Gastric outlet stenosis is a narrowing of its lumen in the area of the pylorus and/or the initial part of the duodenum, in which the evacuation of contents from the stomach is impaired. In children, the most common cause of gastric outlet stenosis is a secondary peptic ulcer of the antrum, which occurs when foreign bodies, caustic substances, nonsteroidal anti-inflammatory drugs (NSAIDs) enter the body and due to inflammatory diseases such as Crohn's disease and tuberculosis. Idiopathic causes (peptic ulcer, hypertrophic pyloric stenosis, prepyloric membrane, annular pancreas) and postoperative (scarring, anastomotic stricture) are less common [1-4].
Disorders of homeostasis, especially water-electrolyte balance, and the nutritional status of the child determine the importance of early diagnosis and surgical treatment [5]. Traditional methods of surgical correction (gastric resection, gastroenterostomy, selective vagotomy in combination with stomach drainage operations) are highly invasive organ-removing interventions and require wide access, significant anesthetic support, the use of fluoroscopic control, a long postoperative recovery period - all this places additional stress on the body of a sick child [6-9].
The method of step-by-step endoscopic balloon dilatation (a method of restoring the lumen using a special balloon made of durable plastic, which is inflated inside the narrowed area) does not have these disadvantages and has a number of advantages. From the point of view of resource costs, it is economically beneficial - a shorter duration of general anesthesia compared to surgical correction, the use of reusable balloon dilators, and a reduction in the length of the hospitalization period. Technically, special equipment is required, but it is reusable, and there are no complications associated with surgical intervention; a room for gastroscopy or any other endoscopic procedures is suitable for carrying out, and the equipment is adapted for mobile transportation from one room to another, which is very convenient within the same or neighboring departments, since it allows optimizing the work time of doctors and reducing the waiting time of patients [10, 11] . Performed by an endoscopist surgeon. The result is the most physiological and anatomical restoration of the gastrointestinal passage and improvement of the child’s quality of life without severe organ-removing surgery.
Endoscopic balloon dilatation is widely used for esophageal stenosis in children and adults [10, 11]. The method is used for cicatricial pyloric stenosis in adults [12–24], but in children there is insufficient experience [1, 7, 25]. Modern literature provides individual clinical observations of the use of the method for pyloric stenosis in children. In a study by A. Temiz et al. [26] presented a retrospective analysis of 14 patients (9 boys and 5 girls aged 3.4±1.7 years) who were diagnosed with pyloric stenosis from August 2003 to August 2011. Upon admission, all patients complained of vomiting. In 8 children, caustic substances entered the body through the mouth, in 2 children a previously diagnosed peptic ulcer was diagnosed, and in 4 children there was no significant medical history. X-ray examination with contrast agent and endoscopy revealed pyloric stenosis in all patients. Endoscopic balloon dilatation was tried in 12 patients; 8 patients required surgical correction of pyloric stenosis; in 6 patients, the complaints resolved after balloon dilatation of the pylorus. The researchers conclude that although endoscopic balloon dilatation is an established treatment for benign pyloric stenosis in adults, there is little experience with this technique in children, who can be effectively and successfully treated without surgery.
In the work of H. Heymans et al. [27] described the use of balloon dilatation as a treatment for pyloric obstruction in 2 children after inadequate pyloromyotomy and in an 11-year-old boy with surgical damage to the vagus nerve. Successful balloon dilatation is considered by the authors to be a good alternative to surgical treatment in these conditions.
In the work of D. Gobbi et al. [28] presented a case of a previously healthy 3-year-old boy who developed severe chronic pyloric obstruction and antral stenosis after short-term administration of liquid ibuprofen at a dose not considered to be associated with adverse effects. The authors report rapid and successful endoscopic treatment of established conditions using pneumatic balloon dilatation, but note that the benefits of such treatment remain to be proven.
Taking into account the etiology, pathogenesis of diseases, anatomical (the length of the pyloric part of the stomach, the thickness of its wall, the abundance of blood supply to the mucous membrane), physiological (features of the rhythm of peristalsis and gastric secretion), functional (motility activity, the speed of passage of food through the corresponding parts of the stomach) and other features In a growing organism, it is impossible to project the results of using the method in adults onto children.
Using the example of two clinical cases, it is shown that staged endoscopic balloon dilatation of the pylorus is devoid of most of the listed problems and disadvantages and allows the most effective restoration of gastrointestinal passage and improve the child’s quality of life.
Boy A
., 5 years old, was admitted to the surgical department of the National Medical Research Center for Children's Health (NMRCHD) in July 2022 with complaints of recurrent pain in the epigastric region with occasional nausea, vomiting, weakness, and weight loss.
From the anamnesis it is known that the disease began on 03/06/17 with repeated vomiting of eaten food, followed by vomiting in the form of coffee grounds. The fact of injury or infectious disease is denied; after the first episode of vomiting, he took ¼ tablet of citramon.
