General information
Clostridiosis (clostridium spp) is an infectious disease with an acute course. It is caused by clostridia - gram-positive anaerobic bacteria that can produce endospores. Thanks to this, they are well preserved in the external environment. It is the varieties of these bacteria that produce the most toxic poisons: botulinum toxin, tetanospasmin, ε-toxin. They cause very serious diseases: tetanus , botulism , gas gangrene , etc. But most often they are affected by the bacterium Clostridium difficile. Normally, these bacteria are part of the microflora of the gastrointestinal tract and genital tract in women. Clostridium difficile is a representative of normal microflora; it causes colitis and enterocolitis if it multiplies too actively. The toxin produced by the bacterium clostridium perfringens can cause foodborne illness, and the toxin produced by clostridium botulinum causes botulism.
Clostridium perfringens is the main causative agent of gas gangrene
Gas gangrene, food poisoning and necrotic enteritis in humans and animals are caused by Clostridium perfringens types A, C and D. Similar diseases, but only in animals are caused by Clostridium perfringens types B, C, D and E.
The pathogen was first discovered by Welch and Nettal in 1892.
Morphology of Clostridium perfringens
Bacteria look like rods with rounded ends. They are large, measuring 3-9 × 0.9-1.2 microns. Fixed. They are located singly. Clostridia isolated from pure cultures have a capsule. Gram stained purple. Old cultures are losing this ability. They form spores that persist in the environment for many decades.
Rice. 7. Smear from a pure culture of Clostridium perfringens (photo on the left). Bacterial spore (photo on the right).
Rice. 8. The photo shows the bacteria Clostridium perfingens and spores.
Cultivation of Clostridium perfringens
Clostridium perfringens are strict obligate anaerobes, chemoorganoheterotrophs. They grow on simple nutrient media - blood sugar agar and Kitta-Tarozzi medium. The growth of bacteria is accompanied by gas formation and a decrease in pH towards the acidic side.
- On sugar-blood agar, bacteria form smooth, shiny, round shapes (S-colonies), or grayish colonies, flat, rough with jagged edges (R-colonies). A hemolysis zone forms around the colonies. When exposed to air, colonies acquire a greenish color. Colonies in the thickness of the agar acquire a lenticular shape.
- When growing in liquid media (Kitta-Tarozzi medium), turbidity is formed with intense gas formation. Subsequently, the medium clears and a whitish plate-like sediment falls to the bottom.
- When growing on bile agar, precipitation zones form.
- When growing on milk, after 4 hours intensive coagulation is noted, and the curd, due to gas formation, acquires a holey structure and often bounces up. A similar reaction is used in laboratories for rapid diagnostics.
- When growing in meat broth, bacteria produce acetic and butyric acids, as well as large amounts of gases such as H2S, NH3 and CO.
Rice. 9. Clostridium perfringens colonies on blood agar.
Rice. 10. C. perfringens is identified by its characteristic “double zone” of hemolysis.
Biochemical properties of clostridia
The powerful enzymatic activity of bacteria gave them the epithet perfringens, which means breaking, breaking through. Due to intense gas formation, swelling of damaged tissues and ruptures of nutrient media occur. Clostridium perfringens produce a huge number of saccharolytic enzymes that ferment glucose, lactose, maltose and sucrose with the subsequent formation of acid and gas. They intensively curdle milk, followed by the formation of a spongy, coarse-celled clot (“storm reaction”).
Bacteria decompose gelatin, egg whites, coagulated whey and collagen. Does not decompose casein.
During acetobutyrate fermentation, Clostridium perfringens synthesize butyric acid, reduce nitrates to nitrites, and form lecithinase.
Rice. 11. Determination of lecithinase activity. Around the colonies, zones of a turbid halo consisting of precipitated lipids are clearly visible.
Rice. 12. In the left test tube is a culture of Clostridium perfringens on sugar agar. As a result of intense gas formation in the helium-like medium, rupture zones formed.
