Removing the stomach is not a death sentence
Stomach cancer ranks fifth in the world in terms of the number of diagnosed cases of cancer, and second in the structure of mortality from tumors. The most effective treatment method is complete or partial removal of the organ. The operation is complex and requires careful preparation and adherence to the rules of a long rehabilitation period. People who follow all doctors' recommendations have a great chance of living a long, fulfilling life.
Proper preparation
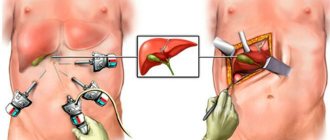
Laparoscopic surgery for stomach cancer in Moscow at the Yusupov Hospital is performed after a preliminary examination of the patient for possible contraindications to surgery.
Preparation includes:
- conclusion of the attending physician;
- medical history indicating the results of previous diagnosis and treatment;
- electrocardiography;
- gastroscopy;
- Ultrasound;
- CT scan;
- blood test (coagulogram, clinical, biochemical, etc.);
- X-ray;
- conclusions of an anesthesiologist.
Before the operation, a consultation is held with an oncologist surgeon. Your doctor may recommend stopping certain medications. The patient will definitely need to stop taking medications that affect blood clotting.
Surgical treatment of cancer
The main method of treatment for gastric tumors is their resection. In the initial stages of organ cancer, endoscopic intervention is possible, in which only the area of the mucous membrane affected by the altered cells is removed. The method is minimally invasive. After removal of the stomach in this way, life quickly returns to normal. However, there are often no indications for endoscopic intervention.
The diagnosis of stomach cancer is extremely rarely confirmed in the early stages of the disease; most people undergo radical surgery with partial or complete removal of the organ.
The amount of tissue cut depends on the size of the tumor and the presence of metastases. During the intervention, doctors perform reconstruction of the digestive system. For example, they replace the removed part of the organ with loops of the small intestine. The operation lasts on average from two to five hours. This is followed by a long period of rehabilitation for the cancer patient, aimed at restoring the full functioning of the digestive tract.
Distal resection
Distal resection involves removing ⅔ or ¾ of the organ. Performed when the antrum is affected.
Distal resection lasts in 3 stages:
- Inspection of the abdominal organs, ligation of the gastric arteries, cutting off the omentum, determining the boundaries of resection.
- Direct removal of a part of the stomach: delimitation of the removed and intact zones, cutting off the affected part using clamps and electrocoagulators.
- Creation of an anastomosis, formation of a stump, drainage of the abdominal cavity, suturing the wound.
General anesthesia is used as anesthesia for distal resection.
Features of digestion after resection
Regardless of whether an organ is completely or partially removed, the patient’s digestion process changes dramatically. It is important to adjust the diet and the functioning of the gastrointestinal tract so that the body continues to receive all the necessary substances. The patient may not feel hungry. You will have to eat on time, clearly calculating calories.
A common postoperative abnormality is dumping syndrome. By this concept, doctors mean the accelerated release of the contents of the organ stump into the intestines against the background of disturbances in the synthesis of enzymes and the nervous regulation of the digestive organs. Attacks usually begin after a meal rich in carbohydrates.
Among the signs of dumping syndrome:
- severe weakness;
- nausea;
- excessive sweating;
- vomit;
- regurgitation;
- cardiopalmus;
- diarrhea;
- drowsiness;
- dizziness.
Cancer patients who have had their stomach removed often develop intolerance to certain substances. More often:
- vitamin B12;
- Sahara;
- fats;
- lactose.
Doctors compensate for the lack of vitamins in the body by introducing them. Eating disorders are corrected by following a special diet.
Proximal resection
Proximal resection of the stomach for a tumor is recommended when the area of the cardia, fundus, or lesser curvature is affected. The surgeon cuts the skin from the xiphoid process to the navel, cuts off part of the organ, if necessary removes the spleen and tail of the pancreas, then ligates the arteries on the left side.
During further formation of the stump, its proximal end should correspond to the distal part of the esophagus. The esophagogastric anastomosis is immersed in the stomach to form a valve, and a nasogastric tube is inserted into the stump.
Two thirds of patients after proximal resection experience gastroesophageal reflux. Flow of the contents of the stump into the esophagus leads to ulcerations.
Food in the early postoperative period
For the first two days after surgery, the patient is prohibited from eating orally. The patient is fed protein and amino acid solutions intravenously. The composition of nutrient cocktails is determined based on the results of blood tests. The task of postoperative nutrition is to replenish the body’s need for certain substances.
Then the diet of the cancer patient is gradually replenished with new products. From the third day the following is added to the food:
- slimy soup;
- puree from fish, meat, cottage cheese;
- souffle;
- soft-boiled eggs;
- rosehip decoction;
- weakly brewed tea;
- strained, slightly sweetened compote.
On days 5-6 (if the patient’s body tolerates food well), food is supplemented with steamed omelets, grated porridge, and vegetable purees. The protein component of the diet is included in every meal. Food products are administered only with the permission of the attending physician, who constantly monitors the condition of the cancer patient and his body’s reaction to food.
The volume of portions is increased gradually. Start with 50 ml per meal (including liquid), increase to 300-400 ml by the tenth day after surgery.
After about two weeks, the patient is transferred to a special diet, which includes a complete high-protein diet with the addition of a normal amount of complex carbohydrates and fats.
Dietitians minimize the intake of cancer patients:
- “fast” carbohydrates;
- foods that irritate the digestive tract;
- nitrogenous substances;
- refractory fats, as well as components of their breakdown (for example, during frying).