When contacting the Republican Scientific Center for Emergency Medical Care in one of the Central Asian republics, the child was hospitalized in the surgical department, where, based on the results of fibroesophagogastroduodenoscopy (FEGDS), a diagnosis was made: gastric ulcer. Callous (giant) ulcer of the antrum of the stomach. Mild protein-energy deficiency. The edges of the ulcer were injected with adrenaline, anti-ulcer therapy was prescribed and surgery was proposed, which the parents refused. Against the background of anti-Helicobacter therapy prescribed on an outpatient basis, nausea and vomiting began, the parents stopped giving the drugs on their own, after a short improvement in the condition, uncontrollable vomiting began, the child was readmitted to the hospital. FEGDS and X-ray of the stomach revealed cicatricial ulcerative pyloric stenosis in the compensation stage; diet and conservative antiulcer therapy were recommended. The family history is burdened: the uncle underwent surgery for duodenal ulcer. After performing double balloon dilatation of the pylorus in Germany (from December 18 and 21, 2017) to a diameter of 10 mm, free passage with the endoscope was not possible.
Objectively: general condition of moderate severity, clear consciousness, active position, correct physique, low nutrition, no peculiarities in organs and systems.
Laboratory parameters (clinical blood test, general urine test, stool test, biochemical blood test) are normal. Ultrasound examination of the abdominal cavity did not show any abnormalities. Endoscopy on July 8, 2022 revealed a pronounced circular, nonspecific cicatricial pyloric stenosis with a residual lumen of 3 mm against the background of a rather hard scar formation approximately 1.5 mm deep, impenetrable to the endoscope. Conclusion: severe cicatricial pyloric stenosis; condition after double balloon dilatation of cicatricial pyloric stenosis.
Taking into account age, medical history, general and somatic condition, results of laboratory and instrumental studies, and with the consent of the parents, a decision was made to conduct experimental balloon dilatation therapy for the pylorus of the stomach. As part of subsequent gastroscopy on July 14 and 18, 2022, staged endoscopic balloon dilatation of the pylorus was performed, guided by a guide wire, to a maximum balloon diameter of 12 mm (Fig. 1-3).
Rice. 2. Balloon dilatation (endophotography).
Rice. 3. Pylorus after balloon dilatation sessions (endophotography).
Rice. 1. Pylorus before balloon dilatation (endophotography).
At the end of the intervention, a short-term examination of the duodenal bulb became possible - no pathological changes were detected. Conclusion of the control endoscopy dated July 19: condition after balloon dilatation of the pylorus. antral gastritis. Diagnosis: cicatricial stenosis of the pylorus. Condition after double balloon dilatation of pyloric stenosis.
It is recommended to continue local dilatation therapy at the end of 2022 to maintain and improve the positive result and prevent recurrence of stenosis. The postoperative period lasted 2 days, without complications, analgesic, antisecretory, antacid therapy with a positive effect. There was no nausea or vomiting, the child recovered quickly and felt well. He was discharged home with recommendations to continue observation and treatment by a gastroenterologist, and to be hospitalized in the surgical department at the end of 2022 to monitor the result and possible repeat dilation therapy.
Boy B
., 2 years 10 months. From the anamnesis it is known that the disease began on 09/01/18 with the appearance of loose stools and fever up to 38 °C. He received treatment with ibuprofen and paracetamol. On the third of September, vomiting appeared without impurities, and then in the form of coffee grounds, pain in the abdomen, and loose black stools. He was urgently hospitalized in the Central District Hospital of one of the cities of the Moscow region in serious condition (Hb 69 g/l, er. 2.54∙1012/l). Endoscopy: acute pyloric ulcer, bleeding from the ulcer (Forrest 2B). Coagulation endohemostasis was performed. An endoscopy on September 12 revealed a gastric ulcer in the scarring stage. After consultation with a gastroenterologist, he was discharged home in satisfactory condition. I received esomeprazole 10 mg 2 times a day, aluminum phosphate ½ packet 3 times a day, domperidone 5 ml 3 times a day. However, on September 17, a single vomiting with streaks of blood was observed again, and therefore he was hospitalized in the Morozov Children's City Clinical Hospital, where an endoscopy revealed cicatricial ulcerative stenosis of the pylorus; the pylorus was impassable for an endoscope with a diameter of 5 mm.
In October 2022, he was hospitalized in the surgical department of the National Medical Research Center for Children with Complaints of the inability to eat solid food and an episode of blood in the stool.
Objectively: general condition is moderate, consciousness is clear. Reduced nutrition, harmonious physical development. He absorbs the enteral load and does not vomit. There are no peculiarities on the part of organs and systems.
Clinical blood test: mild anemia (Hb 94 g/l, Ht 29%), general urine test, stool test, biochemical blood test are normal.
Endoscopy was performed. Esophagus: the lumen is preserved, expands freely during insufflation, a large amount of gastric contents in the lumen, the mucous membrane in the upper and middle third is pale pink, in the lower third it is hyperemic, the dentate line is blurred, generally corresponds to the esophagogastric junction, vascular pattern in the upper and the middle third can be traced, the lower third is blurred, the cardia closes, peristalsis is moderately reduced (study under general anesthesia). There is a large amount of turbid contents in the lumen of the stomach (the study was continued after sanitation of the stomach). The mucous membrane in the antrum is swollen, hyperemic, loose, the vascular pattern is blurred. The pyloric lumen is narrowed, visually about 3-4 mm, impassable for an endoscope with an outer diameter of 5.9 mm.