Toxin formation
The bacteria Clostridium perfringens, according to the spectrum of toxins (enzymes) they produce, are divided into types A, B, C, and E. Gas gangrene and foodborne toxic infections are more often associated with type A, necrotizing enterocolitis - with type C. The concept of “toxin” unites about 12 identified today toxins (enzymes) and enterotoxin. The release of enzymes in the area of damaged tissue leads to the breakdown of complex substances and disruption of cellular permeability, as a result of which cells swell and melt.
Main exotoxins of clostridia
- α-toxin (phospholipase C). It is produced more intensively by clostridia type A. It is the main and most powerful toxin. The enzyme hydrolyzes (breaks down) phospholipids of cell membranes, which leads to destruction (lysis) of cells. It has a dermatonecrotic and lethal effect, and is the main factor in interstitial invasion and intravascular hemolysis - a symbol of fatal clostridial toxinemia. Has lecithinase activity.
- b-toxin (cytotoxin). Mainly produced by clostridia types B and C. It has a dermatonecrotic and lethal effect and does not cause hemolysis. It causes the development of necrotic enteritis.
- Theta toxin. It has hemolytic and dermatonecrotic effects. Sensitive to oxygen. It is similar to O-streptolysin of streptococci.
- v-toxin (proteinases). They disrupt protein synthesis reactions by splitting nucleic acids.
- p-toxin (collagenase and gelatinase). Produced by clostridia types A, C and E, as well as some strains of bacteria type D. Enzymes break down gelatin and collagen fibers of connective tissue. They have a necrotizing and lethal effect.
- Mu-toxin (hyaluronidase). It is a factor in the penetration of clostridia. Enzymes break down acidic mucopolysaccharides and hyaluronic acid.
- Nu-toxin (DNA-za). Destroys cellular DNA.
- q-hemolysin. With the participation of complement, it destroys red blood cell membranes.
- Fibrinolysin. Dissolves fibrin fibers.
- Hemagglutinin. With its participation, the agglutination reaction of erythrocytes occurs.
- y-toxin (proteinase). Its action resembles fibrinolysin. Does not break down native (natural) collagen, but destroys azocoll (denatured collagen), casein and gelatin.
- Delta toxin (elastase). It is a proteolytic enzyme. Breaks down proteins and peptides.
- Sigma toxin. They produce clostridia types B and C. It has a lethal effect and exhibits hemolytic activity.
- Omega toxin. Produced mainly by clostridia type C. It has a dermatonecrotic and lethal effect.
- Epsilon is a toxin. Produced by clostridia types B and D, l-toxin - by clostridia type E. They exhibit a lethal and dermatonecrotizing effect.
- y- and n-toxins. The biochemical nature of these toxins remains unknown.
- p-toxin. It is a tissue permeability factor.
Enterotoxin of the causative agent of gas gangrene
Enterotoxin is produced by clostridia types A and C.
- Clostridium perfringens enterotoxin strain A is a heat-labile protein released in the small intestine during spore formation. When exposed to it, capillaries expand, their permeability increases, the secretion of water, sodium and chloride ions increases, and the membranes of enterocytes are damaged.
- The enteropathogenicity of Clostridium perfringens type C is associated with b-toxin. The disease occurs as necrotizing enteritis.
Rice. 13. Under unfavorable conditions, some bacteria form spores. They help the microorganism survive in unfavorable conditions for many decades. The photo shows spores of bacteria of the genus Clostridium.
Pathogenesis
- Clostridium difficile is a gram-positive rod that produces two exotoxins: enterotoxin A and cytotoxin B. Both of them provoke diarrhea syndrome. Clostridium difficile in the form of spores demonstrates high resistance in the external environment and can survive in the intestines even at high concentrations of a number of antibiotics . Clostridia difficile is the main causative agent of pseudomembranous colitis, a dangerous condition for newborns and young children. In addition, they provoke other enterocolitis and colitis after irrational antibiotic treatment. The pathogen is transmitted by contact. The disease caused by this pathogen develops during or after treatment with broad-spectrum antibiotics. Under the influence of certain antibacterial drugs ( lincomycin , clindamycin , ampicillin , etc.), changes occur in the intestinal microflora and colonies of clostridium difficile appear. They actively reproduce and provoke disease. The disease can also develop as a result of exogenous infection during or immediately after antibacterial treatment. The disease develops immediately after treatment is discontinued or after a few weeks; it can be protracted or become chronic.