Completely exclude from the diet foods and substances that stimulate the removal of bile, the secretion of the pancreas, and intestines. The food is thoroughly ground. You need to stick to this diet for 2-4 months.
Then, if there are no signs of an operated stomach, it is permissible to refuse crushed food. Prepare solid foods. A cancer patient will have to follow certain nutritional rules for at least five years.
Rehabilitation after gastric surgery
Surgery in the treatment of diseases of the stomach and duodenum remains the dominant method of treatment at the moment.
Most often, surgery is required for complications of peptic ulcer disease. For example, such as internal bleeding, perforation of an ulcer. Surgical intervention is also necessary if conservative treatment is ineffective for a long time. And the most important thing about this is that rehabilitation after gastric surgery is often necessary to restore not only the stomach itself, but also many related organs and systems. But unfortunately, such interventions often do not bring relief to patients. Moreover, sometimes the consequences of interventions can be more severe than the disease itself. Therefore, the issue of preventing postoperative complications becomes key.
Features of the recovery period
Healing after surgery may take longer than with other diseases...
After surgery, patients may experience weakness and other painful symptoms for 2 to 3 weeks. There is heaviness and distension in the epigastric region after eating. There may also be difficulties with eating. After a deep resection, a person can rarely take more than 200 - 300 ml of liquid food at a time. Also, after any type of gastrointestinal surgery, the patient may develop concomitant functional disorders. For example, such as esophagitis, gastritis, impaired gastric motility. The functional state of the liver changes. Due to the large number of complications, the patient may remain unable to work for a long time after the operation.
The goals of medical rehabilitation after gastric surgery are two key aspects. The first aspect is the prevention of postoperative disorders. The second is to maximize the patient’s ability to work.
Physical and natural factors of rehabilitation
Rehabilitation after gastric surgery should be comprehensive and consistent. Since the therapeutic effect gives results only in the totality and compatibility of factors, both physical and natural. The key components of restorative treatment are mineral waters, mud applications, physical therapy and massage.
- Mineral waters help reduce the secretory function of the stomach, namely acidity. They also improve motor function and help normalize the functioning of the liver and pancreas. Carbon dioxide, bicarbonate sodium-potassium waters are recommended. For example, such as “Essentuki 4”, “Moskovskaya”, “Smirnovskaya”.
- Mud applications also help normalize the motor function of the stomach. The best effect of therapeutic mud is 3-4 weeks after surgery.
- Physical therapy is a whole medical area that deserves to be considered separately. However, we will indicate the key positive aspects that exercise therapy gives us. Therapeutic exercise has a general tonic effect and helps strengthen the abdominal muscles. Which in turn leads to the elimination of constipation and accelerated healing of the postoperative scar.
General principles of nutrition
People with a stomach removed must constantly ensure that they consume enough food to maintain full functioning. The size of the organ after surgery is significantly reduced (or it is completely absent), the stump cannot accommodate the same amount of food.
To avoid critical weight loss during cancer treatment, you should adhere to the following recommendations:
- eat 6-8 times a day in small portions with an interval of 2-3 hours between meals;
- chew foods thoroughly;
- sit at the table while eating with your back straight;
- have dinner a maximum of two hours before bedtime;
- refuse to drink food;
- Vegetable oils should not be subjected to heat treatment, used in food as a dressing;
- Add foods to the diet one at a time. Monitor the digestive tract's reaction to food. If nausea, vomiting, or other unpleasant symptoms occur, exclude the new dish from the diet;
- fill the menu with plant and animal proteins;
- cook, bake, steam food;
- minimize the amount of spicy, fatty, sweet foods in the diet;
- drink at least eight glasses of liquid per day one hour before and after meals.
Attention: you cannot completely give up fats and carbohydrates. They supply the body of a cancer patient with the necessary energy, maintain healthy skin, hair, and nails.
People after gastric sleeve surgery should consume about 3,000 kcal per day. The approximate balance of substances recommended by doctors is as follows:
- 138 g proteins;
- 115 g fat;
- 390 g carbohydrates.
Doctors advise patients who have had an organ removed to keep a food diary. It must indicate the foods eaten, their quantity, time of meal, the body’s reaction to the components of the diet, and calorie content. This helps control body weight and eliminate substances that provoke signs of the operated organ.
Attention: after surgical treatment of cancer you need to weigh yourself every 3-5 days. If you experience weight loss, you should consult a nutritionist and adjust your diet.
After cancer surgery, it is important to completely give up bad habits and choose the right food for the patient.
Recommended Foods
In the diet of a cancer patient after resection of part of the stomach, doctors allow the following to be included:
- soups with vegetable and cereal broth;
- dried, whole grain bread;
- lean meat;
- unsweetened unleavened cookies;
- cereals (buckwheat, rice, oatmeal);
- soft-boiled eggs, white omelette;
- pasta, casseroles made from it;
- low-fat fish;
- vegetables - fresh or heat-treated;
- vegetable oils;
- sweet fruits, berries;
- nuts;
- dairy products;
- Chop fresh herbs and add to any dishes.
Doctors allow patients who have had their digestive organs removed to drink:
- weak tea;
- coffee with milk;
- unsweetened fruit drinks, compotes;
- natural fruit, vegetable, berry juices.
If there are no pronounced symptoms of the operated stomach, it is acceptable to occasionally eat snacks in the form of low-fat herring, homemade meat pate, fish or meat aspic.