After preliminary preparation, a diagnostic colonoscopy was performed (to exclude Crohn's disease, since a single episode of blood in the stool was noted), no signs of ongoing bleeding were detected, and moderately severe lymphoid hyperplasia of the colon was detected. Based on the results of a morphological study, Crohn's disease was excluded.
Due to severe pyloric stenosis and the inability to eat solid food, a decision was made to perform a series of planned endoscopic balloon dilatations of the pylorus. During the first session of balloon dilatation (October 15), under endoscopic control, a balloon catheter was inserted through the guide wire through the working channel of the endoscope into the area of the narrowed pylorus. The catheter was sequentially insufflated with distilled water up to 10 mm under a pressure of 3 atm, then up to 12 mm under a pressure of 8 atm with an exposure time of 120 s, after which the balloon was completely deflated and removed. The site of dilatation was irrigated with dexamethasone solution. During the control endoscopy, linear ruptures of the mucous membrane in the area of dilatation were revealed, the pyloric lumen was about 6 mm, passable for an endoscope with an outer diameter of 5.9 mm, there was no active bleeding. During the second session of balloon dilatation (October 22), the same actions were performed with the balloon inflated to 15 mm under a pressure of 8 atm, exposure time 120 s (Fig. 4-6).
Rice. 5. Balloon dilatation. Balloon catheter in the pyloric lumen (endophotography).
Rice. 6. Condition after the second session of balloon dilatation. The pylorus is passable for a 5.9 mm endoscope. Linear breaks in the mucous membrane are visible (endophotography).
Rice. 4. Condition before balloon dilatation sessions: the pylorus is narrowed to 3 mm (endophotography).
The course of the postoperative period is smooth. Conclusion of the control endoscopy dated October 25: condition after balloon dilatation of the pylorus. Common gastritis. Duodenitis. The pylorus is passable for a 5.9 mm endoscope. The absorption of enteral load was clinically improved, and it became possible to take solid food in a small volume.
Diagnosis: cicatricial ulcerative pyloric stenosis as a result of NSAID gastropathy. Condition after double balloon dilatation of cicatricial pyloric stenosis. Anemia of mixed origin, mild severity.
The child received parenteral nutrition, medicinal formula for enteral nutrition, esomeprazole per os
, then intravenously, antibacterial and symptomatic therapy in the postoperative period, antacids, domperidone, vitamin D3. Upon discharge, observation by a surgeon and gastroenterologist, endoscopic monitoring of the result after 3 months, and the use of antipyretic drugs rectally or parenterally if the body temperature rises above 38.5 °C are recommended.
Acute dilatation of the stomach in humans: what is it?
Acute dilatation of the stomach belongs to the category of uncommon diseases of this organ and the gastrointestinal tract as a whole. On the other hand, at its first signs, clinical alertness should arise, since the consequences of the described disease can be severe and lead to critical consequences.
Males get sick more often than females. But women often suffer from acute dilatation of the stomach more severely.
note
If acute dilatation of the stomach is diagnosed in childhood or adolescence, this indicates some kind of disturbance in the intrauterine development of the fetus.
Causes of acute gastric dilatation
Acute dilatation of the stomach is a polyetiological disease - this means that its occurrence is provoked by a number of factors, and they can be very different in nature.
For the purpose of systematization, all the causes of this disease are divided into groups:
- neurological;
- nutritional (food);
- infectious;
- somatic;
- tumor;
- mental;
- bad habits;
- medicinal.
The neurological reasons that provoke the occurrence of the described disorder are pathologies of the peripheral and central nervous system, due to which the nervous regulation of the stomach is disrupted. They can be inflammatory, traumatic, tumor or other in nature.
The nutritional (food) causes of the development of this disease include alternating diets with severe restrictions and overeating.
It is assumed that the bacterium Helicobacter pylori, which inhabits this organ, may be involved in the occurrence of acute dilation of the stomach. Also, this condition developed after an inflammatory lesion of the stomach with the addition of staphylococci, streptococci, E. coli and some specific pathogens (in particular, Mycobacterium tuberculosis).
Of the somatic disorders, most often the background for the development of the described pathology are:
- formation of stones in the bile duct system;
- pyloric stenosis;
- his scars
and so on.
Of the tumors, any neoplasm that becomes a barrier to the food masses evacuating from the stomach is important for acute expansion of the stomach. These can be either benign or malignant tumors.
What bad habits can provoke the development of the described pathology? This includes smoking and drinking alcoholic beverages. Nicotine constricts blood vessels (including in the wall of the stomach), due to which blood flow worsens, less nutrients (fats, proteins, carbohydrates) reach the tissues of the gastric wall, it becomes depleted and then stops contracting as usual.
note
Drug-induced causes of acute gastric dilatation most often are drugs administered to the patient to ensure medicated sleep during surgery.
