Intestinal infection in children is a group of infectious diseases of various etiologies that occur with primary damage to the digestive tract, toxic reaction and dehydration of the body.
In children, intestinal infection is manifested by increased body temperature, lethargy, lack of appetite, abdominal pain, vomiting, and diarrhea. Diagnosis of intestinal infection in children is based on clinical and laboratory data (history, symptoms, excretion of the pathogen in feces, detection of specific antibodies in the blood). For intestinal infections in children, antimicrobial drugs, bacteriophages, and enterosorbents are prescribed; During the treatment period, it is important to follow a diet and rehydrate.
Intestinal infection in children is an acute bacterial and viral infectious disease accompanied by intestinal syndrome, intoxication and dehydration. In the structure of infectious morbidity in pediatrics, intestinal infections in children occupy second place after ARVI. Susceptibility to intestinal infections in children is 2.5-3 times higher than in adults. About half of the cases of intestinal infection in children occur at an early age (up to 3 years). Intestinal infection in a young child is more severe and may be accompanied by malnutrition, the development of dysbacteriosis and enzymatic deficiency, and decreased immunity. Frequent repetition of episodes of infection causes disruption of the physical and neuropsychic development of children.
What organs are affected by intestinal infections?
In children and adults, intestinal infections can affect various organs of the digestive system:
- Stomach - when its mucous membrane becomes inflamed, gastritis develops. It is accompanied by nausea, vomiting and pain in the area above the navel.
- Stomach and small intestine - gastroenteritis develops, which is characterized by loose, watery stools containing undigested food debris. Patients complain of pain around the navel.
- Stomach, small and large intestines - gastroenterocolitis develops. In this case, the patient feels pain not only in the abdomen, but also during bowel movements. The stool is loose, frequent, sometimes mixed with blood.
- Small intestine - when the mucous membrane of this section of the gastrointestinal tract becomes inflamed, enteritis develops. This infectious disease is not characterized by nausea, vomiting and abdominal pain. The stool is frequent and watery.
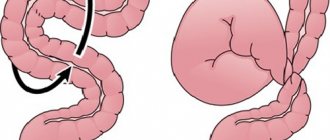
- Large intestine - when this part of the digestive system is damaged, colitis develops. The disease is characterized by pain localized in the lower abdomen. Acute diarrhea develops, sometimes mixed with blood and mucus.
- Large and small intestines - inflammation of the mucous membrane, which causes severe abdominal pain, loose stools, and a frequent urge to empty the bowel.
Causes
An intestinal infection in a child can be caused by pathogenic or opportunistic viruses and bacteria. The main route of transmission of the bacterial pathogen of ACI is fecal-oral. In this case, infection often occurs from the consumption of unwashed, stale, thermally untreated foods and unboiled water.
The viral pathogen of ACI has an airborne route. The virus or bacteria enters the mouth, stomach, and then the intestines. There the pathogen takes hold and begins to actively multiply, which ultimately leads to intoxication of the child’s body.
Causes of intestinal infection
Infection with intestinal infections occurs through the fecal-oral and household contact routes. Bacteria, viruses and fungi are transmitted from a sick person to a healthy person through shared objects (toys, dishes, towels, etc.). Children are the most susceptible to the disease. This is due to the following reasons:
- Children have lower acidity of gastric juice compared to adults.
- An incompletely formed immune system cannot resist pathogenic microflora.
- Children are more likely than adults to not observe the rules of personal hygiene.
- Children attending kindergartens and schools have closer contact with peers, which facilitates the process of transmission of infection.
Intestinal infection is often called the disease of dirty hands. Young children often ignore basic hygiene standards - they forget to wash their hands after using the toilet and before eating, they often pick up unwashed objects previously handled by infected peers, they play with pets, which can also be carriers of various infections, etc.