- Clostridium perfringens is a gram-positive bacteria, the causative agent of toxic infections and gas gangrene. Clostridium perfringens is a representative of opportunistic microflora; they persist in the external environment for a long time. The bacteria Clostridium perfringens causes foodborne illnesses. And when Clostridium perfringens gets into an open wound, they produce toxins that damage surrounding tissues and create conditions for further spread of infection. C. perfringens type A is the main etiological factor of gas gangrene.
- Clostridium botulinum is an anaerobic bacterium that grows in the absence of oxygen. Produces spores that are widely distributed in soil, water, etc. Bacteria enter food products, grow in them and produce toxins . After consuming contaminated food, mainly canned food, a person becomes infected with botulism.
- Clostridium tetani is a spore-forming, Gram-positive, anaerobic bacterium. It is the causative agent of tetanus. Transmitted by contact. Bacteria produce tetanospasmin , which affects the nervous system and provokes tonic contractions of striated muscles. It is neutralized by antitetanus serum. The bacterium also produces tetanolysin .
Clostridium (clostridia)
Clostridia
(lat.
Clostridium
) - a genus of gram-positive spore-bearing bacteria.
Clostridia are part of the normal human microflora. However, some types of clostridia can cause disease. The name “clostridia” comes from the Greek κλοςτεδ
(spindle), since during sporulation the clostridia swell in the center and take on the shape of a spindle.
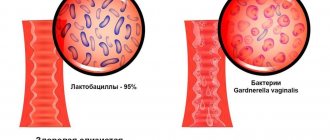
Clostridia - normal human microflora
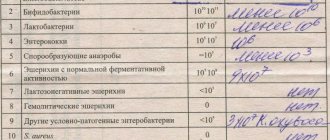
Clostridia are found in healthy people in the intestines, in the female genital tract, and sometimes on the skin and in the mouth. The main habitat of clostridia in the human body is the large intestine. There are no clostridia in the duodenum and jejunum; in the ileum, their population is normally 102–104 colony-forming units (CFU)/ml. The following amounts of clostridia are found in the stool of healthy people:
- in children under one year of age - up to 103 CFU/g
- in children over one year old and adults up to 60 years old - up to 105 CFU/g
- in adults over 60 years old - up to 106 CFU/g
During their life activity, clostridia produce short-chain fatty acids: butyric, isobutyric, valeric, capronic, isovaleric, isocaproic (Akopyan A.N.).
Clostridia are pathogens
Most clostridia are not pathogenic, but some types of clostridia can cause various human diseases, some of which are severe and can be fatal. In particular, Clostridium botulinum
can cause botulism,
Clostridium tetani
- tetanus,
Clostridium perfringens, Clostridium novyi, Clostridium oedematiens
and
Clostridium septicum
- gas gangrene.
Clostridium perfringens
can also cause foodborne illness due to a toxin produced by
Clostridium perfringens
.
8–14 hours after eating Clostridium perfringens-
meat, poultry, or legumes, watery diarrhea, nausea, abdominal cramps, and sometimes fever begin. The duration of the illness is one or two days.
Clostridium perfringens
type A can cause antibiotic-associated diarrhea or pseudomembranous colitis.
Clostridium perfringens
type F can cause necrotic enteritis.
Clostridium tetani
is the causative agent of tetanus, an acute infectious disease of humans and animals, characterized by damage to the nervous system and manifested by tonic tension of skeletal muscles and generalized convulsions.
Clostridia can cause diseases of the human genitourinary organs, in particular acute prostatitis.
By Order of the Ministry of Health and Social Development of Russia No. 1664n dated December 27, 2011 “On approval of the nomenclature of medical services,” medical and “A26.19.007 Bacteriological examination of stool for clostridium (Clostridium spp.)” are included in the nomenclature of medical services, section 26.
Antibiotics active against clostridia
Antibacterial agents (those described in this reference book) active against clostridia: metronidazole, tinidazole, rifaximin, tetracycline, doxycycline, lincomycin.
