Any discomfort or pain in the abdomen is a reason to consult a doctor, especially if these manifestations are accompanied by symptoms such as abnormal stool, the presence of impurities in it (mucus, pus, blood). In some cases, already during the examination, all of the above complaints may indicate the development of sigmoiditis (ICD code 10 - K 52).
Sigmoiditis
Causes of inflammation of the sigmoid colon
First of all, mention should be made of the anatomical specificity of this section of the intestine. Its name itself indicates these features. The shape of the sigmoid colon resembles the English letter “S”, which, naturally, creates difficulties with the movement of digested food through it.
Prolonged presence of feces in the intestinal lumen will cause microtraumatic damage and irritation of its wall. All this, together with the active bacterial flora of the large intestine, is “fertile ground” for future inflammation.
Causes of sigmoiditis also include:
- bacterial infections: amoebiasis, dysentery, salmonellosis. Certain forms of these diseases occur with ulceration or the formation of erosions on the mucous membrane, where microorganisms subsequently enter and inflammation begins;
- chronic diseases of the gastrointestinal tract, with predominant damage to the large intestine. They are UC (nonspecific ulcerative colitis), Crohn's disease and other diseases, the leading role in the occurrence of which does not belong to bacteria. In some cases, they have a hereditary predisposition to development or arise as a result of improper immune reactivity of the body;
- dysbacteriosis;
- atherosclerosis of mesenteric vessels. It leads to disruption of the normal blood supply to the intestines, so the wall of the sigmoid colon becomes even more vulnerable to bacterial infections. The regeneration of microtraumas slows down, areas of necrosis (death) may appear, on which bacteria successfully reproduce;
- radiation sickness;
- pregnancy. The expectant mother may experience compression of the intestine by the growing fetus, which, together with constipation, will cause inflammation.
In some cases, the pathological inflammatory process does not occur in the sigmoid colon itself, but in other parts of the large intestine, and only then spreads to it. If the process spreads upward, then the disease will be called Rectosigmoiditis, since the rectum will also be affected.
Classification
Depending on the degree of activity and duration of existence, inflammation can occur as follows:
- acute sigmoiditis;
- or chronic sigmoiditis.
Based on the nature of the inflammatory changes occurring in the intestinal wall, the following are distinguished:
- catarrhal sigmoiditis. With it, the lesion does not extend deeper than the epithelial, that is, the uppermost mucous layer of the sigmoid colon;
- erosive sigmoiditis. It may transform into the previous form if treatment was not prescribed in a timely manner. On the intestinal wall, in addition to signs of catarrhal inflammatory process, instrumental examination will reveal erosions;
- The ulcerative form of sigmoiditis is characterized by deepening inflammatory damage. The changes affect not only the upper mucous membrane, but also the submucosal layer, and in severe forms even move to the muscular layer;
- the last and most severe form will be Perisigmoiditis. The outcome of this type of inflammation can be an extensive adhesive process, because the intestinal wall is completely affected.
Sigmoiditis is also necessarily classified according to its effect on the motor-evacuation function of the intestine. Highlight:
- spastic sigmoiditis;
- paralytic sigmoiditis.
When formulating a diagnosis, the doctor must describe all the signs that characterize the sigmoiditis of a particular patient. This will immediately give all other specialists an understanding of the degree of intestinal damage, the severity of the disease, and will also indicate the possibility of prescribing certain medications.
Kinds
Like most inflammatory diseases, sigmoiditis can be acute or chronic. In addition, there are the following types, differing in the nature of intestinal damage:
- Catarrhal sigmoiditis. The mildest form, in which only the upper layer of the intestinal epithelium is damaged.
- Erosive sigmoiditis. It is a continuation of untreated catarrhal disease and is characterized by the destruction of the intestinal epithelium with the formation of erosions on it - open, unprotected areas of the mucous membrane.
- Ulcerative sigmoiditis. This form appears with prolonged irritation of erosions on the surface of the intestine, as a result of which they turn into ulcers - deeper defects of the mucous membrane.
- Perisigmoiditis. It is the most severe form of the disease. Through the ulcerative surface, inflammation penetrates into the deep parts of the intestinal wall, reduces its mobility, and the adhesive process begins in the abdominal cavity (the process of connecting intestinal loops to each other).
