomen. Many people also notice the lowering visually. Most women have a protruding belly button. “Descent” of the abdomen occurs due to the lowering and insertion of the presenting part of the fetus (usually the head) into the pelvic inlet, as well as stretching of the lower segment of the uterus and deviation of the uterine fundus (its upper part) anteriorly due to a slight decrease in abdominal tone. This is how the child finds a comfortable position for entering the small pelvis and settles into it. The baby's head is placed approximately in the middle of the expectant mother's small pelvis. In the second and subsequent pregnancies, the head is initially low, so no noticeable prolapse occurs. In some cases (and this is within normal limits), the baby may “wander” or be relatively high in the pelvis until the very moment of birth, and the “dropping” of the abdomen does not occur at all.
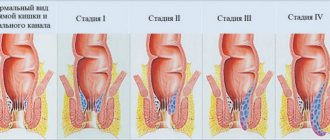
What are the stages of the birth process?
First stage of labor. The onset of labor occurs as soon as regular contractions begin, with less and less time between them. Many expectant mothers notice the appearance of irregular “false” contractions after the 30th week of pregnancy. If you are worried about this, it is enough to visit a doctor to make sure that they are false. In any case, remember that only the regularity of contractions indicates the onset of labor.
At the initial stage, the cervix gradually opens; at the end it should be opened by 10 - 12 cm.
The initial stage consists of two phases:
- Latent phase - first, the cervix opens by 2 - 3 cm at a speed of 0.35 - 0.5 cm per hour;
- Active phase - the speed of cervical dilatation increases to 1 - 2 cm per hour, but at the end, when the cervix is almost completely dilated, it drops slightly: the body is preparing for the second stage of labor.
On average, disclosure takes 9 – 12 hours.
The second stage of labor is contractions from the moment the uterus opens until the baby is born.
The third stage of labor is the time between the birth of the baby and the birth of the “afterbirth” - the placenta and membranes.
Both pregnancy and childbirth always proceed individually. On average, the birth process takes from 10 to 20 hours. But some women give birth much longer, while others, on the contrary, faster. For expectant mothers who give birth vaginally for the first time, labor is thought to take longer.
Do precursors always indicate the onset of labor?
What is meant by the onset of labor? This is the development of regular contractions. Contractions in 15-20 minutes for 20 seconds. The intensity and duration of contractions increases, and the intervals between contractions decrease. The development of regular labor leads to the opening of the uterine pharynx.
Harbingers of labor only indicate the imminent onset of regular labor. Training contractions, which can begin several weeks before birth, are of a completely different nature (see above). And they are aimed at preparing, a kind of familiarization, with how the uterus needs to work during childbirth. They do not lead to the opening of the uterine pharynx, and, accordingly, to childbirth.
How labor begins
Childbirth begins with contractions: regular contractions of the uterus lead to the dilatation of the cervix and the birth of the baby. The sensations can be described as follows: the stomach seems to turn to stone, shrinking into a lump, and after a few seconds it relaxes.
The very first contractions can be missed without noticing them: most often they are almost not felt; then they become stronger, and at the moment when they occur, nagging pain appears in the lower abdomen or lower back. Afterwards, these sensations go away until another contraction occurs.
As a rule, early contractions are not too painful, but it can be different. In this case, tell your doctor about your discomfort so that he can help you cope with it.
How long do contractions last?
The interval between contractions at the beginning of labor is 10–12 minutes (sometimes 5–6), and they last for several seconds. Gradually they begin to appear every 3 - 5 minutes, their duration also increases to 40 - 60 seconds.
Typically, this period lasts from 6 to 12 hours. Sometimes prenatal contractions last a long time, more than a day, and the expectant mother may get tired of them, which is not very conducive to a normal birth. In this case, you need to consult a doctor who, if necessary, will help in this situation.
When does your water break?