Development of pathology
Even if the root cause of acute gastric dilatation is not neurological disorders, the end result, regardless of the etiological factor, is the disruption of the nervous supply of this organ. Bioelectric impulses that move along neurons begin to move faster and more slowly - the muscular wall of the stomach reacts to such a slowdown: its tone sharply decreases, it practically loses the ability to contract.
The contents that have accumulated in the lumen of the stomach put pressure on its walls, and violations on their part lead to greater development of atony of the gastric wall. Thus, a kind of vicious circle is formed.
note
In acute dilatation of the stomach, the disorder is that the gastric wall loses its ability to absorb liquid, while its secretory (excretory) function is preserved.
With the disease described, not only the stomach suffers. It, being overfilled with liquid contents, shifts, which causes the organs adjacent to it to shift - the duodenum, small intestine, jejunum and loops of the large intestine. They are attached to the abdominal wall by the mesentery, which becomes stretched with such displacement. The mesentery contains blood vessels and nerve structures of the small and large intestines, so if it is damaged, then these elements suffer.
The following types of acute gastric dilatation have been identified:
- by degree of increase - initial, medium, pronounced;
- according to the presence of consequences - complicated, uncomplicated;
- by drawing neighboring organs into the pathological process;
- by type of expansion - primary (initiated by a large amount of food in the lumen of the stomach), secondary (associated with damage to the nervous apparatus of the gastric wall).
Can the stomach stretch?
There are many myths that circulate among people. One of them: “My stomach has stretched. I ate a lot and very quickly, it’s my fault, I stretched my stomach.”
Moreover, this works both for bariatric patients and for those who have not had any surgery. That is, people come before surgery and explain their excess weight to themselves as a result of a distended stomach. Nutritionists often tell stories about how a person has a large stomach, so he eats a lot, and if he eats less, his stomach shrinks in size.
It is a myth! Because it contradicts normal anatomy, human physiology and common sense in general. The stomach is just one of the human organs. It is of the shape and size that nature gave it.
A person’s weight does not depend on the size of the stomach! Fat people have small stomachs, while thin people can have very large stomachs.
The stomach can stretch, but only in the presence of some pathological disease. For example, an ulcer or scar deformity develops in the pyloric area, which leads to difficulty in evacuating food. In this case, the esophagus, like a pump, will create chronic high pressure in the stomach. The stomach stretches, becoming very large. It can occupy the entire space of the abdominal cavity. This is a very bad disease, but on the contrary, the person loses a lot of weight because he cannot eat anything and he develops vomiting syndrome.
It is theoretically also possible to stretch your stomach after bariatric surgery, but again this is not the patient’s fault, but rather the mistake of the bariatric surgeon who performed an incorrect operation. For example, if during sleeve gastroplasty you make an uneven gastric tube, and make a slight narrowing in the middle of this tube, then an expansion of the stomach will gradually develop above the narrowing. The esophagus will constantly put pressure there, the evacuation of food is difficult due to the obstruction, the muscular wall of the stomach stops contracting, atrophies and stretches. In this case, it is necessary to perform reconstructive bariatric surgery to realign the gastric tube.
What are we talking about when we see complaints about “stomach distension”? Bariatric forums are full of messages like this: “Everything was fine for me, 3-4 years have passed since the operation, I started eating more, my stomach has stretched.” In such patients, if the operation is performed correctly, we do not see any expansion of the stomach. The patient himself can verify this by taking a regular X-ray of the stomach.
We see something different. Unfortunately, the body can adapt to everything. And unfortunately, the genetics of bariatric patients do not change after surgery. The predisposition to the accumulation of fat cells does not go away. Yes, the body now does not have a tool for this accumulation; it cannot force a person to eat more than what he wants. That's why he invents such a tool.
The nervous impulse that comes from the esophagus, which feels pressure in the stomach, gradually weakens. That is, the feeling of fullness that occurs as a result of eating solid food gradually weakens. This effect is confused by patients, mistaking it for a distended stomach.
How to avoid this? Very simple. In the first year after surgery, when food evokes virtually no emotions and does not affect a person’s actions in any way, it is necessary to develop correct eating behavior to the point of automaticity:
- eat first what you need to chew
- eat long and slowly, chewing food thoroughly
- eat regularly with equal intervals between meals.
Following these simple rules will help you avoid the effect of a “stretched stomach”, which is actually a response of the body consisting in dulling the severity of satiety. But even if you do not follow these rules, the weight return will be small. It is considered normal if, after several years after surgery, 10-20% of the original body weight returns.
If the weight gain is more serious, we are talking about the fact that the patient is indicated for either a stronger bariatric surgery, or the primary operation has stopped working due to a developing postoperative complication.
As a rule, people forget all these rules and nuances very quickly. They get the desired results and enjoy a new life at a normal weight. Often they switch to a diet according to the formula “I eat what is easier to eat.” They begin to eat on the go, swallowing unchewed food. This is a big mistake!
You should always remember your genetics, stay in touch with information, periodically meet with your surgeons and remember their recommendations. Unfortunately, this is a lifelong condition for the literate bariatric patient.