Symptoms of Sigmoiditis
The clinical symptoms of sigmoiditis will vary greatly from patient to patient. Even the medical history of the same person at different periods of life can vary: the past exacerbation may be barely noticeable, but the current one may have a vivid clinical picture.
Among all the clinical manifestations, three main ones can be distinguished, present in almost any patient with Sigmoiditis:
- pain;
- change in stool;
- general manifestations.
If we talk about pain, its localization is the same - the iliac region on the left (below, above the pelvic bones). More often the pain is intense, radiating to the leg and/or lower back. Sigmoiditis during pregnancy can occur with an atypical location of pain. Another similar displacement in a small number of cases is observed in people who have previously undergone operations on the intestines, and there is an adhesive process, as well as in patients who are short or, conversely, tall.
In patients with Sigmoiditis, the stool is often relaxed (diarrhea), and they are much less likely to be bothered by a tendency to constipation. Depending on the form of the lesion, pathological impurities may be detected in the stool. Naturally, with the catarrhal form of the disease, mucus may appear in the stool, and with ulcerative or, less commonly, erosive sigmoiditis, blood or pus.
Crohn's disease. Chronic intestinal inflammation
How to treat the intestines and thereby get rid of many
How to treat the intestines. A proven way to heal your intestines.
How to treat the intestines and thereby get rid of many
Official group of Nadezhda Kolesnikova: https://vk.com/koles
Intestinal restoration session. Nadezhda Kolesnikova
Official group of Nadezhda Kolesnikova: https://vk.com/koles
Cette vidéo présente les étapes d'une Sigmoidectomie Laparoscopique «Colectomie Gauch
Sigmoidectomie Laparoscopique pour Sigmoidite : Dr Mustapha OUALI
Cette vidéo présente les étapes d'une Sigmoidectomie Laparoscopique «Colectomie Gauch
Colorectal surgeon Marat Khaikin in front
Inflammatory bowel diseases.mp4
Colorectal surgeon Marat Khaikin in front
Changes in general condition rarely accompany catarrhal focal sigmoiditis. The larger the affected area, the more severe they can appear. In addition, pathology is more often caused by a general change than a subacute course. Among the general complaints, patients indicate increased fatigue, weakness, decreased body weight, decreased performance, and in some cases, sleep disturbances.
Publications in the media
Diverticular disease is a disease characterized by the formation of diverticula in the intestinal wall; the development of diverticulosis (multiple diverticula) and diverticulitis is possible (see Diverticular disease).
The incidence of diverticular disease of the colon reaches 20% in the population; the frequency increases with age, reaching 40–50% among patients 60–80 years old. The predominant age is 60–80 years. It rarely occurs before age 40.
Classification • Colon diverticula. More frequent damage to the left half of the colon is explained by its anatomical and functional features - smaller diameter, a large number of bends, denser consistency of the contents; the sigmoid colon has a reservoir function, so the pressure in it is higher • Diverticula of the small intestine are less common than diverticula of the large intestine. Diverticula of the duodenum occur more often (see Diverticula of the stomach and duodenum), mainly in its distal section. In 3% of cases, diverticula of the duodenum are combined with diverticula of the jejunum and ileum.
The etiology is largely controversial; the occurrence of the disease is due to a combination of factors rather than the action of one of them • The hernia theory is one of the most common. The cause of the formation of protrusions is considered to be weakness of the connective tissue framework of the intestinal wall, which develops as the body ages. Impaired intestinal motor function, also characteristic of an aging body, leads to an increase in intestinal pressure and protrusion of the mucous membrane in places of least resistance. The highest intraintestinal pressure occurs in the narrowest part of the colon - the sigmoid. For this reason, diverticula are more likely to form there. The proximity of blood vessels explains the tendency of diverticula to bleed • Vascular theory. The main reason for the appearance of diverticula is changes in the intestinal wall due to circulatory disorders • Theory of congenital predisposition • Mechanical, or pulsation, theory. With increased activity of the smooth muscles of the intestinal wall, excessive segmentation of the intestine occurs, leading to an increase in intraintestinal pressure in certain areas. Under the influence of high pressure, the mucous membrane protrudes through the muscle membrane.
Genetic aspects - see Diverticular disease.