Labor may begin with the rupture of amniotic fluid. They can immediately go away completely, or pour out in small portions. In any case, after this you need to see a doctor so that, after assessing your condition, he can decide whether you are ready for childbirth or whether you need to wait a little longer. Most often, the water is colorless, with small white flakes - this is the lubricant of the fruit. If they are green or yellow, you should consult a doctor.
As a rule, water is poured out in large quantities (about 250 - 300 ml) or - in another case - constantly, from the moment the process begins, and it is difficult not to notice.
It is impossible to confuse water with discharge, which also becomes more noticeable and watery towards the end of pregnancy: discharge may appear in the morning, and then disappear during the day, unlike water, which flows constantly. If in doubt, do not hesitate to consult your doctor.
When to go to the maternity hospital?
This is a question that worries many expectant mothers. The general recommendation is to go there when not only contractions have become regular, but the intervals between them are 7–8 minutes.
Until this time, you can walk around, take a warm bath, or sleep a little between contractions.
But if you wish, you can go to the maternity hospital earlier. The first stage of labor is considered complete when the cervix has dilated to 4–6 cm and continues to dilate. If this “indicator” is less than 3 cm, you may not be admitted to the maternity hospital and sent back home.
How to behave during the onset of labor
Don't nervously count down time with a stopwatch, this will only tire you. It doesn't matter how long the initial labor process lasts. Make sure that the birth lasts as long as necessary. It is enough to pay attention to the duration of contractions and intervals from time to time. As a rule, the contractions themselves will tell you when the labor process has intensified.
- The most important thing for you is to save energy and rest more. Try to sleep between contractions.
- Drink enough fluids and go to the toilet more often, even if you don't really want to: a full bladder prevents the uterus from contracting, and the baby has less room to move around.
- If you are worried, the best thing to do is do relaxation exercises, watch a movie or read a book.
Sources
- Yu Y., Yang X., Wang S., Wang H., Chang R., Tsamlag L., Zhang S., Xu C., Yu X., Cai Y., Lau JTF. Serial multiple mediation of the association between internet gaming disorder and suicidal ideation by insomnia and depression in adolescents in Shanghai, China. // BMC Psychiatry - 2022 - Vol20 - N1 - p.460; PMID:32967648
- Macari S., Milgramm A., Reed J., Shic F., Powell KK., Macris D., Chawarska K. Context-Specific Dyadic Attention Vulnerabilities During the First Year in Infants Later Developing Autism Spectrum Disorder. // J Am Acad Child Adolesc Psychiatry - 2022 - Vol60 - N1 - p.166-175; PMID:32061926
- Hewitt L., Benjamin-Neelon SE., Carson V., Stanley RM., Janssen I., Okely AD. Child care center adherence to infant physical activity and screen time recommendations in Australia, Canada and the United States: An observational study. // Infant Behav Dev - 2018 - Vol50 - NNULL - p.88-97; PMID:29223777
- Daniels LA., Mallan KM., Battistutta D., Nicholson JM., Perry R., Magarey A. Evaluation of an intervention to promote protective infant feeding practices to prevent childhood obesity: outcomes of the NOURISH RCT at 14 months of age and 6 months post the first of two intervention modules. // Int J Obes (Lond) - 2012 - Vol36 - N10 - p.1292-8; PMID:22710926
Active phase of onset of labor
Contractions become stronger, longer and more frequent, making it difficult for you to talk when they occur. The cervix is actively dilating. If contractions become painful and occur every 5 minutes for an hour, you need to go to the hospital without delay. This phase of labor lasts on average 5 – 8 hours. If you are giving birth for the first time or the baby is large, it will take longer, but if you have taken oxytocin or have had a vaginal birth before, the process will be faster and is unlikely to take more than an hour.
What to do at this moment
It's okay to walk during this time, but you'll likely want to lean on something during contractions. If you are tired, you can rest by lying on your left side. You can take a shower, a warm bath, or ask for a light massage.