Clostridia species resistant to clindamycin: Clostridium sporogenes
and
Clostridium tertium.
Clostridia in the taxonomy of bacteria
According to modern classification, the genus of Clostridia is included in the family Clostridiaceae
, order
Clostridiales
, class
Clostridia
, phylum
Firmicutes
, <group without rank>
Terrabacteria group
, kingdom Bacteria.
The genus Clostridia includes more than 100 species: C. aceticum, C. acetireducens, C. acetobutylicum, C. acidisoli, C. aciditolerans, C. aestuarii, C. akagii, C. alcalibutyricum, C. alcaliphilum, C. algidicarnis, C. algifaecis, C. algoriphilum, C. amazonense, C. aminobutyricum, C. aminovorans, C. amylolyticum, C. arbusti, C. argentinense, C. aurantibutyricum, C. autoethanogenum, C. baratii, C. beijerinckii, C. bogorii, C. boliviensis, C. bornimense,
C. botulinum , C. bovipellis, C. bowmanii, C. butyricum, C. cadaveris, C. caliptrosporum, C. caminithermale, C. carboxidivorans, C. carnis, C. cavendishii, C. celatum, C. cellulovorans, C. chartatabidum, C. chauvoei, C. chromiireducens, C. cochlearium, C. colicanis, C. collagenovorans, C. corinoforum, C. coskatii, C. crotonatovorans, C. cylindrosporum, C. diolis, C. disporicum, C. drakei, C. elmenteitii, C. estertheticum, C. fallax, C. favososporum, C. felsineum, C. filamentosum, C. formicaceticum, C. frigidicarnis, C. frigoriphilum, C. frigoris, C. fusiformis, C. ganghwense, C. gasigenes, C. grantii, C. guangxiense, C. haemolyticum, C. halophilum, C. homopropionicum, C. huakuii, C. hveragerdense, C. hydrogeniformans, C. hydrolyticum, C. ihumii, C. intestinale, C. isatidis, C. islandicum, C. kluyveri, C. kogasensis, C. lacusfryxellense, C. liquoris, C. ljungdahlii, C. longisporum, C. lundense, C. luticellarii, C. magnum, C. malenominatum, C. massiliodielmoense, C. maximum, C. merdae, C. moniliforme, C. neonatale, C. neuense, C. nitrophenolicum, C. novyi, C. oceanicum, C. oryzae, C. paraputrificum, C. pascui, C. pasteurianum, C. peptidivorans, C. perfringens, C. phoceensis, C. polyendosporum, C. polynesiense, C. proteolyticus, C. psychrophilum, C. punense, C. puniceum, C. putrefaciens, C. quinii, C. ragsdalei, C. roseum, C. saccharobutylicum, C. saccharoperbutylacetonicum, C. sardiniense, C. sartagoforme, C. saudiense, C. scatologenes, C. schirmacherense, C. senegalense, C. septicum, C. sordelli, C. sporogenes, C. subterminale, C. sulfidigenes, C. swellfunianum, C. taeniosporum, C. tagluense, C. tarantellae, C. tepidiprofundi, C. tepidum, C. tertium, C. tetani, C. tetanomorphum, C. thermobutyricum, C. thermopalmarium, C. thermophilus, C. thiosulfatireducens, C. tunisiense, C. tyrobutyricum, C. uliginosum, C. uzonii, C. ventriculi, C. vincentii, C. vulturis, [Butyribacterium] methylotrophicum
.
Clostiridia C. sporogenes
and others have active proteolytic enzymes and are able to use proteins and peptides as substrates, hydrolyzing them to amino acids and then subjecting the latter to fermentation. Such clostridia belong to the group of proteolytic clostridia.
Formerly clinically important species Clostridium perfringens
called
Clostridium welchii
.
Changes in the composition of the genus Clostridium
In recent years, clostridia have been seriously reclassified, in particular:
The most important clinically important species is Clostridium difficile
was transferred to the newly created genus
Clostridioides
of the family
Peptostreptococcaceae
and was given the name
Clostridioides difficile
.
Clostridium mangenotii
was transferred to the same genus .