Classification
In medicine, acute intestinal infections are divided depending on the type of pathogen that caused them. Therefore, there are two large groups of diseases - bacterial and viral. In turn, each group has subgroups:
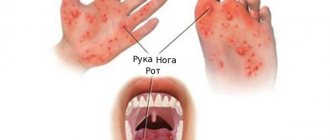
- Viral – this includes rotavirus infection, adenovirus (intestinal flu) and enterovirus infection.
- Bacterial - This includes dysentery (shigellosis) and botulism, which occurs due to the consumption of home-canned foods.
Symptoms
Acute intestinal infection (ACI) is characterized by a number of signs, which doctors divide into general and local. Local symptoms of the disease include:
- vomit;
- diarrhea;
- pain in the abdominal area;
- damage to the mucous membrane of the stomach and intestines.
Local symptoms of bacterial or viral acute intestinal infection:
- hurts, dizzy;
- body temperature rises;
- malaise, weakness, drowsiness;
- signs of dehydration appear - dry mucous membranes in the mouth, viscous saliva, a gray tint appears on the skin, the volume of urine and the number of urinations are reduced by 50%. In infants, the fontanel on the head sinks and the pulse quickens.
First aid
When an intestinal infection occurs, many parents begin to independently select medications to eliminate unpleasant symptoms in their child. However, before starting treatment, you should consult your pediatrician. Self-medication is dangerous, as it can lead to complications.
It is important for parents to know that if their baby complains of deterioration and blurred vision, or signs of strabismus appear, then they should immediately call an ambulance. These symptoms are characteristic of deadly botulism. Before the ambulance arrives, the child must be given first aid:
- put on the bed and prepare a container for vomit;
- rinse the stomach - give 1–1.5 liters of water to drink, then induce vomiting;
- if there is a chill, then you need to warm your feet with a heating pad and cover them with a blanket;
- ensure that the child constantly drinks warm water in small portions;
- in case of acute diarrhea and vomiting, it is necessary to give the drug “Regidron” - this will help avoid dehydration of the body.
If your stomach hurts badly, you can give painkillers before the doctor arrives. However, it should be borne in mind that the effect of the drug may complicate the diagnosis of the disease. In the future, if the parents follow all the doctor’s recommendations, the child will gradually improve. Correctly selected treatment, diet and protection of the body from dehydration will allow the baby to recover on the 4th–5th day.
Prevention of intestinal infection
In order to prevent the development of intestinal infection, parents must adhere to the following preventive rules:
- From a very early age, develop primary personal hygiene skills in your child.
- Carefully monitor the cleanliness of the child’s hands and ensure the cleanliness of the objects surrounding the baby.
- Drink only clean water.
- Carefully process fruits and vegetables before giving them to your child.
- Regularly wet clean your home with disinfectants.
If your baby does develop an intestinal infection, you should immediately seek medical help from a specialist. Doctors at the SM-Doctor clinic for children and adolescents will help you quickly identify the disease and prescribe the necessary treatment.
Diagnosis of intestinal infection in a child
To determine the type of infection and the type of pathogen, a pediatrician or pediatric infectious disease specialist collects an anamnesis and performs an examination. Then the specialist asks to submit the feces for bacteriological examination. In severe, complicated forms of the disease, the doctor may prescribe:
- analysis of cerebrospinal fluid, urine - for bacteriological examination;
- blood test - culture for sterility: this method helps to identify existing harmful bacteria, which indicate that pathological processes are occurring in the child’s body.
In addition, the pediatrician carries out differential diagnosis with acute appendicitis, pancreatitis, biliary dyskinesia and other pathologies. Therefore, a specialist can schedule a consultation with a pediatric surgeon and gastroenterologist.
When is hospitalization needed?
If the intestinal infection is severe, the child must be hospitalized. The appearance of blood in the stool indicates that the infection has reached the large intestine. In the vast majority of cases, this indicates its bacterial origin. This requires injection of an antibiotic. This treatment is best received in a hospital setting.