Risk factors for developing diverticular disease • Age over 40 years • Diet low in plant fiber.
Risk factors for diverticulitis • History of diverticulitis • Multiple colonic diverticula.
Clinical picture • Diverticulosis without clinical manifestations • Diverticulosis with clinical manifestations is characterized by abdominal pain, bloating, unstable stool (alternating constipation, diarrhea and normal stool) • There are uncomplicated and complicated diverticulosis •• The clinical picture of uncomplicated diverticulosis is characterized by periodic abdominal pain, bloating , unstable stool (alternating constipation, diarrhea and normal stool) •• Diverticulosis with a complicated course (see Complications).
Concomitant pathology. Colitis, dysbacteriosis.
Age characteristics • Children. Diverticular disease occurs very rarely; complications of Meckel's diverticulum are more common • Elderly. Occurs most often, diagnosis is difficult due to the large number of concomitant diseases.
Complications of diverticulosis
• Diverticulitis occurs in approximately 25% of patients with diverticulosis. Main signs •• Acute onset - pain and tension in the muscles of the anterior abdominal wall in the left lower quadrant of the abdomen •• As the disease progresses - increased body temperature, chills •• Anorexia, nausea, vomiting •• Diarrhea or constipation •• Painful dense sedentary infiltrate in the abdominal cavity (when the inflammatory process spreads from the diverticulum to the surrounding tissues) •• When the bladder is involved in the process - dysuria.
• Perforation •• When the diverticulum is perforated into the abdominal cavity, a clinic of diffuse peritonitis develops •• When the diverticulum is perforated into the retroperitoneal tissue or the space between the layers of the mesentery, infiltrates or abscesses occur •• With the slow progression of inflammation, the serous membrane adheres to the surrounding organs, covered perforation occurs •• Development peritonitis can be associated not only with perforation of the diverticulum, but also with abscesses that arise in the thickness of the intestinal wall, with inflammation and swelling of the neck of the diverticulum with its blockage.
• Bleeding •• Occurs in 20–25% of cases, often the first and only manifestation of the disease •• Bleeding is usually associated with ulceration of the neck or wall of the diverticulum and the vessel passing there as a result of chronic inflammation or the formation of a bedsore at the site of the fecal stone •• Bleeding from a non-inflamed diverticulum can occur in patients with essential arterial hypertension, atherosclerosis, heart disease, blood diseases, diabetes and with long-term use of GCs •• The volume of blood loss varies: a slight admixture of blood in the stool (sometimes hidden bleeding), massive profuse bleeding, accompanied by collapse and sometimes leading to death.
• Intestinal obstruction •• The cause of intestinal obstruction can be an inflammatory infiltrate that compresses the intestine, an adhesive process leading to deformation of the intestine and its mesentery, in some cases - intussusception of a part of the intestine with a diverticulum or spasm of smooth muscles •• Intestinal obstruction with diverticulosis is often obstructive in nature with all the manifestations inherent in this form.
• Internal or, less commonly, external intestinal fistulas •• In men, sigmo-vesical fistulas more often develop, in women - sigmo-vaginal fistulas •• When internal fistulas form, a complex system of fistulous tracts can form, opening onto the skin of the anterior abdominal wall •• When intestinal - vesical fistula - pneumaturia, fecaluria.
• Diverticula of the small intestine can lead to the development of malabsorption syndrome due to excessive growth of bacterial flora.
Laboratory tests • With diverticulosis, the number of leukocytes in the peripheral blood usually remains within normal limits; with diverticulitis, a shift in the leukocyte formula to the left and an increase in ESR often occur • With bleeding, IDA develops • In the urine, leukocytes, erythrocytes, and components of intestinal contents can be detected; when an intestinal-vesical fistula is formed, bacteria specific to the intestine are found in the urine • Coprological examination data confirming the presence of inflammation: neutrophilic leukocytes, an admixture of a large number of macrophages, desquamated epithelium in the mucus.