Symptoms of acute gastric dilatation
Acute gastric dilatation is an acute condition. The clinical picture develops quite quickly, the disorders progress before our eyes. There is a deterioration in the patient's condition literally over the course of one hour.
The clinical picture is represented by the following signs:
- local;
- are common.
The main local symptoms of acute gastric dilatation are:
- pain;
- hiccups;
- dyspeptic disorders.
The characteristics of pain in this pathology will be as follows:
- by localization - in the epigastric region;
- by distribution - pain can spread to neighboring locations, and as the pathology progresses - to the entire abdominal cavity, while the patient seems to have pain throughout his entire abdomen;
- by nature – pressing, bursting, spasmodic, sharp;
- in terms of severity - medium intensity or strong, increasing with the progression of pathology and an increase in the amount of stagnant contents in the stomach;
- by occurrence - they appear when contents accumulate in the stomach, occupying about a fifth of this organ; with a progressive increase in its quantity, they increase.
note
With acute dilatation of the stomach, abdominal pain is caused not only by stretching of the stomach, but also by uncontrollable vomiting, due to which the anterior abdominal wall becomes tense.
Hiccups with acute dilatation of the stomach occur reflexively.
Dyspeptic disorders that occur with stromal dilatation of the stomach are:
- nausea;
- vomit;
- worsening of gas discharge;
- violation of the act of defecation.
Nausea with acute dilatation of the stomach is constantly observed, accompanied by the urge to vomit.
Vomiting is the most important symptom of the described disease. Its characteristics are as follows:
by occurrence - as a rule, it appears at the time of an acute painful attack from the stomach;- in terms of frequency – very frequent, the patient does not have time to literally catch his breath after one attack of vomiting before the next one begins;
- by nature - gushing, with vomit literally pouring out from the gastrointestinal tract;
- in terms of the amount of vomit - on average from five to ten liters per day;
- by the nature of the vomit - they are stagnant stomach contents. In particularly severe forms of vomiting, it may contain impurities of bile and coffee grounds. The second signals a violation of the integrity of the gastrointestinal tract vessels and bleeding - the blood mixes with the gastric contents, forming a specific brown substance;
- According to the patient’s subjective feelings, vomiting does not bring relief, and if it is prolonged, it leads to exhaustion of the patient’s strength, who is no longer able to tolerate convulsive contractions of the gastric wall.
note
It is characteristic that after some time the number of vomiting “acts” and the volume of vomit decrease. This is explained by the patient's dehydration, so a decrease in the intensity of vomiting is an alarming diagnostic sign.
Since the intestines are not affected, gases continue to pass, but due to the triggering of the reflex mechanism of the intestinal response, it is worse.
A patient with acute gastric dilatation has irregular diarrhea.
General symptoms of acute gastric dilatation occur due to the body losing a large amount of fluid. The following signs are observed:
- general weakness;
- feeling overwhelmed;
- severe impairment of ability to work – mental and physical;
- lethargy;
- “flies” before the eyes;
- decrease in the amount of urine excreted per day;
- decrease in body temperature.
general description
Operated stomach syndrome (Dumping syndrome) is a complication after gastric resection, in frequent cases using the Billroth II method.
One of the common post-resection syndromes. It manifests itself as a specific symptom complex consisting of: a vegetative-vascular crisis with vasomotor, hemodynamic, dyspeptic, hormonal, and metabolic disorders that occur during meals rich in carbohydrates. Dumping syndrome occurs in approximately 25-50%, mainly in women, with operated duodenal ulcer (in 60-70% of cases).
Depends on the volume of surgical treatment - resection according to Billroth-2, dumping syndrome occurs 3-4 times more often than resection according to Billroth-1.
Diagnostics
The diagnosis of acute gastric dilatation is made through a comprehensive examination - the patient’s complaints, details of the anamnesis (history) of pathology, and the results of additional examination methods (physical, instrumental, laboratory) are taken into account.
From the anamnesis, the following is revealed:
- what does the patient associate with the clinical picture that has developed;
- how often does vomiting occur?
- whether the patient previously suffered from any stomach pathologies.
Physiological examination reveals the following abnormalities:
- upon general examination, the patient’s general condition is of moderate severity, and with the progression of the disease (in particular, uncontrollable vomiting), the condition is close to severe. The skin and visible mucous membranes are pale, the skin is dry due to dehydration due to vomiting;
- upon local examination, the tongue is dry, covered with a white coating, and an unpleasant putrid or fermentative odor may be felt from the mouth. In thin patients, there is a protrusion in the epigastric region due to an enlarged stomach. With flatulence, bloating is visualized;
- during palpation (palpation) – pain in the epigastric region and fluctuation (fluctuations of the fluid during pushing movements with the examiner’s fingers) are noted. If flatulence occurs, its presence is also confirmed by palpation;
- during percussion (tapping) - at the site of projection of the overfilled stomach onto the anterior abdominal wall, a dull sound is noted when tapping. In the lower sections, against the background of flatulence, the sound will be similar to that which occurs when tapping on a hollow object;
- during auscultation (listening with a phonendoscope), a splashing noise is noted. Over the lower abdomen, peristaltic bowel sounds are weakened.