You should definitely go to the hospital if the parents are unable to give their child something to drink. It is better to call an ambulance before the patient shows the first signs of dehydration. To normalize fluid reserves in the body, intravenous replenishment is required.
Treatment of rotavirus infection in children
Early diagnosis and timely initiation of therapy are extremely important in the treatment of rotavirus infection in children. It is necessary to replenish the loss of fluid in the body: use rehydration solutions (rehydron), give the child a drink every 15 minutes containing 1 tablespoon of salt, 2 tablespoons of sugar, 1 liter of water and half a lemon. You can defeat the virus and cope with intoxication thanks to enterosorbent drugs, including activated carbon, Smecta and Enterosgel. Sorbents bind viruses and remove them from the body, but they can be given to a child for no more than three days: these drugs can cause constipation, which prevents the removal of toxins from the body.
For rotavirus infection, it is strictly forbidden to use antibiotics, as they can destroy bacteria, but not viruses. In addition, antibiotics can harm the child’s already disturbed intestinal microflora.
A sick child needs a strict diet. Infants should continue to be breastfed, since the necessary antibodies enter the body through mother's milk. It is also necessary to give the child a rehydration solution, lean porridge, mashed potatoes, baked apples rich in natural sorbent, crackers, bananas, and low-fat kefir. Small meals: the child should be fed frequently and in small portions.
Doctors often prescribe enzymes for patients: Creon, Pancreatin, etc. These medications help normalize digestion and assimilate food. After recovery, it is recommended to take medications that restore the disturbed intestinal microflora. It is also useful to give children compote of dried fruits.
Treatment
Many intestinal infections in children do not require treatment and go away on their own due to the protective action of the immune system. Therefore, the main task of parents is to provide maximum support to the child’s body during this period.
Protecting the body from dehydration
To avoid dehydration due to vomiting and diarrhea, you need to maintain a normal level of water-salt balance. Special rehydration medications will help with this.
Reduce Heat
If a child has a high temperature due to an acute intestinal infection, it should be brought down. Fever, like diarrhea and vomiting, causes fluid loss and can lead to dehydration. Therefore, in order to maintain normal water balance and reduce symptoms of intoxication, you need to give your child an antipyretic drug. In this case, you should strictly adhere to the pediatrician’s recommendations and give the medicine strictly in a volume that corresponds to the baby’s age.
Antibiotic therapy
According to WHO, for bacterial and viral intestinal infections, antimicrobial drugs should be taken in the following cases:
- if there is blood in the vomit and feces;
- There is acute diarrhea for several days.
It should be remembered that only the attending physician prescribes medications and treatment regimens. Self-medication can significantly worsen the baby’s condition.
Reception of sorbents
To prevent intoxication in a child, sorbents should be given if an intestinal infection occurs. According to WHO, there is no official evidence that these drugs help in the fight against such infectious diseases. However, they do not cause harm to the child’s body - for this reason, pediatricians quite often include them in the treatment regimen.
Maintaining a gentle diet
The disease progresses much worse if you do not take into account the fact that during this period the child must be given gentle food. According to experts, you should steam or boil dishes, and then finely grate or puree them. Berries and juices are excluded. You need to feed your baby in small portions.
Acute intestinal infections in children: prevention, medications and treatment
Summer is a time for vacations, relaxation and travel. During this period, we usually think about pleasant things: a trip to the sea, sunbathing on the beach, exciting trips and, of course, the opportunity to simply get a good night's sleep. However, we should not forget that in summer the risk of diseases, especially infectious ones, increases.
When is the risk of infection highest?
Infections await us always and everywhere, but the incidence of acute intestinal infections increases precisely in the warm season.