Prohibited Products
Doctors recommend the following foods to be excluded from the patient’s diet after complete or partial removal of an organ during the rehabilitation period, and to be minimized in the long term (several years after surgery):
- canned meat and fish;
- smoked meats;
- fast food;
- pickles;
- sausages;
- spicy seasonings;
- semi-finished products;
- meat, fatty fish;
- rich broths;
- fresh bread;
- mushrooms;
- confectionery;
- animal fats;
- baked goods;
- legumes;
- barley, pearl barley, corn, millet, semolina;
- raw cabbage, radish;
- grapes, juice from them;
- spicy food;
- ice cream;
- dairy products with a high percentage of fat;
- chocolate;
- citrus;
- ketchup; mayonnaise;
- hard-boiled eggs.
If you have cancer, it is forbidden to drink carbonated and alcoholic drinks, strongly brewed coffee, tea, and packaged juices.
How to smooth out the main negative aspects in food
Often cancer patients are afraid that every meal will cause pain and reduce the amount of food they eat. In order to prevent critical weight loss, you need to learn how to stop the main negative aspects of nutrition that are characteristic of an operated stomach without changing the recommended diet.
The following methods help to cope with nausea and overeating:
- you need to eat slowly;
- exclude heavy, spicy foods from the diet;
- take a horizontal position no earlier than 2-3 hours after eating;
- reduce portion size by reducing the interval between meals;
- Do not consume carbonated drinks, foods, or substances that cause increased gas formation in the body.
To prevent diarrhea, doctors recommend:
- reduce consumption of sugar and fat;
- increase the amount of fiber in food;
- follow food storage rules;
- eat food warm (but not hot).
If you are intolerant to fats, lactose, sugar, introduce ingredients containing them into the diet gradually, in small portions. When negative symptoms persist, consult a doctor. You may need to take enzyme substances, painkillers, and vitamin complexes.
Prognosis for stomach cancer
Prognosis and survival depend on many factors. The doctor must know well the patient’s medical history, the specifics of the disease (type, stage, signs), the treatment procedures performed, the body’s reaction to therapy in order to collect all the information together and give a prognosis for the development of the disease.
Essentially, this is a specialist’s assessment of how the disease will further affect the person, and how the body will respond to treatment. When making a forecast, prognostic and predictive factors are taken into account. The first represents the cancer or patient characteristics that are taken into account in prognosis. A predictive factor determines how a disease will respond to a particular therapy.
Stage
It is the most important prognostic factor for gastric cancer. The main indicators or indicators are tumor and lymph nodes.
- A malignant tumor that has not spread beyond the stomach has a better prognosis.
- The number of lymph nodes affected by cancer affects the prognosis: 4 or more lymph nodes worsen the situation, 7 or more complicate the situation even more.
Location of the malignant tumor
Neoplasms that are located in the lower part of the organ (distal) have a more favorable prognosis for stomach cancer than in the upper (proximal).
Tumor type
The intestinal type of stomach cancer has a better prognosis compared to diffuse.
Tumor cells in peritoneal wash
If cancer cells are found in the peritoneal wash, the prognosis is less favorable.
Surgical removal
When the tumor process is completely removed during surgery, the prognosis will be better.
Physical education in cancer treatment
Exercise therapy is an important part of the rehabilitation of cancer patients after organ removal. Among the main tasks of gymnastics:
- stimulation of the synthesis of secretions from the digestive tract of the body;
- activation of intestinal motility;
- strengthening the abdominal muscles;
- normalization of the functioning of the respiratory and cardiovascular systems;
- developing correct posture;
- restoration of the patient's tolerance to everyday stress.
Attention: classes must be supervised by a physiotherapist.
In addition to exercise, cancer patients are advised to walk in the fresh air for at least half an hour a day. Dosed physical activity improves the functioning of the digestive system, stimulates metabolism, food absorption, and improves the patient’s mood.
Lifting heavy objects is contraindicated for patients. In the first year after removal, you cannot lift a total of more than 3 kg, then - more than 5 kg.
Gastrectomy
Gastrectomy is the total removal of the stomach. The integrity of the digestive tract is restored by creating an anastomosis between the esophagus and the small intestine. The surgeon applies clamps to the stomach ligaments, which allows it to be cut off from the esophagus and duodenum, then an anastomosis is formed. The intervention can be performed using open, laparoscopic or combined access. On average, the operation lasts no more than four hours, the minimum duration is 2 hours.
How is the operation performed?
The operation is usually performed through a large incision in the abdomen (laparotomy). Laparoscopy is rarely used. Although surgery through short incisions is less traumatic, there is no convincing evidence that it can provide similar patient survival rates.
The doctor removes the stomach, cutting it at a distance of about 5 cm from the tumor. For aggressive types of cancer, the indentation is increased to 7 cm. The stomach is removed along with the greater and lesser omentum, tissue and lymph nodes. Immediately after the intervention, a histological examination of the material is performed to ensure the absence of cancer cells at the border of the removed tissue.
Our expert in this field:
Moiseev Alexey Andreevich
Oncologist, chemotherapist, Ph.D.
Candidate of Medical Sciences
Experience: More than 19 years
Call the doctor
Call the doctor
Send documents by email The possibility of treatment will be reviewed by the chief physician of the clinic.
The operation is always complemented by lymph node dissection. The number of lymph nodes removed depends on the stage of the pathology, size and location of the tumor. Typically, the more nodes a doctor removes, the better the patient's survival rate. But the surgeon removes only the first and second order lymph nodes. Third-order nodes are considered remote. Their removal increases the risk of complications, but does not increase patient survival.