Special studies • Contrast X-ray examination. Traditional irrigography or colonoscopy is considered the most valuable diagnostic test for diverticulosis. In case of complicated diverticulosis, in the first 1–2 weeks the examination is limited to sigmoidoscopy and colonoscopy only. If diverticulitis is suspected, a water-soluble X-ray contrast agent (for example, gastrografin) can be used • Colon diverticula can also be detected with an oral contrast study 24–72 hours after ingestion of a barium suspension • Plain radiography of the abdominal organs in horizontal and vertical positions - in case of perforation diverticulum and peritonitis • Colonoscopy can identify the source of intestinal bleeding. Characteristic endoscopic signs of diverticulosis •• The presence of single or multiple diverticulum orifices (holes) in the intestinal wall •• Often a blood vessel is found near the mouth of the diverticulum •• In the area of the diverticulum - increased tone and rigidity of the intestinal wall; when the diverticulum is close to the physiological sphincters, the latter are spasmodic and open with difficulty •• Sometimes you can observe the discharge of pus from the mouth of the diverticulum • CT is used in the acute stage of the disease to assess the condition of the intestinal wall and peri-intestinal tissues. If there are signs of acute pathology, CT is a more preferable diagnostic method than irrigography • Cystoscopy and cystography are indicated for the diagnosis of vesicointestinal fistulas • Intravenous urography allows us to establish possible involvement of the ureters in the inflammatory process • Angiography is a diagnostic method used for bleeding from a diverticulum; it is possible to carry out therapeutic measures through embolization of a bleeding vessel • Fistulography is used in the development of intestinal fistulas to establish their connection with the intestine.
TREATMENT
Regimen • For diverticulosis with clinical manifestations, but without intoxication, symptoms of peritoneal irritation, leukocytosis, outpatient observation and treatment is possible • For diverticulosis with a complicated course, inpatient treatment in a specialized department (coloproctology) is indicated • For diverticulitis, restriction of physical activity is necessary.
Diet • All patients with diverticulosis are recommended to eat a diet with a high content of plant fiber • Wheat bran significantly reduces intracavitary pressure and accelerates the rate of migration of intestinal contents, with coarsely ground bran having a greater effect • It is necessary to exclude products that cause flatulence (legumes, grapes, lentils , onions) and constipation (blueberries, rice). You should also exclude seeds, fruits with a large number of grains and excessively coarse fiber (persimmons, pineapples, turnips, radishes, radishes).
Management tactics • In case of asymptomatic intestinal diverticulosis, detected by chance, there is no need for special treatment. A diet rich in plant fiber is recommended in order to prevent further progression of the disease and prevent possible complications • For diverticulosis with pronounced clinical manifestations, a complex of therapeutic measures is used: a laxative diet, antispasmodics, drugs that regulate intestinal motor function, and agents that normalize the composition of the intestinal bacterial flora. In most patients with clinically significant diverticulosis of the colon, conservative treatment gives a lasting effect • For diverticulitis, the use of NSAIDs, antibiotics, intestinal antiseptics, and agents that restore normal intestinal microflora is indicated • If bleeding from a diverticulum develops, the introduction of vasopressin through a catheter during selective angiography is indicated • When solving The question of the need for surgical treatment is guided by the clinical picture and the combination of risk factors.
Indications for surgical treatment: •• Complications of diverticulosis that pose an immediate threat to the patient’s life - perforation of the diverticulum into the abdominal cavity with the development of diffuse peritonitis, intestinal obstruction, massive bleeding •• Presence of fistulas •• Formation of chronic infiltrates simulating a tumor •• Frequent exacerbations of chronic diverticulosis •• Currently, surgical treatment is increasingly used for uncomplicated but clinically significant diverticulosis that is not amenable to complex conservative treatment.
Drug therapy • Diverticulosis •• Antispasmodics (papaverine hydrochloride 2% solution 1–2 ml subcutaneously or intramuscularly, bencyclane 0.05 g intramuscularly or drotaverine 2% solution 2–4 ml intramuscularly ) for pain •• Pyridostigmine bromide 0.06 g 1–3 times a day orally or 2–5 mg subcutaneously or intramuscularly; metoclopramide 10 mg 3 times a day orally (before meals) or intramuscularly - to enhance gastric and intestinal motility •• Escherichia coli, bifidobacterium bifidum or bificol - if dysbacteriosis is detected to restore normal intestinal microflora •• Vaseline or olive oil orally or in microenemas - for persistent constipation • Diverticulitis •• During the period of acute diverticulitis, it is recommended to prescribe antibiotics or •• 5-hydroxyquinoline derivatives (chloroquinaldol) •• NSAIDs •• Escherichia coli, bifidobacterium bifidum or bificol - if dysbiosis is detected • Alternative drugs. Tobramycin and metronidazole, third generation cephalosporins.