- When the cervix has dilated to 8–10 cm, the most active part of labor begins. The contractions are getting stronger, coming every 2 - 3 minutes and lasting a minute or longer.
- You may feel shivering and chills between contractions, and feel hot during contractions.
- The baby moves to the pelvic area, if he has not done so before, and there is a feeling of pressure on the rectum and the desire to push.
- Most often, bleeding appears at this moment - don’t worry, this is normal.
- There is often a feeling of nausea.
Before labor begins, many (but not all) doctors ask the woman to give her an enema. This is a voluntary procedure, but expectant mothers often agree because then they won't have to worry about having a bowel movement during labor, although this is completely normal. This means they will be able to feel more comfortable while pushing. It is better to consult your doctor in advance and choose a plan of action that is more suitable for you.
Many women in this phase of labor turn to pain relief, such as an epidural.
However, there are many ways to relax and relieve pain, since much of the pain is caused by fear, and not by a real physical process.
Here are a few tricks:
- Ask for a light massage;
- Look for a more comfortable body position;
- Apply a cool or warm compress to your forehead;
- You may want silence and no need to communicate, since contractions take all your attention; but maybe you will want to get support from a doula - your assistant during childbirth, about whom we will talk in more detail below - as well as from the child’s father or another loved one;
- Focus on the fact that with each contraction you are helping the baby to be born.
Breathing becomes easier
Immediately after the baby begins to descend deeper into the pelvic area and the pressure on the chest, diaphragm and internal organs decreases, the mother experiences relief: it becomes much easier to breathe. Most often, heartburn goes away because the space for the stomach increases and the contents from the stomach do not flow back into the esophagus. However, this increases pressure on the lower abdomen and makes sitting and walking a little more difficult. It is also possible that after the fetus is displaced downwards, the expectant mother will have difficulty sleeping, since at this time it is difficult to find a comfortable position. In addition, numbness in the legs is possible, which is caused by the lowering of the baby's head, which can compress the nerve endings - the numbness can go away when lying on its side.
Epidural anesthesia
If you have an epidural, either for medical reasons or because you want it, you will feel less pressure. This process takes from several minutes to several hours.
- This procedure is widespread and is considered safe; complications occur very rarely, only in 1 case out of 80,000.
- This anesthesia is done in the lumbar region using a special needle and a thin catheter into which medication is injected approximately every 30 minutes.
- As a rule, after this the expectant mother is able to walk, but sometimes her legs may lose sensitivity for a while, and then she will have to lie down.
What are the benefits of anesthesia? Thanks to her, the expectant mother, as a rule, does not feel pain.
The disadvantages are that labor is slower, in 1 in 20 cases the anesthesia does not work, and complications are possible. It is believed that the effect of anesthesia on the baby is minimal if no complications arise.
As a rule, doctors recommend against epidural anesthesia, but each woman's sensitivity threshold is different, and if severe fear and pain increase and you cannot cope with it, your doctor will prescribe this procedure for you.
Pushing, childbirth and placenta
Once the cervix is fully dilated, the baby begins to move through the birth canal. At this point, contractions occur less frequently so that you have time to rest between them. Many mothers believe that this period, despite the fact that it is the main one - right now the baby will be born - is easier to bear. For others, having to push may not be the most pleasant thing to do.
The uterus contracts and the baby feels pressure. With each attempt, he moves along the birth canal. Now you don’t need to do anything special, you just push with each contraction, trying to relax as much as possible during the breaks. However, in many hospitals, doctors ask the expectant mother to push specifically: everything is individual, so you should discuss with the doctor in advance how best to behave and choose the method that is closer to you.
If you have had an epidural anesthesia, you do not feel the contractions of the uterus so clearly, then you should trust your doctor who will tell you when to push.
- The birth of the baby itself can be fast, especially if this is not your first vaginal birth, or slow. With each contraction, the baby will get closer to exiting the birth canal.
- At this moment, a woman often wants to change her position to find the most comfortable one, but the hospital does not always have this opportunity.