Introduction
Gastric cancer is one of the most common cancer diseases worldwide [7, 14, 18, 28, 30], occupying a leading position in the mortality structure (803 thousand deaths annually) [60]. The incidence of stomach cancer varies significantly in different parts of the world. The highest incidence of this disease was found in South Korea - 66.5-72.5 per 100,000 men and 19.5-30.4 per 100,000 women [51]. Similar figures in the USA are 10 times lower [49].
Stomach cancer took second place after lung cancer in the structure of cancer incidence in Russia in 2007. The number of registered cases was 41,941, which amounted to 17.5% of the total number of cancer diseases. In the structure of mortality from malignant diseases, stomach cancer accounts for 13.8% [27].
Currently, the only radical treatment method for patients with stomach cancer is surgery. Radiotherapy and chemotherapy complement surgery and do not play a decisive role in the duration of the disease-free period and life expectancy of patients [9, 10, 19, 24, 25]. The most common surgery for stomach cancer is gastrectomy (GE). Depending on the location and stage of the tumor process, surgical interventions can be extended, combined, and also accompanied by lymphadenectomy (LAE) to one extent or another [16, 29, 31, 33].
The choice of the optimal volume of surgical intervention for gastric cancer currently causes a lot of controversy. This is due to the fact that improving the results of treatment of resectable gastric cancer is not always directly related to expanding the scope of radical surgery. The main subject of discussion is the indications for LAE, its scope and long-term results [3, 36, 43]. Traditionally, radical operations for cancer of various locations include mandatory removal of regional lymph nodes as a single block.
In the late 70s in Japan, “extended” LAE was elevated to the “rank” of a national recommendation (Japanese Research Society for Gastric Cancer - JRSGC, 1981).
Currently, the use of operations in combination with extended LAE is considered as the most promising direction that can increase the effectiveness of treatment of resectable gastric cancer [2, 4, 7, 9, 11, 15, 23, 31-33, 42, 50, 52, 53].
The issue of indications for splenectomy (SE) during radical operations for gastric cancer continues to be debated in the literature. The feasibility of routine SE as a component of extended gastrectomy for gastric cancer should be determined by the interaction of two factors: on the one hand, the frequency of metastases affecting the lymph nodes of the hilum of the spleen, on the other, a prerequisite for improving long-term results by preserving the spleen as an immunocompetent organ. Of no small importance is the fact of an increased risk of developing subdiaphragmatic abscesses and pancreatic necrosis of the distal pancreas (P) after SE [10, 26, 42].
The clinical consequences of SE have been studied by many authors. It is believed that the early postoperative period can be complicated by subdiaphragmatic abscess [45], pancreatitis [21, 44, 56], sepsis [5], suppuration of the postoperative wound, eventration, adhesive intestinal obstruction [21], bleeding, and intestinal fistula formation [13, 20 ], thrombosis of the superior mesenteric and portal veins [47]. Other authors point to the possibility of developing extra-abdominal complications, such as pneumonia, pleurisy, thromboembolism of the pulmonary artery and its branches [14, 38, 45].
Tumors of the upper and middle third of the stomach can metastasize to the lymph nodes located in the area of the splenic artery and hilum of the spleen (groups No. 10, 11). According to some authors, LAE in volume D2 included SE and distal resection of the pancreas, which is reflected in numerous Japanese studies in the 80s [9]. It was believed that SE and distal resection of the pancreatic tail make it possible to most fully perform LAE of nodes of groups No. 10 and 11 [6, 9, 11, 35].
Subsequently, some authors insisted on SE and resection of the pancreas if the tumor had spread beyond the serous membrane of the stomach or in the presence of visible metastases in the area of the splenic vessels/splenic hilum [6, 9-12].
Undoubtedly, the most important prognostic factor in assessing the radicality of a surgical operation is a pathomorphological examination of the resection margins [9, 23]. Accordingly, in the case of direct tumor ingrowth into the spleen or pancreas in the absence of obvious damage to the lymph nodes, the need for a combined operation is undeniable [8, 9, 12, 23, 24].
According to K. Okajima et al. [54], the frequency of metastasis to the lymph nodes of the hilum of the spleen and the splenic artery for tumors occupying the upper and middle third of the stomach reaches 26.7%, with distal localizations it is close to zero.
A.F. Chernousov et al. [31] consider SE to be indicated only for tumors of the upper and middle third of the organ that invade the serous membrane and poorly differentiated forms of cancer.
In the last decade, there has been a trend in the surgical community towards organ-conserving operations. If we are talking about preserving the spleen, this is certainly justified.
In 2012, a systematic review of studies was published comparing the results of surgical treatment of gastric cancer depending on SE and distal resection of the pancreas as components of extended LAE [58]. Data from Medline, Embase, and Cochrane Central Register of Controlled Trials were analyzed from January 1998 to December 31, 2009. 42 studies with a total number of patients of 6354 met the criteria for a systematic review of the literature. In 4 randomized trials there were no statistically significant differences in the total number of complications and mortality was not identified. Of 6 prospective studies comparing different LAE techniques, spleen and pancreas preservation was associated with fewer complications in 2, fewer postoperative complications and deaths in 1, and no statistically significant differences in the remainder. In retrospective studies, spleen preservation was associated with fewer complications in 3, pancreatic preservation in 5, and decreased mortality in 1. Of the 33 remaining retrospective studies, 10 studies on spleen preservation and 13 without pancreatic resection showed statistically significant differences in mortality rates and the number of complications did not have. Randomized trials found no difference in survival.