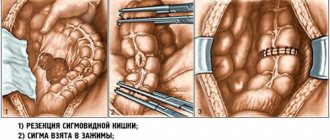
Surgery
• The choice of surgical method in each specific case depends on the following factors: •• The nature of complications and the extent of the process •• Inflammatory changes in the tissues of the diverticulum, intestinal wall and surrounding tissues •• The presence of perifocal inflammation or peritonitis •• Concomitant diseases, often observed in patients, are of no small importance elderly people.
• It is preferable to perform a planned resection of the colon with simultaneous anastomosis. The operation is performed approximately 6–12 weeks after an acute attack of diverticulitis has resolved.
• Colon fistulas in patients with diverticular disease are subject to surgical treatment, because. in most patients, independent healing does not occur and chronic inflammation in the surrounding tissues leads to the development of chronic intoxication; when intestinal-vesical fistulas form, there is a threat of developing an ascending urinary tract infection •• Surgical interventions in patients with complex fistulas (having several fistula tracts, including those that end blindly) in the presence of parafistular cavities are advisable to be carried out in several stages, which allows to reduce mortality and reduce the frequency of fistula recurrences.
• In case of profuse bleeding, it is necessary to perform a hemicolectomy, most often left-sided •• The issue of applying a primary anastomosis should be decided individually, based on the general condition of the patient, the severity of anemia, and the quality of preoperative preparation of the colon.
• The choice of surgery for intestinal perforation due to acute diverticulitis should be strictly individual •• Resection of the sigmoid colon with primary anastomosis is the most effective method of treatment in the event of local limited abscesses. The presence of a limited abscess is not considered a contraindication for the imposition of a primary anastomosis, if the sections of the intestine involved in the anastomosis are not involved in the inflammatory process and there is no immunodeficiency state •• Resection of the sigmoid colon with the imposition of a primary anastomosis and removal of a unloading colostomy of the proximal part of the anastomosis (for example, transversostomy) • • Resection of the segment of the sigmoid colon involved in the pathological process with removal of the end colostomy and suturing of the distal segment of the intestine (Hartmann-type operation). After the inflammatory process subsides (usually after 2.5–3 months), a reconstructive operation is performed to restore the anatomical continuity of the large intestine •• Application of a unloading double-barreled transversostomy and drainage of the abscess cavity (necessarily with a “spur” and intersection of both ends of the intestine).
Outpatient observation • Clinical observation with a coloproctologist at the clinic • Irrigography, colonoscopy every 3 years for diverticulosis with clinical manifestations • If there is a persistent frequency of relapses of diverticulitis, anti-relapse courses of treatment are indicated.
Course and prognosis • The prognosis for diverticular disease in most cases is favorable, but in some situations it can lead to the development of severe and life-threatening complications. This can be explained not only by the severity of the complications themselves, but also by the predominant impact on older people, who often have concomitant diseases, as well as lower body resistance in this age group • 33% of patients experience relapses of the inflammatory process • On average, 20% of patients with diverticulosis complicated bleeding, repeated bleeding occurs after several months or years.
Prevention. Prevention of constipation: adherence to nutrition and diet, active lifestyle, exercise therapy, massage.
ICD-10 • K57 Diverticular disease of the intestine.
Diagnostics
First of all, at the appointment, the doctor will conduct a detailed examination and questioning. The collected information will help determine further diagnostic tactics.
General examinations are mandatory: blood test, urine test, biochemical study, as well as coprogram. In any form of sigmoiditis, the intestines are first examined using the digital method, and after sigmoidoscopy. Only if these methods do not provide a complete picture, colonoscopy or irrigoscopy is prescribed, the indications and contraindications for which are determined by the doctor on an individual basis.
Treatment of Sigmoiditis
Treatment of any sigmoiditis should begin with lifestyle correction and diet. In some cases, this makes it possible to reduce clinical manifestations without even using drug treatment. Sigmoiditis “responds” well to the exclusion of fried, hot, spicy foods from the diet. Alcohol and rough food are strictly contraindicated. During an exacerbation, a person should consume all foods in crushed form, and if there is Perisigmoiditis, then in a mushy form.