- Finally, when the next contraction ends, the baby’s head (as a rule, the baby is born with the head forward, although this is not at all necessary) will gradually appear and will be born very soon.
- Now the expectant mother wants to push even harder, and with each contraction the head is visible more and more clearly, and the muscles of the perineum are stretched and a burning sensation may be felt in this area (between the anus and vagina).
- At this time, your doctor will tell you when to push less or stop so that the baby's head can come out of the vagina. It is important to try to allow the head to pass through slowly and smoothly to avoid tearing the perineum.
- As soon as the head is born, the doctor checks whether the umbilical cord is entangled in the baby’s neck. If this happens, they will try to remove the umbilical cord from the neck or cut it if necessary.
- Then the doctor will tell you when to push so that the baby moves smoothly out of the birth canal.
As soon as the baby is born, he will be dried with a towel and excess mucus will be removed from the mouth and nose. If possible, the doctor will place your son or daughter on your chest so that you can admire your treasure. They will cover you with a blanket: now the newborn needs warmth.
The doctor will cut the umbilical cord, and you will be overwhelmed with emotions and great relief that labor is over. And although you will be very tired, you may not even want to sleep at this moment.
How long does the second stage of labor last? From several minutes to several hours. Without an epidural, this stage usually takes about an hour for a woman giving birth for the first time, and about 20 minutes if this is not her first labor.
There is very little left. Just a few minutes after the baby is born, contractions begin again. The first few contractions separate the placenta from the walls of the uterus. The doctor will tell you when to push. As a rule, the placenta is born after one contraction, it is not painful and takes 5 – 10 minutes.
The birth is over - what next?
Congratulations to mom and her baby! After the placenta has left the uterus, you will feel that your stomach has become hard: this is the uterus contracting. The doctor will check to make sure she remains in this position. This is important so that the blood vessels that connect the placenta and uterus can narrow and the bleeding stops.
- The doctor will check to see if all of the placenta has been delivered and will do an exam to make sure there are no stitches needed in the perineum. If necessary, you will be given local anesthesia. If you had an epidural, the anesthesiologist will come to you to remove the catheter from your back. It takes one second and doesn't hurt at all.
- If you are planning to breastfeed, now is the time to make your first try. True, both you and your baby should be prepared for this. Not all newborns have this desire in the first minutes after birth, but try holding the baby at the nipple. Most babies begin to breastfeed within the first hour after birth. Breastfeeding early helps your newborn, and it's good for mom, too: Breastfeeding releases oxytocin, the same hormone that causes contractions and now helps your uterus stay in a contracted position. If this does not happen, the doctor will give you oxytocin and everything will work out in any case.
- At this time, contractions continue, but almost imperceptibly. If this is your first baby, you may only feel a few contractions. If you already have children, then contractions may continue from time to time for 1 to 2 days. They feel like menstrual pain, and if it is too severe, ask your doctor for a safe pain reliever. You may feel weak or chilly - this is completely normal and will pass soon.
If the birth went without problems and the baby does not need special care, ask the doctor to leave you with the child, now is your time!
Episiotomy: when and why it is done
This is the name given to a small incision in the perineum and back wall of the vagina so that the baby's head can be born. This is a fairly common procedure, and the doctor cannot tell before delivery whether it will be needed. We list the cases when the doctor may decide that it needs to be done:
- If there are signs that the perineal ligaments are not elastic enough and there is a risk of rupture. Then a 2-3 cm incision is the lesser of evils, because the gap may be longer and heal less quickly.
- If there is a fear that the baby's head may be injured. This may happen if the baby’s head is much larger than the opening of the vagina or if the baby moves his pelvis forward during childbirth.
- If childbirth occurs quickly.
- If swelling of the perineum is noticeable, this happens when contractions are not strong enough or if they last much longer than expected.
- When a woman is unable to wait out the attempts and the tissues are forced to expand too quickly.