According to the results of two large randomized European studies, a high level of complications and mortality was associated with SE and distal resection of the pancreas.
Given that these conclusions were drawn using a post hok subgroup statistical method, they must be interpreted with extreme caution. Some researchers believe that such low 5-year survival rates could be associated with extremely high perioperative mortality rates [37, 39].
Randomized studies [40, 41] compared the results of LAE in volumes D2 and D1. There was no difference between spleen-preserving operations and SE, but the study was supported by specific patient selection, exceptional in-hospital care, and the participation of surgeons with extensive experience.
A. Csendes et al. [39] and W. Yu et al. [61] noted a trend towards an increase in 5-year survival in the group of patients after SE.
A study by K. Okinaga et al. [55] was relatively small (43 patients) and also did not demonstrate significant benefits of spleen preservation. Along with this, the authors postulated that spleen lymphocytes have increased cytotoxic activity in the early stages of the tumor process and significant suppressive activity in the later stages of gastric cancer. The authors also noted an increase in survival rate with spleen preservation and immunotherapy.
H. Furukawa et al. [46] compared the results of LAE in the D2 volume with resection of the tail of the pancreas and standard LAE in the D2 volume and also did not reveal a statistically significant increase in the number of complications and survival rate. One possible explanation for the lack of statistical differences in results is the insufficient number of patients.
Of interest are the results of a meta-analysis of three randomized cohort studies [59] on the effect of SE as a combined stage of LAE in gastric cancer. The location and stage of the tumor played a decisive role in the indications for SE. Postoperative mortality and the number of complications did not differ significantly in both groups. The number of removed lymph nodes was higher in the SE group. The duration of the operation and hospitalization period was the same. There was also no difference in the number of reoperations. The data obtained indicate that performing “routine” SE does not affect the 5-year survival of patients and should not be recommended as a standard operation.
Despite the numerous studies cited in the latest JGCA clinical guidelines [48], LAE in volume D2 complements SE for T2-T4 tumors located along the greater curvature in the upper third of the stomach.
In 2002, a multicenter randomized study of the feasibility of SE in cancer of the proximal stomach was launched in Japan, designed to finally resolve this issue [57]. The examination and treatment data of 505 patients, divided into two groups, were studied. The inclusion criteria for the study were T2-T4, N0-2, M0, tumor localization not along the greater curvature, histologically confirmed adenocarcinoma. In 2010, JCOG published the interim results of this study. In the early postoperative period, 3 patients died (2 in the spleen preservation group, 1 in the SE group). The number of patients with postoperative complications was significantly higher (30.3%) in the SE group than in the group with a preserved spleen (16.7%; p
<0.0001).
Blood loss was significantly greater in the SE group: 390.5 ml versus 315 ml when the spleen was preserved ( p
= 0.002). There were no statistically significant differences in the duration of operations (on average 231 and 224 minutes, respectively). Recruitment of patients was completed in 2009, and final results will be published in 2014.
Since 2005, a similar randomized trial has been conducted at the Russian Cancer Research Center named after. N.N. Blokhin RAMS. Russian oncologists are developing and applying the technique of LAE in volume D2 with preservation of the spleen and performing complete LAE at its hilum, calling only such operations spleen-preserving, in contrast to gastrectomies with leaving the spleen [28].
Thus, literature data indicate that the question of the advisability of simultaneous removal of the spleen when performing gastric gastric cancer in patients with different tumor localizations has not yet been resolved. Data on the state of immunity of cancer patients before and at different times after surgery are ambiguous. In addition, taking into account the diverse functions of the spleen, the influence of SE on the course of the immediate postoperative period and the health status of patients in the long term after surgery has not been fully studied.
Material and methods
The study included 118 patients with stomach cancer, operated on from 2006 to 2011 at the Faculty Surgery Clinic named after. N.N. Burdenko PMGMU named after. THEM. Sechenov.
Depending on the nature of the intervention, all patients were divided into 2 groups: 61 patients were included in group 1 (GE and SE), and 57 patients were included in group 2 (GE with spleen preservation). Among those operated on there were 72 men and 46 women.
Both groups were homogeneous in gender and age. The study predominantly included male patients over 60 years of age. 79 (67%) patients were diagnosed with concomitant, competing diseases.
A homogeneous distribution of concomitant diseases was revealed in both groups. The most common diseases were the cardiovascular system.
62 (52.5%) patients had concomitant therapeutic diseases, 42.7% had two or more diseases, which required preoperative preparation. The most common among them were diseases of the cardiovascular system and respiratory organs: coronary heart disease - in 55 patients, arterial hypertension - in 70, chronic obstructive pulmonary disease - in 36. According to the results of calculating the body mass index, 22 patients were obese.
The examination included standard laboratory and instrumental methods (general blood and urine analysis, biochemical blood test, coagulogram, electrocardiography, pulmonary function test).
A comprehensive study of immune status was also performed. Blood sampling was performed before surgery to determine initial parameters, on the 7th day after surgery and in the period from 14 to 20 days after surgery. Patients admitted for a follow-up examination underwent a similar study 3 months, 6 months and 1 year after surgery, then every year for 5 years.