This is a group of diseases characterized mainly by damage to the gastrointestinal tract. Currently, about 30 of them are known, and in their prevalence they are second only to acute respiratory infections. The causative agents can be bacteria (salmonella, shigella, enteropathogenic E. coli, staphylococci) and their toxins (foodborne diseases), as well as viruses (enteroviruses, rotaviruses, astroviruses, parvoviruses) and protozoa (giardia, amoebas). In the summer, the spread of intestinal diseases is favored by high temperatures, which reduce the shelf life of products and promote the survival of pathogens in the environment; flies and other insects that can become carriers of infection; “crowding” of people - do not forget that the source of infection can be a sick or infected person without signs of illness, but who is a bacteria excretor. The main cause of acute intestinal diseases remains non-compliance with hygiene rules. That is why children are at greatest risk of infection.
Symptoms of intestinal infection in a child
Pathogens enter the human body through the mouth. Basically, all intestinal diseases occur with fairly similar symptoms and always begin suddenly. At the very beginning, you may be worried about weakness, lethargy, loss of appetite, headache, fever - these symptoms are similar to those of acute respiratory infections. Soon nausea, abdominal pain, vomiting, and loose stools appear. Among the symptoms of damage to the gastrointestinal tract, as a rule, the most pronounced symptoms are those associated with the affected organ:
- nausea, vomiting, pain in the upper abdomen - with gastritis;
- loose stools, stools with mucus, blood - with enteritis, colitis;
- vomiting and loose stools - with gastroenteritis.
Children have a number of features that contribute to the more frequent occurrence and more severe course of intestinal infections, for example: low levels of acidity of gastric juice and enzymes allow pathogens to easily pass this barrier and cause damage to the entire gastrointestinal tract; good blood supply to the intestinal mucosa and increased permeability of all barrier systems allow toxins to quickly penetrate into the blood, which leads to rapid disturbances in the regulatory systems of the whole body, disorders of the central nervous system and psyche - children become lethargic, capricious or, on the contrary, excited, as well as They may experience delirium (delirium). All these and some other features sometimes make it difficult to diagnose the disease in a timely manner.
In general, it should be said that the younger the child’s age, the higher the risk of severe disease and the greater the likelihood of complications. With the initial signs of the disease, it is difficult to assess the severity and predict the outcome. This requires dynamic observation with assessment of all symptoms of the disease. Children may “hide” their complaints out of fear and simply not differentiate pain. Therefore, if the child’s condition worsens, it is recommended to immediately consult a doctor.
Medicines for intestinal infections in children
You can alleviate the condition of a sick child, promote his rapid recovery, and also prevent the onset of the disease by doing the following before the doctor arrives:
- For heaviness in the abdomen, overeating, fatty foods, give enzymes (Creon, Mezim-Forte, Pancreatin, etc.). These medications are taken with meals or can be added to food.
- In case of vomiting, nausea, loose stools, and even if poisoning is suspected, sorbents should be given as quickly as possible - these are drugs that capture toxins, preventing them from entering the blood, and remove them from the body with feces (Smecta, Enterosgel, Filtrum, Polysorb, etc. .d.). Some of them have enveloping properties and protect the mucous membrane of the stomach and intestines (Smecta). Their disadvantage is an unpleasant taste, which is a problem when treating a child. However, some of them (Smecta) can be added to porridge or mixture. Taken at intervals of 1.5-2 hours before or after taking other medications.
- Probiotics that normalize intestinal microflora are an effective preventive agent that promotes faster restoration of intestinal microflora (Acipol, Enterol, Baktisubtil, RioFlora Immuno, etc.). At the first symptoms of the disease, they should be given 2 hours after taking the sorbent.
- If a disease occurs, accompanied by vomiting, loose stools, or fever, drinking water is mandatory. This requires a certain degree of persistence and patience on the part of the parents. The procedure should be carried out in small volumes, so as not to provoke vomiting, 5, 10, 15 ml at intervals of 10-15 minutes, until vomiting stops and stool decreases. For drinking, drinking water, weak tea, dried fruit infusion, rice infusion, and apple-raisin infusion are used. These solutions do not cause stomach irritation, contain the necessary salts and are easily absorbed.