Instrumental research methods that are used in the diagnosis of the described disease are:
- plain radiography of the abdominal organs. Despite the fact that this diagnostic method is generally less informative than other methods, in this case it plays an important role: X-ray images show a distended stomach, while neighboring organs are displaced. The increase in the volume of the stomach can reach such an extent that its lower edge reaches the pelvic region;
- Contrast radiography - the patient ingests a portion of a suspension of barium sulfate (a contrast agent), after which a series of X-ray images are taken. In the photographs, the stomach is presented as a shapeless bag overflowing with a contrast agent. Also, due to their serial nature, the images allow one to estimate the rate of evacuation (release) of the contrast agent from the stomach - with its acute expansion, they are critically slowed down or evacuation does not occur at all;
- fibrogastroduodenoscopy (FGDS) - a fibrogastroscope (a type of endoscopic equipment) is inserted into the stomach through the esophagus, examined from the inside, and the size of the organ is assessed using indirect signs. It is often difficult to evaluate what is seen during FGDS, since the stomach is filled with mucus, gastric juice and fermented food masses that are not evacuated into the duodenum due to atony of the gastric wall;
- computed tomography (CT) - when carrying out this research method, layer-by-layer images-sections of the tissue of the gastric wall are taken, which allow one to evaluate its structure. Thanks to this, the information content of the method is very high and allows you to identify violations;
- multislice computed tomography (MSCT) is a type of computed tomography, but more advanced;
- Magnetic resonance imaging (MRI) - during this procedure, layer-by-layer images of the gastric wall are also obtained. But MRI, in comparison with CT and MSCT, is more informative when studying soft tissues.
Laboratory research methods used in the diagnosis of acute gastric dilatation are:
general blood test - the most characteristic sign is a violation of hematocrit (the ratio of formed elements and the liquid part of the blood). With prolonged pathology, due to the addition of an infectious agent, an increase in the number of leukocytes (leukocytosis) and ESR is observed;- biochemical blood test - there is a decrease in the amount of sodium, potassium, chlorine, and an increase in the amount of nitrogen compounds. The first occurs due to profuse vomiting, the second due to the fact that stagnant gastric contents begin to ferment, fermentation products are absorbed into the blood, reach the liver and kidneys and negatively affect their function in removing nitrogenous products of tissue metabolism;
- microscopy of gastric contents - it reveals undigested food elements, and at later stages of pathology development - an attached infectious agent.
Differential diagnosis
Differential (distinctive) diagnosis of acute gastric dilatation is most often carried out with diseases and pathological conditions such as:
- gastritis is an inflammatory lesion of the gastric mucosa. Differential diagnosis should be carried out with the acute form of this pathology;
- duodenitis - inflammation of the duodenal mucosa;
- gastric bezoar is a foreign body formed from undigested elements that were swallowed accidentally or purposefully;
- Gastric ulcer is the formation of deep destruction of the gastric wall. Differential diagnosis should be carried out with this pathology in the acute stage;
- perforated ulcer - the occurrence of a through defect in the wall of the stomach at the site of ulceration, which is accompanied by the release of gastric contents into the abdominal cavity;
- penetrating ulcer – spread of the ulcerative process from the stomach wall to neighboring organs;
- pancreatitis - an inflammatory process in the parenchyma (working tissue) of the pancreas;
- pancreatic necrosis – necrosis of the pancreatic parenchyma, which occurs when simultaneously ingesting large amounts of fatty foods and alcoholic beverages;
- intestinal obstruction - a violation of the passage of food masses through the intestinal lumen;
- food toxicoinfection – poisoning by food products containing pathogenic microflora;
- dysentery - acute infection of the intestines by Shigella, which is characterized by profuse repeated diarrhea;
- peritonitis is an inflammatory lesion of the peritoneum (the connective tissue film that lines the inside of the abdominal wall and covers its organs).
Complications
The main consequences of acute gastric dilatation are:
violation of the motor function of the organ - its contents are not evacuated into the duodenum;- indigestion;
- perforation of the gastric wall - the formation of its through defect. The gastric wall itself is a strong elastic structure, but if the patient suffered from a gastric ulcer, then due to the high pressure of the contents, even greater thinning of the wall at the site of the ulcer and the formation of a through defect are possible;
- gastrointestinal bleeding.
Treatment of acute gastric dilatation
Treatment of the described pathology can be conservative and surgical.
Acute gastric dilatation refers to acute conditions - that is, those that require immediate intervention. First, medical care is provided aimed at improving the patient’s condition, then he is taken to the clinic, where he will undergo a comprehensive examination and treatment.
Important
In case of acute dilatation of the stomach, a nasogastric tube is inserted to remove excess contents from the stomach. In this case, it is strictly forbidden to stimulate the patient to vomit.
The main appointments in the clinic are:
- bed rest;
- hunger;
- placement of a nasogastric tube - it remains in the stomach for 24-76 hours, sometimes up to 5-6 days;
- drug therapy.
The duration of bed rest is determined by the general condition of the patient.