All patients we observed, taking into account the presence of secondary immunodeficiency, in the perioperative period and before discharge from the hospital received immunomodulatory therapy with the drug Galavit, a phthalhydroside derivative [1, 17, 24]. A special feature of this drug is the presence, in addition to immunomodulatory, pronounced anti-inflammatory properties. Its main pharmacological effects are associated with its effect on the functional activity of macrophages. When these cells are hyperactivated, galavit reversibly inhibits the production of tumor necrosis factor and interleukin (IL)-1, as well as reactive oxygen species. The functional state of macrophages is normalized, normal cytokine production and antigen-presenting function are restored. Galavit stimulates the functional activity of neutrophils, increasing the absorption and intracellular killing of bacteria. The consequence of this is an increase in the body’s nonspecific resistance to infections. Galavit does not affect the normal level of natural killer cell cytotoxicity, but at initially low values it restores cytotoxicity to normal values.
In terms of the localization of the oncological process, stages and nature of the operations performed, both groups of patients were homogeneous.
In our work, we used the TNM classification (UICC, 2002), according to which there were 22 and 46 patients with stage I and II disease in both groups, respectively, stage III - 35 (16 in the 1st and 19 in the 2nd), Stage IV - 15. There were 50 patients with stage III and IV disease. In 7 patients, the tumor grew into adjacent anatomical structures (T4), which required combined surgical interventions. It is obvious that early detection of cancer and timely radical surgical treatment improve both immediate and long-term results of surgical treatment of patients with gastric cancer.
In both groups, infiltrative-ulcerative forms of cancer predominated (94%), with localization in the body of the stomach (64%), and a low degree of tumor differentiation (54%). Spread of stomach cancer to the esophagus was observed in 28 patients. Involvement of the greater curvature of the stomach in the tumor occurred in 61 (52%) patients.
Results and discussion
Of the 118 gastrectomies, 88 (75%) were combined. Gastrectomy was combined with resection of the colon in 3 patients, with resection of the pancreas in 9, with resection of the esophagus in 81. Gallstone disease served as the basis for removal of the gallbladder in 5 patients, at the same time, a fundamental cholecystectomy was performed in 49 patients during LAE in the volume D 2 ,5 with circular dissection of the hepatoduodenal ligament.
In the majority of cases, radical surgery with LAE (90%) was performed in the volume of D2, D 2.5, D3 - 73, 23 and 14 patients, respectively.
During most operations, one of the variants of fibrin glue was applied to the anastomotic area to improve local regeneration processes.
Depending on the stage of gastric cancer and the variant of the histological structure of the tumor, standard chemotherapy treatment was performed: most often systemic adjuvant chemotherapy, and in 8 patients after cytoreductive operations - curative chemotherapy. Cytoreductive operations were performed in the presence of distant metastases in the upper mediastinum, liver, lungs, retroperitoneum, as well as in the presence of ascites, peritoneal carcinomatosis, metastases of Krukenberg, Schnitzler, Virchow, and Sister Mary Joseph.
Assessing the physiological capabilities of the body of patients suffering from stomach cancer, the majority of whom are elderly and senile people, is difficult and controversial, but surgical intervention is the only radical method that gives any hope for recovery.
A number of authors recognize the forced reduction of surgical activity due to the patient’s age and the presence of concomitant diseases of the heart and lungs [17, 22, 29, 34]. The number of patients undergoing exploratory laparotomies, thoracotomies, and palliative interventions is large [32]. We also encountered similar facts and in most cases we were able to perform radical or cytoreductive surgical interventions during repeated operations in such patients.
Traumatic (combined) surgical interventions are contraindicated in patients with severe cardiovascular and pulmonary diseases in the stage of decompensation, with severe impairment of liver and kidney function, and decompensated diabetes mellitus.
Simultaneously with the preoperative examination, the patients underwent correction of identified disorders of the heart and lungs, electrolyte and nutritional changes caused by inadequate nutrition.
The administration of high-calorie nutrition through a probe passed through the tumor narrowing, simultaneously with intravenous infusions of amino acids, proteins, vitamins and microelements (in a total daily dose of 2500-3000 kcal) made it possible to compensate for the nutritional deficiency. To assess the effectiveness of the therapy in all patients, the thickness of the skin fold at the level of the middle third of the shoulder was measured, the content of total protein and the level of transferrin, protein fractions, indicators of immune status, albumin-globulin coefficient were determined, the level of electrolytes was monitored, the loss of daily nitrogen and nitrogen balance were measured.
All patients receiving enteral nutrition received special nutritional liquid mixtures. Along with replacement of excreted nitrogen, patients underwent correction of the level of total protein and albumin by administering 10 and 20% solutions of albumin, plasmalit and plasma.
The criteria for the adequacy of the course of preoperative therapy were normalization of the level of blood electrolytes, an increase in total protein and blood albumin, an increase in the albumin-globulin index, positive or zero nitrogen balance, maintenance of moderate hemodilution (35-37%) with a tendency towards normalization of immune status indicators: decrease the total number of leukocytes and lymphocytes, an increase in the number of T-lymphocytes, a decrease in active T-lymphocytes, a decrease in quantity and percentage of T-suppressors and B-lymphocytes.
Depending on various factors, issues of preoperative preparation in each specific situation were resolved individually.
The indications for preservation of the spleen were the absence of direct tumor invasion into its capsule or vessels.
During the operation, while preserving the spleen, the short gastric vessels were ligated and transected as close as possible to the splenic capsule, while the tissue and lymph nodes from the hilum of the spleen were displaced into the complex to be removed.