In case of repeated vomiting and frequent stools, it is necessary to additionally supplement the child with saline solutions (Regidron, Gidrovit, etc.), because the loss of salts and water leads to significant disruptions in the functioning of organs and systems. Solutions are given fractionally, alternating with drinking, in the same volume, and if the doctor does not indicate the volume of saline solution, then drinking should be done with saline solution and drinking in a ratio of 1:3. Saline solutions should be given at room temperature to avoid causing vomiting. If mineral water is used, it must first be degassed.
Other drugs, such as antiemetics (Motilium, etc.), intestinal antiseptics (Enterofuril, etc.), etc. should be given only after consultation with a doctor, who will select the required dose. In addition, taking antiemetic drugs in the first hours of the disease is undesirable, since vomiting causes spontaneous rapid removal of the contaminated product, which will contribute to a quick recovery. Antidiarrheal drugs, such as Loperamide, are also not recommended to be given without a doctor's prescription.
Nutrition is a very important part in treating a patient with an intestinal infection. A proper diet reduces the load on the inflamed mucous membrane and organs of the gastrointestinal tract (specially selected foods are better absorbed) and contributes to the rapid recovery of the child’s body. During the acute period, the following food is recommended: slimy (boiled) porridge in water (rice, buckwheat), mashed potatoes, vegetable soups, crackers, baked apples, lean meats (turkey, beef) in crushed form (soufflé, minced meat, puree) and etc.
With the therapy, the child's condition can quickly improve. However, with symptoms such as repeated vomiting, abdominal pain, vomiting with various impurities, including blood, or “rusty” vomit (it is advisable to collect it for examination by a doctor), black or bloody stools, rare urination in small portions, You should consult a doctor immediately.
Prevention of intestinal infections in children
Considering the risk of intestinal disorders, it is recommended to take all of the above medications with you in your travel first aid kit, and also remember basic hygiene rules:
- wash your hands with hot water and soap;
- store food correctly;
- drink purified, or preferably boiled, water;
- wash all fruits, berries and vegetables eaten raw with hot water;
- do not buy products with damaged packaging or from dubious sellers;
- avoid contact with sick people (if your child is sick, try to limit contact with other people, stop visiting swimming pools and the sea, observe hygiene more carefully, because you can also be a source of infection, so do not allow the infection to spread);
- do not allow children under 3 years of age to swim in the sea (it is better to take them to the pool);
- use disinfectant wipes and gels after washing your hands (this prevents infection for a longer period).
Prognosis and prevention
Timely detection of the first signs of intestinal infection in a child and properly selected treatment can ensure a complete recovery. Usually immunity to such diseases is unstable. With the development of a severe form of the disease, complications may appear, including acute renal or heart failure, pulmonary edema and other dangerous conditions. For this reason, parents are advised not to select medications for treatment themselves, but to immediately consult a doctor.
To prevent bacterial and viral intestinal infections, the following sanitary and hygienic standards must be observed:
- teach your child the rules of personal hygiene from an early age;
- properly store and heat process food;
- Parents should always wash their hands after washing and swaddling the baby;
- Make sure that the water you drink is clean (filtration and boiling will help);
- disinfection of toys and utensils in kindergartens, which can be sources of infection;
- When breastfeeding, the mother should shower daily and change her underwear regularly to keep the mammary glands clean;
- If a child eats from bottles and sucks on a pacifier, then they also need to be regularly treated with specially designed products. This way, viruses and bacteria that cause acute intestinal infections will not penetrate the gastrointestinal tract through the objects used.
The remaining children in the family or in the child care facility where the sick child was located should be examined, and their well-being should be monitored for at least 7 days.
Etiology of acute intestinal infections
The etiology of intestinal infections is associated with the entry of the pathogen into the body. There are 3 main routes through which they enter the body:
- through food - usually through food products that have not undergone sufficient hygienic and heat treatment;
- through water - symptoms and etiology of intestinal diseases when infected through water occur when drinking low-quality water;
- during everyday contact - through various objects or dirty hands.