The contents of the stomach are not only released through the tube - it must be actively sucked out.
Medication prescriptions are as follows:
- infusion therapy;
- general strengthening appointments.
The purpose of infusion therapy is to restore the amount of fluid in the body that was lost during attacks of profuse (uncontrollable) vomiting. Saline solutions, electrolytes, glucose, blood serum, and so on are injected intravenously.
General restorative therapy means:
- parenteral nutrition - intravenous administration of protein drugs, since the patient cannot eat food in the usual way;
- vitamin therapy - the use of injectable drugs.
Surgical treatment is carried out for certain conditions that could provoke acute dilatation of the stomach. So, in case of violations on the part of the mesentery, its partial excision is performed. In some cases, it is necessary to form a communication between the stomach and the anterior abdominal wall - this will ensure gastric emptying. During surgical treatment, drug therapy is carried out in full.
Technical aspects
The advantage, at least theoretically, of balloon dilatation over bougienage is its uniform impact throughout the stricture and the virtual absence of axial load on the tissue.
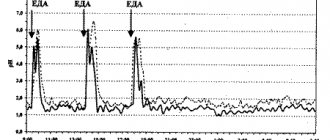
Currently, there are three types of balloons: those installed along a guide under X-ray control, those installed through an endoscope channel under visual control, and a combination of the first and second types (balloons for dilatation of biliary strictures). Balloons for endoscopic dilatation of strictures are shown in Fig. 1.
When using a guide, it is passed through the stricture (using an endoscope or X-ray control), a balloon (with X-ray contrast marks) is passed through it, which is installed so that the stricture falls on its central part, then using a special inflating device the balloon is filled with water-soluble contrast up to a certain pressure (specified by the manufacturer for each cylinder of a specific diameter). Initially, a “waist” is clearly visualized on the balloon in the area of narrowing, which disappears with successful dilatation.
Balloons designed to be passed through an endoscope can be installed in two ways:
- If the device can be passed through the stricture, which happens, however, relatively rarely. Then, after overcoming it, the balloon is completely removed from the canal and then the device begins to be removed along with the balloon until its correct location in the stricture is achieved.
- If the stricture is insurmountable, the device attempts to “cannulate” the area of stenosis with a balloon.
Successful dilatation is judged by the ability of the inflated balloon to move back and forth across the stricture.
In our work, we use a combination of endoscopic and radiological control for balloon installation and dilatation. The dilator is passed through the endoscope channel and, under X-ray control, is installed in the center of the narrowing. Inflation is carried out under X-ray control until the “waist” disappears, but without exceeding the maximum recommended pressure.
We usually keep the balloon inflated in the area of the stricture for 2-3 minutes. Then the balloon is deflated and removed from the canal. The area of the eliminated stricture and previously inaccessible areas of the gastrointestinal tract due to it, for example, the stomach and duodenum with esophageal strictures, are examined endoscopically.
The question that remains quite difficult to resolve is: to what diameter should dilatation be carried out? On the one hand, there is evidence that perforation occurs more often when using a balloon with a diameter of 18 mm, at least when it is used to treat stenoses of the gastric outlet [5], on the other hand, clinical symptoms are closely related to the diameter of the narrowing. When using balloons (or bougies) to dilate esophageal strictures, it is recommended to dilate the stricture in one session by 6-10 F compared to its initial diameter [19]. This approach seems to us to be reasonably cautious; we try not to dilate strictures, regardless of their location, by more than 10 F during a single procedure. For esophageal strictures, some authors recommend dilatation to achieve a lumen of 14-15 mm (42-45 F) [13]. As for colonic strictures, there is evidence that after dilation of colonic anastomotic strictures to 40 F, symptoms of obstruction disappeared in 90% of patients [4]. In our work, in the vast majority of cases, we use a balloon with a diameter of no more than 16 mm due to the increased risk of perforation and virtually no difference in symptoms in patients with strictures extended to 16 and 18-20 mm.
It is necessary to adequately prepare the patient for dilatation - with severe strictures of the esophagus and gastric outlet, the overlying sections may contain a large amount of fluid and remnants of food eaten the day before. It is necessary to wash the contents through the probe. Adequate preparation is also extremely important to eliminate colonic strictures.
Like other therapeutic endoscopic interventions, dilatation should be performed only with adequate sedation of the patient.
Before the procedure, an endoscopic examination of the stricture with a biopsy and an X-ray examination with barium are required. A study with water-soluble contrast is also performed after dilatation to exclude perforation. Repeated endoscopic examination is also recommended to exclude complications. Sometimes it is reasonable to take a second biopsy from the area of narrowing to rule out a malignant nature of the lesion.
Indications for dilatation are only strictures with obvious clinical symptoms and sometimes the need to exclude its malignant nature, such as strictures arising against the background of ulcerative colitis.