In total, out of 61 operated patients of group 1, complications developed in 22 (36.1%). In this case, 41 patients had the esophagus resected: 32 - the abdominal section, 9 - the abdominal and lower thoracic sections. In 9 cases, the operation was supplemented with resection of the crura of the diaphragm, in 9 cases - with distal resection of the pancreas.
Among patients in group 1, the main intra-abdominal complication was an abdominal abscess localized in the left subdiaphragmatic space. This complication was observed in 6 (9.8%) patients. Timely diagnosis of this complication, antibacterial therapy, and minimally invasive interventions under ultrasound control made it possible to achieve a cure for all patients.
Acute edematous pancreatitis was diagnosed in 4 (6.6%) patients after GE with resection of the lower third of the thoracic esophagus through a transhiatal approach. The main manifestations of edematous pancreatitis were an increase in the level of amylase in drainage discharge and in the blood, as well as an increase in the size of the pancreas according to ultrasound. One patient was diagnosed with pancreatic tail necrosis.
The development of postoperative pancreatitis in the 1st group of patients was a characteristic complication and only in 2 observations was associated with distal resection of the pancreas.
In order to prevent postoperative pancreatitis in extended PAE, we used a synthetic analogue of somatostatin (octreotide).
In 7 (11.5%) patients, complications required additional surgical interventions in the postoperative period. Ultrasound-guided punctures and drainage of abdominal abscesses were performed in 5 (8.2%) patients. One patient had to undergo a lumbotomy due to pancreatic necrosis and phlegmon of the retroperitoneal tissue.
The greatest number of extra-abdominal complications were observed from the chest organs; in total, they developed in 10 (16.4%) patients. Exudative pleurisy occurred in 4 (6.6%) patients.
In two cases, left-sided pleurisy was a complication of acute postoperative pancreatitis. In another patient, pleurisy was combined with an abscess of the left subphrenic space.
Pneumonia was diagnosed in 5 (8.2%) patients, 1 of them developed a fulminant form of herpes viral pneumonia, which caused death on the 2nd day after surgery.
The relatively high incidence of complications from the lungs and pleural cavity is due to the initial chronic diseases of the respiratory system that patients had (bronchial asthma, chronic bronchitis, emphysema), as well as intervention in the posterior mediastinum with proximal localizations of the cancer tumor.
Complications from the cardiovascular system were noted in 1 (1.6%) patient. He developed thromboembolism of small branches of the pulmonary artery with the development of infarction pneumonia. The diagnosis of thromboembolism was established based on the results of MSCT angiopulmonography. Against the background of anticoagulant, antibacterial and cardiotropic therapy, recovery occurred.
Of the 57 patients in group 2, 53 underwent radical surgery. It should be noted that performing SE during an obviously cytoreductive operation was considered inappropriate. Radical operations were supplemented by resection of the esophagus in 41 patients: abdominal - in 31, lower thoracic - in 10. Resection of the crura of the diaphragm was performed in 13 cases. The volume and number of combined interventions did not differ significantly between the two groups of patients. Complications were diagnosed in 10 (17.5%) patients.
It seems important that when the spleen was preserved, abscesses of the subdiaphragmatic space did not develop, and there was also a tendency to reduce the frequency of postoperative wound suppuration. In patients of group 2, extra-abdominal complications associated with concomitant diseases of the cardiovascular and respiratory systems predominated.
During cytoreductive operations, we sought to preserve the spleen in all situations, except for direct tumor invasion into the vessels of the splenic pedicle or the splenic capsule.
Complications from the cardiovascular system were observed in patients: in 1 - acute myocardial infarction on the 12th day after surgery, in another 1 - acute left ventricular failure, which arose on the 3rd day after surgery against the background of previous concomitant paroxysmal atrial fibrillation and relieved as a result of intensive cardiac therapy. Pneumonia was diagnosed in 5 (8.8%) patients, and suppuration of the postoperative wound was detected in 4 (7%). There were no deaths in this group.
Thus, the use of a differentiated approach depending on the location of the tumor and the degree of involvement of the esophagus in patients burdened with cardiopulmonary diseases made it possible to significantly improve the immediate results of treatment, including expanding the indications for radical operations in patients with high anesthetic risk, and reducing the number of early postoperative complications.
Before surgery, were patients in both groups characterized by lymphopenia, a decrease in the content of the CD8+ antigen and, in connection with this, an imbalance of the subpopulation? T-cell link against the background of a decrease in anti-infective immunity and an increase in the content of activation markers CD25+, in addition, there was an increase in the concentration of immunoglobulins of classes M and G. Statistically significant differences in indicators before surgery were not detected in both groups.
The absence of a difference in the indicators of immune status before surgery indicates the homogeneity of both groups of patients observed by us, and secondary immunodeficiency, expressed to varying degrees and established in all patients, is a consequence of the influence of a malignant tumor.
When studying the immune status on days 7-10 after surgery, it was found that the level of IgM and T-active lymphocytes was significantly higher in group 1, which indicates an early reaction of the immune system in response to the traumatic effects of the operation. The level of B-lymphocytes, circulating immune complexes (CIC), IL-1B and IL-10 against the background of a continuing decrease in the number of proinflammatory cytokines was significantly lower than in group 2.
The worsening of previous immunodeficiency in patients after SE is also reflected in a decrease in the rate of spontaneous and stimulated NBT test.