Bacterial acute intestinal infections are often caused by bacteria such as salmonella, E. coli, and viral ones - by the entry into the body of rotaviruses, enteroviruses, etc. Severe clinical symptoms occur with amoebiasis and giardiasis, which are relatively rare causes.
Question answer
When to call a doctor?
In this matter, parents need to focus on general well-being and characteristic symptoms indicating that the child has an acute intestinal infection. For children, especially in infancy, this disease is extremely dangerous, as dehydration rapidly develops in the body. An alarming symptom that should promptly consult a doctor is a decrease in the volume of urine and the number of urinations.
How can you tell if dehydration is developing?
The disease is most often accompanied by vomiting and diarrhea. As a result, the human body loses a lot of fluid and salts (potassium, sodium, chlorine, etc.). Dehydration develops, which is considered one of the most life-threatening situations, especially for a small child.
Parents should be very careful, especially if their child exhibits the following alarming symptoms:
- saliva has become more viscous;
- the skin has acquired a gray tint;
- the child has become more lethargic and drowsy;
- in 12 hours the baby peed twice as often as usual;
- the oral mucosa and tongue become dry;
- vomiting is so severe that the child cannot be given anything to drink;
- in a baby under the age of 1 year, the pulse quickens and the fontanel on the head begins to sink;
- The volume of urine excreted is reduced, which acquires a dark tint and a pungent odor.
In this case, the child should be taken to the clinic, where he will be given a drip so that the fluid balance in the body normalizes.
How to feed a child with an intestinal infection?
If an acute viral or bacterial intestinal infection has developed, the child should be given proper water. It is necessary to ensure that the sick person does not take large sips, as this can cause vomiting, which will lead to even greater loss of fluid. Therefore, experts recommend feeding your baby carefully and little by little.
It is better to do this every 5 or 10 minutes, 5-15 ml of water at a time. Also, you should not give your child only clean water, as this will cause a salt imbalance in the body. You can give a pharmaceutical solution for rehydration. However, if the baby refuses to drink, then you should give him any liquid he wants.
What to feed a child with an intestinal infection?
When choosing dishes, you should be guided by the fact that food should reduce inflammatory changes in the gastrointestinal tract that occurred as a result of an acute viral intestinal infection.
Basic nutritional recommendations:
- the food consumed must be warm, not higher than 38 °C;
- it is advisable to eat not 3 times, but 5-6 times a day;
- in the first days it is necessary to reduce the amount of food consumed by 15–20%;
- food should be steamed, boiled, mashed or mashed;
- you need to limit fats, carbohydrates and table salt in your diet, and introduce a sufficient amount of protein;
- dishes should be mechanically and chemically gentle, easily digestible and varied in taste.
You should also exclude from your diet foods that increase intestinal motility: packaged and freshly squeezed juices, berries, raw fruits and vegetables, fresh baked goods, legumes, as well as pure vegetable and animal oils.
Treatment of intestinal infection
The treatment tactics for intestinal infections directly depend on the type of causative agent of the disease, the severity and the presence of concomitant disorders in the body.
When treating pathology, doctors set themselves several tasks at once: to eliminate the onset of infection, prevent dehydration, relieve unpleasant symptoms and restore the normal functioning of the child’s body. For this purpose, the child is prescribed the following groups of medications:
- glucose-saline solutions for oral rehydration;
- antibiotics (for bacterial forms of the disease);
- antifungal drugs (for fungal infections);
- intestinal antiseptics;
- antipyretics;
- sorbents to prevent intoxication of the body.
In addition to drug therapy, parents need to provide the patient with dietary nutrition that is gentle on the child’s stomach and intestines.
Heavy foods can aggravate the condition and delay recovery. In case of an intestinal infection, it is necessary to reduce the amount of food consumed, drink plenty of water, and give preference to pureed or liquid easily digestible food. Fatty, fried, smoked and highly salted foods, fatty meats, fruits, dairy products, juices and carbonated drinks are excluded.