- If a woman’s condition requires a faster birth of the baby (for example, high blood pressure, severe myopia or other factors).
- When the doctor needs to apply special instruments to help the baby be born: these can be obstetric forceps or a vacuum extractor. An experienced specialist will be able to assess whether this is really necessary, whether it is safe for the child and which method is correct.
The perineal muscles may not be flexible enough in the following cases:
- If this is the first birth of a woman over 35 years old;
- If the perineum is located high, that is, the distance between the anus and the vagina is more than 7 - 8 cm;
- If there are scars on the perineum;
- When the obstetrician did not sufficiently protect the perineum when removing the baby's head and shoulders.
How is an episiotomy done?
Anesthesia is not usually used for this procedure, but the woman does not feel pain because there is currently insufficient blood supply and sensitivity in these tissues.
The incision is most often made when the head is exposed; do it with scissors.
After your baby is born, your doctor will stitch you with anesthesia using surgical suture, which dissolves on its own so there is no need to remove stitches.
The suture usually heals within 4 to 5 weeks if you follow the doctor’s recommendations (bed rest, breastfeeding while lying down, a light diet) and take care of the suture. After the lochia (discharge after childbirth) has stopped and the stitch has healed, if you are ready, you can engage in sports and sex. There may be some discomfort at first, but it will go away over time.
What you can do to reduce the risk of an episiotomy:
- You should massage the perineum 2 - 3 times a week, starting from about the 36th week of pregnancy - preferably using special oil. The technique is simple: you need to insert your fingers shallowly into the vagina and press towards the anus.
- Kegel exercises are also useful - contraction of the intimate muscles and muscles of the anus at different rates. Read about them in a special material (https://agulife.ru/calendopedia/kak-vosstanovitsya-posle-rodov).
- Try to be as calm and patient as possible during childbirth.
When is a caesarean section performed?
Statistics from recent decades show that caesarean sections are being performed more and more often all over the world. According to WHO, this operation for medical reasons should be prescribed no more than 15% of cases. But in reality this number is much higher (in a number of European countries - almost half of all births).
A caesarean section is a medical operation in which childbirth occurs surgically through an incision in the uterus. This method has been known since the times of Ancient Rome. But the conditions under which the operation is carried out have, of course, changed markedly since then. Everything goes quite quickly and, as a rule, only takes an hour. It is the latter fact that is often decisive when women opt for a cesarean section “at will”: some are afraid of hours of contractions, others are afraid of ruptures and stretching of the uterus, etc.
However, a caesarean section is not a cosmetic procedure. For medical reasons, it is prescribed only if there is a threat to the life and health of the mother or baby. Compared to natural childbirth, the risks for both the woman and the baby in the case of a cesarean section are many times higher.
When is a caesarean section performed electively, as prescribed by a doctor?
- The woman’s pelvis is too narrow and/or the fetus is too large;
- Placenta previa (the placenta covers the entrance to the uterus);
- Scars on the uterus from previous operations, threat of rupture;
- Multiple pregnancy;
- A number of diseases not related to pregnancy (cardiovascular diseases, risk of retinal detachment, varicose veins, viral diseases of the urinary tract, etc.).
When is a caesarean section performed urgently after contractions have started?
- When labor takes too long or labor activity suddenly stops;
- In case of acute oxygen deficiency and problems with the child’s heartbeat;
- With premature placental abruption;
- If there is a risk of uterine rupture.
What should you know if you are scheduled for a caesarean section?
- The doctor monitoring your pregnancy will most likely report the need for surgery during the first examinations. Especially if you already have a history of uterine surgery or have chronic diseases.
- The operation itself is most often scheduled for the end of the third trimester of pregnancy—at 38–39 weeks. Most caesarean sections are performed under local anesthesia (epidural or spinal anesthesia). This way, you will most likely have the opportunity to put your baby to your breast immediately after birth.