Prevention
Measures to prevent acute gastric dilatation are:
prevention, identification and treatment of neurological disorders, against the background of which the innervation of the stomach may suffer with the subsequent development of the described condition;- adherence to the principles of proper nutrition, avoiding strict diets and overeating;
- neutralization of the bacterium Helicobacter pylori. For this purpose, courses of antibacterial therapy are carried out;
- prevention, diagnosis and relief of somatic pathologies that can cause acute dilatation of the stomach - cholelithiasis, pyloric stenosis, its scars, and so on;
- prevention, detection and elimination of tumor pathologies of the stomach;
- rejection of bad habits;
- correct administration of anesthesia.
Discussion
Two rare cases of the formation of large ulcers in the antrum of the stomach in children of early and preschool age are presented. The etiology of the ulcer in the first case has not been reliably established; in the second, the cause was probably unjustified and uncontrolled use of NSAIDs. Secondary peptic ulcer in both cases was complicated by stenosis of the gastric outlet. Children were hospitalized with symptoms caused by this condition. Taking into account age, medical history, general and somatic condition, results of laboratory and instrumental studies, with the consent of the parents, a decision was made to conduct experimental balloon dilatation therapy for the pylorus of the stomach. At the end of the intervention and in the postoperative period, a positive result of endoscopic treatment was noted, determined both clinically and instrumentally.
The value of the experimental cases lies in the clarity of the benefits of using the developed high-tech minimally invasive intraluminal method for correcting pyloric stenosis in children and in its obvious accessibility and effectiveness.
In addition to the high-tech, minimally invasive, well-tolerated and other advantages of the method, the use of equipment in the form of balloon dilators is in itself as safe as possible: the balloon does not overextend beyond the technically specified outer diameter under the influence of distilled water pumped into it, which makes it possible to achieve the required force of influence in the area of stenosis, in addition, pressure on the wall is exerted from the inside radially and at the same time along the entire length of the stenosis area, which reduces the risk of perforation to a minimum [10, 11, 29]. During one session, you can use 1-2 balloon dilators of increasing diameter or inflate one balloon to different diameters, if this is provided for by its design. Each diameter corresponds to a certain level of pressure, which is pumped into the balloon by an insufflator [30]. It is optimal to keep the balloon inflated for 120 s.
Intervention under endoscopic control has certain advantages compared to alternative X-ray control: there is no radiation exposure to the sick child and the doctor; intervention is also feasible in cases where it is not feasible using only X-ray techniques, for example, if it is impossible to pass the guide string under X-ray control due to severe stenosis, tortuous course of the narrowing, deformation of the suprastenotic region; direct local visual assessment is possible [31, 32]. At the end of the intervention, it is advisable to examine the duodenal bulb. A repeat dilatation session is carried out no earlier than 2-3 days later [31].
If it is not possible to achieve completely free passage of the pylorus by the endoscope after double dilation therapy, it is recommended to continue local dilation therapy after 3 months to maintain and improve the positive result and prevent recurrence of stenosis.
In the future, it is necessary to create an independent evidence base by conducting an original scientific study using the developed method in a statistically significant number of children. Based on these data, it will be possible to draw an objective conclusion about the effectiveness and feasibility of introducing a new method.
Forecast
The prognosis for acute gastric dilatation is generally favorable. With the help of competent prescriptions, you can stop the causes of this pathology and its consequences.
At the same time, complications of this disease occur quite often: bleeding of varying severity and perforation of the gastric wall are observed, according to some data, in every fifth patient with this diagnosis.
The prognosis worsens with:
- complications;
- late relieved dehydration.
Kovtonyuk Oksana Vladimirovna, medical observer, surgeon, consultant doctor
1,859 total views, 1 views today
( 59 votes, average: 4.88 out of 5)
Dysphagia in children: causes and treatments
Liver steatosis: causes, symptoms and treatment
Related Posts
Esophagus
The main indications for dilatation are peptic and caustic strictures. Dilatation of tumor narrowings and anastomotic strictures is also possible. Dilatation is also successfully used for achalasia cardia. In our experience, the most rewarding are short narrowings of the lumen of a peptic nature. When adequate antisecretory therapy is prescribed, such strictures rarely recur.
Dilatation in strictures resulting from burns of the esophagus with acid or alkali is the most difficult (due to the often high extent, tortuosity and density of the narrowing). Often a series of dilations with balloons of different diameters (from small to large) is used over 3-7 days. The recurrence rate of such strictures is high.
Tumor stenoses are, as a rule, easy to dilate, but the elimination of dysphagia is rather short-term. In a series of 39 patients with esophageal cancer, dilation reduced dysphagia in 90% of patients; complications included one perforation [12]. Dilations for tumor strictures can be performed repeatedly, with repeated appearances of dysphagia. According to one study, patients with this pathology typically required repeat dilatation every 4 weeks [10]. After eliminating the tumor stenosis, it is necessary to perform stenting with a self-expanding metal stent, which, however, in Russia is not always possible for financial reasons. There are reports of the successful combination of dilatation with chemotherapy as a palliative treatment for inoperable tumors of the cardia [7].
When dilating strictures of esophageal anastomoses, the results are more favorable for short strictures (if their length is more than 12 mm, balloon dilatation is generally ineffective), but the result does not depend on the diameter of the narrowing. The results are worse with manual anastomoses and with a history of their failure [6].