You should not eat a lot at one time, it is better to do it more often, maintaining the required calorie content of the diet and its balance in fats, carbohydrates and proteins. The latter are especially important in any inflammatory reactions for the normal course of regenerative processes. As the inflammation subsides and the patient’s general condition improves, the diet for Sigmoiditis expands, however, in order to avoid another exacerbation, its basic principles should be adhered to constantly.
Drug treatment and symptoms of Sigmoiditis will be inextricably linked. The more pronounced the clinical picture, the longer and more complex therapy a person needs. Currently, high-quality and good modern drugs are available for the treatment of any Sigmoiditis. The main thing is to correctly find out the root cause of the disease and determine its form.
If the pathology is provoked by infectious agents, then treatment of sigmoiditis consists of prescribing antibiotics: Biseptol, Ampicillin, Tetracycline. In parallel with antibacterial drugs, the treatment plan includes drugs for the treatment and prevention of dysbacteriosis: Bifidobac, Hilak Forte, etc.
What do the organs of the body look like?
When the inflammation is nonspecific, anti-inflammatory intestinal drugs are prescribed: Sulfasalazine, Salazoperidazine, etc. In each case, the doctor selects treatment individually, as well as the necessary therapeutic dosage.
If there is a significant change in the general condition, hospitalization in a hospital and the administration of infusion therapy may be recommended, and in severe forms, even the administration of drugs for parenteral nutrition.
In any case, the next exacerbation, not to mention the initially appearing symptoms of the disease, indicating sigmoiditis, is a reason to consult a gastroenterologist or therapist. It is these specialists who, having carried out the diagnosis, will prescribe the necessary drug treatment; in addition, only a doctor can correctly answer the question of what enemas should be done for Sigmoiditis.
As with any other inflammatory process, with inflammation of the sigmoid colon, excessive outside intervention can only cause harm. Only the treating doctor, who is aware of the intricacies of your pathology, will correctly answer the question about treatment tactics.
Stages of the disease
It is possible to make a diagnosis and determine the degree of progression of dolichosigma only after a comprehensive examination.
Dolichosigma has 3 stages - in accordance with the severity of constipation and manifestations:
- Compensated. Constipation occurs rarely, mainly due to errors in nutrition. The x-ray shows elongation of the sigmoid intestine. Pain occurs with constipation and goes away after defecation. There are no changes in physical development - the abdomen is not increased in volume.
- Subcompensated. Characterized by constipation that lasts up to two days. Stool passage occurs independently and in large quantities. If there is a deficiency of plant fiber in the child’s diet and dense foods predominate, then constipation will be more pronounced. In this case, frequent bowel movements are observed, which are accompanied by flatulence. A characteristic feature is bloating in the lower part of the abdomen and an increase in its size.
- Decompensated. Accompanied by almost daily constipation. The stool does not pass until 4-5 days. In this case, there is severe pain in the abdomen and bloating. Possible vomiting. The physical development of the child suffers.
There are different forms of dolichosigma: acute and chronic. During periods of exacerbation, constipation is prolonged (lasts 3-5 days). In this case, intoxication of the body is observed, and concomitant diseases develop. In the chronic form, constipation becomes a constant problem. Severe pain and intoxication appear.
Depending on the etiological (causal) factor, congenital and acquired dolichosigma are distinguished. Congenital occurs genetically or develops in the womb. Acquired disease develops due to the influence of various factors, external and internal.
Non-drug therapy and treatment with folk remedies
As with any other Colitis, with inflammation of the sigmoid colon, physiotherapy can be used. Naturally, it is indicated during the rehabilitation period or when the clinic subsides. In some cases, physical therapy helped reduce the duration and volume of supportive drug therapy. This was especially true when physiotherapy was prescribed to a child or when the inflammatory process was mildly active in an adult.
How sigmoiditis is treated can also be found out on various forums. Quite often in the discussion there are comments and practical reviews about certain medications, as well as advice on how to carry out treatment using traditional methods.
In pharmacies you can purchase ready-made herbal mixtures recommended for diseases of the gastrointestinal tract, or create a mixture yourself. As a tea for sigmoiditis, you can use chamomile, celandine, dill seeds or rose hips.