On the 14-20th day after surgery, no significant differences in immune status indicators were detected, since in patients of both groups, against the background of immunomodulatory therapy, they depend to a greater extent on the presence of purulent-septic complications than on the type of operation.
After 3 months, no significant differences were also found due to the activation of compensatory mechanisms of the immune system and ongoing treatment with Galavit.
By 6 months after surgery, in the 1st group of patients the level of T-total lymphocytes was significantly higher than in the 2nd group. This is due to the end of the use of immunomodulatory drugs and the suppression of the phagocytic component of immunity in the SE group, in which a decrease in the level of early T-lymphocytes and the indicator of the stimulated NBT test, IL-8, was also observed.
1 year after surgery in group 1, the level of T-active lymphocytes, CEC, tumor necrosis factor was significantly higher, and the level of lymphocytes, T-general, and T-helper cells was significantly lower than in group 2.
Oncological radicalism was assessed based on survival rates in both groups of patients. In the 1st group of patients, the average survival rate was 26 months (16.0; 40.0), in the 2nd group - 23.5 (13.0; 36.0).
Among 57 radically operated patients of group 1, long-term results were observed in 50 (82%). The 2-year survival rate was 55.2±0.2%, and the 3-year survival rate was 34.6±0.2%. Among 53 radically operated patients of group 2, long-term results were observed in 45 (79%). The 2-year survival rate was 54.8±0.3%, and the 3-year survival rate was 36.4±0.3%.
When analyzing the 2- and 3-year survival rates of operated patients, depending on the stage of the disease, a clear correlation is visible: the higher the stage, the shorter the life expectancy. Of the 50 patients of the 1st group, followed in the long term, after surgery for 2 years or more, 12 (80±1.5%) lived with stage I of the disease, 8 (72.7±1.3%) with stage II. , at stage IIIA - 11 (57.8±0.9%), at stage IIIB - 3 (37.5±0.4%), at stage IV - 3 (25±0.09%). Overall 2-year survival rate was 56.92±0.2%. 22 (33.8±0.2%) patients lived for three years or more. The 3-year survival rate for stage I of the disease was 60±1.0%, for stage II - 36.36±0.9%, for stage IIIA - 36.84±0.9%, for stage IIIB - 12.5 ±0.1%, at stage IV - 8.3±0.08%.
In group 2, 2- and 3-year survival rates depended on the stage of the disease, the same as in group 1: the higher the stage, the shorter the life expectancy. Of the 45 patients followed long-term after surgery, 10 (80±1.5%) patients lived for 2 years or more with stage I of the disease, with stage II - 7 (72.7±1.3%), with stage IIIA - 10 ( 57.8±0.9%), at stage IIIB - 4 (37.5±0.4%), at stage IV - 3 (25±0.09%). Overall 2-year survival rate was 55.66±0.2%. 23 (33.8±0.2%) patients lived for three years or more. The 3-year survival rates depending on the stage of the disease were: at stage I - 60±1.0%, at stage II - 36.36±0.9%, at stage IIIA - 36.84±0.9%, at Stage III - 12.5±0.1%, stage IV - 8.3±0.08%.
Thus, the lower the stage of the disease, the more favorable the prognosis and the higher the 2- and 3-year survival rates.
The factor of lymph node damage has a significant negative impact on long-term results. There were 1.5 and 2.6 times more patients without metastases who survived the 2- and 3-year follow-up than patients with metastases in the lymph nodes. Patients without metastases to regional lymph nodes are 2 times more likely to survive than patients with lymphogenous metastases. As the follow-up period increases, the chances of survival increase.
The survival of patients after radical surgery for gastric cancer is influenced by a number of factors. The main ones are the stage of the disease, the anatomical shape of the tumor, metastases to the lymph nodes, the depth of tumor invasion, the location of the tumor, the extent of damage to the esophagus and the extent of surgical intervention performed.
Overall 2-year survival rate in both groups of patients was 56.92±0.2%. Of the 95 patients followed, 22 (33.8±0.2%) lived for 3 years or more. The 3-year survival rates for stage I of the disease were 60±1.0%, for stage II - 36.36±0.9%, for stage IIIA - 36.84±0.9%, for stage IIIB - 12.5 ±0.1%, at stage IV - 8.3±0.08%.
Of the 118 patients operated on, 14 did not have metastatic lesions of the lymph nodes. Among them, 9 (66.6%) people lived 2 years, 5 (33.4%) lived 3 years. The remaining 104 patients had damage to regional lymph nodes, 59 (57%) survived 2 years and 45 (34%) patients survived 3 years.
According to modern literature, 2-year survival rates for patients with stomach cancer vary from 36 to 58%, 3-year survival rates - from 25 to 52%. Our results of 2- and 3-year survival in obviously seriously ill patients turned out to be comparable and significant ( p
<0.005) did not differ and amounted to 57 and 34%, respectively.
Thus, we can talk about the legitimacy of the chosen treatment tactics from the point of view of oncological radicalism, since preservation of the spleen allows to reduce the number of postoperative complications and does not affect long-term treatment results.
A comparison of survival depending on the type of surgical intervention (with splenectomy or spleen preservation) indicates that 2- and 3-year survival rates do not differ significantly in both groups of patients.
Regardless of the location and extent of the cancer process, in the absence of direct invasion of the tumor into the splenic vessels, splenic capsule or pancreas, preservation of the spleen during lymphadenectomy with complete removal of lymph nodes in the area of the splenic hilum allows to reduce the number of early postoperative complications and does not significantly affect the long-term survival of patients stomach cancer.