- The work of surgeons is hidden from the woman in labor using a small curtain. And only after the doctor removes the baby through an incision in the uterus (in most cases horizontal), you will be able to see your baby.
What should you consider if you are considering having a caesarean section without a compelling medical reason?
- The likelihood of complications developing in both mother and baby is much higher. You will have a longer recovery after childbirth: while the stitch is healing, your mother will need constant help.
- There may be difficulties establishing breastfeeding.
- Negative effects of anesthesia and antibiotics received during surgery for the baby.
- Difficulty regaining fertility: Research shows that a cesarean section may make it more difficult for you to become pregnant again.
If you are having a caesarean section for medical reasons, remember that this is a vital necessity for your baby, and you are doing everything right. If you are choosing surgery out of uncertainty and fear, you may want to reconsider the situation.
Many expectant mothers periodically experience anxiety. Once you cope with it, you will probably believe in the strength of your own body. After all, if natural childbirth is available to you, you should definitely take advantage of this chance.
How a doula is useful
We have already talked about how a doula can help you cope with emotions during childbirth. This is the name of an assistant who prepares a woman for the birth of a child (sometimes even before conception), accompanies her during childbirth and helps to establish contact with the baby immediately after his birth. Being a doula is a job that requires first of all a calling, and then special training and preparation. Doula schools in different countries are united into a community: they share knowledge, hold meetings and conferences, celebrate International Doula Day and train “newbies.”
And although this profession has existed as long as humanity itself, the current doula movement arose in response to the needs of modern urban women. After all, unfortunately, the process of childbirth in urban conditions is depersonalized.
A doula may not have a medical education (having her own children is also not necessary), since she does not interfere in the birth process itself and does not bring her own experience into the woman’s personal process.
How a doula can help you
- Provide information support. A woman knows at any moment what is happening to her, what stage of the process she is at, what is next, how to prepare for it.
- Support emotionally. During childbirth, it’s easy to get scared and wilt, but the assistant “pours” strength and enthusiasm into the woman giving birth, shares her emotions with her and shares her confidence.
- Ensure that the woman's wishes are respected. If a woman was preparing for a specific birth plan and wanted, for example, to do without stimulation and pain relief, these intentions can be easily forgotten under the pressure of specialists in the clinic. At this moment, the doula can “share” her persistence with the expectant mother and act as her representative in negotiations with doctors, so that they treat the wishes of the woman in labor with greater respect. If a mother wants the baby to be placed on her stomach, to wait until the umbilical cord pulsates, to allow her to put the baby to her breast and stay with him as long as necessary, a doula will come to the rescue. At this moment, the mother may not have enough of her own strength to insist on her own, and the doula reminds her and the doctors that there is no need to rush.
- Take care of the woman. Each doula has her own repertoire of ways to relieve labor pain and cope with contractions and pushing. Some use massage, some use aromatherapy, some “sing” the contractions along with the woman. In addition, there are many movement and breathing techniques that make childbirth somewhat easier. Doulas help women manage labor pain naturally, infusing the process with joy, anticipation, curiosity, and confidence.
Doulas are not doctors, and they do not assist in childbirth themselves. But any of them has the appropriate equipment and is ready to step in if for some reason the doctors don’t have time.
Increased frequency of urination and defecation
The urge to urinate becomes more frequent as pressure on the bladder increases. Under the influence of biologically active substances produced in her body towards the end of pregnancy, a woman's intestines cause some stool liquefaction and acceleration of peristalsis, which leads to diarrhea and mild abdominal cramps. This condition is comparable to “bear sickness,” which is well known to many students and occurs before an exam. It is believed that the appearance of frequent soft stools is no coincidence: this leads to cleansing of the mother’s intestines, and at the same time frees up space in the pelvis to facilitate the passage of the child. Sometimes this process is so pronounced that it causes serious panic, as women mistake it for food poisoning. So, if there were no significant reasons for digestive disorders, then you can confidently perceive such a disorder as a harbinger of childbirth.