Species Clostridium litorale
moved to the genus
Peptoclostridium
of the same family
Peptostreptococcaceae
and renamed
Peptoclostridium litorale.
Species Clostridium sticklandii
moved to the genus
Acetoanaerobium
of the family
Peptostreptococcaceae
and renamed
Acetoanaerobium sticklandii
.
Species Clostridium dakarense
moved to the genus
Romboutsia
of the family
Peptostreptococcaceae.
Clostridium hiranonis, Clostridium paradoxum,
and
Clostridium thermoalcaliphilum
, their modern names: [
Clostridium
]
hiranonis
, [
Clostridium
]
paradoxum
and [
Clostridium
]
thermoalcaliphilum
, transferred to the family
Peptostreptococcaceae
without specifying a genus.
Species Clostridium histolyticum
was moved to the genus
Hathewaya
of the family
Clostridiaceae
and given the name
Hathewaya histolytica.
Clostridium limosum
and
Clostridium proteolyticum
were transferred to the same genus with the name changed to
Hathewaya limosa
and
Hathewaya proteolytica
, respectively.
Species Clostridium ramosum
moved to the genus
Erysipelatoclostridium
, family
Erysipelotrichaceae
, order
Erysipelotrichales
, class
Erysipelotrichia
and given the name
Erysipelatoclostridium ramosum
.
Species Clostridium aerotolerans, Clostridium aldenense, Clostridium algidixylanolyticum, Clostridium aminophilum, Clostridium amygdalinum, Clostridium asparagiforme, Clostridium bolteae, Clostridium celerecrescens, Clostridium citroniae, Clostridium clostridioforme, Clostridium fimetarium, Clostridium glycyrrhizinily ticum, Clostridium herbivorans, Clostridium hylemonae, Clostridium indolis, Clostridium lavalense, Clostridium methoxybenzovorans, Clostridium polysaccharolyticum, Clostridium populeti, Clostridium saccharolyticum, Clostridium scindens, Clostridium sphenoides, Clostridium symbiosum, Clostridium xylanolyticum
were transferred to the genus
Lachnoclostridium
of the family
Lachnospiraceae
and they are currently called [
Clostridium
]
aerotolerans
, [
Clostridium
]
aldenense
, [
Clostridium
]
algidixylanolyticum
, [
Clostridium
]
aminophilum
, [
Clostridium
]
amygdalinum
, [
Clostridium
]
asparagiforme
, [
Clostridium
]
bolteae
, [
Clostridium
]
celerecrescens
, [
Clostridium
]
citroniae
, [
Clostridium
]
clostridioforme
, [
Clostridium
]
fimetarium
, [
Clostridium
]
glycyrrhizinilyticum
, [
Clostridium
]
herbivorans
, [
Clostridium
]
hylemonae
, [
Clostridium
]
indolis
, [
Clostridium
]
lavalense
, [
Clostridium
]
methoxyben zovorans
,
Lachnoclostridium phytofermentans
, [
Clostridium
]
polysaccharolyticum
, [
Clostridium
]
populeti
, [
Clostridium
]
saccharolyticum
, [
Clostridium
]
scindens
, [
Clostridium
]
sphenoides
, [
Clostridium
]
symbiosum
, [
Clostridium
]
xylanolyticum
, respectively.
Eubacterium moniliforme species
and
Eubacterium tarantellae
are transferred from the genus
Eubacterium
and named
Clostridium moniliforme
and
Clostridium tarantellae
.
On the website GastroScan.ru in the “Literature” section there is a subsection “Microflora, microbiocenosis, dysbiosis (dysbacteriosis)”, containing articles addressing the problems of microbiocenosis and dysbiosis of the human gastrointestinal tract. Back to section
Classification
To date, more than one hundred species of clostridia have been identified. In medicine, their classification is based on several principles. Based on morphology, the following groups are distinguished:
- rods with a round, terminal spore (C. tetani);
- rods with an oval subterminal spore (C. botulinum);
- with a subterminal or centrally located oval spore (causative agents of gas gangrene).
By type of pathological processes:
- enteral clostridioses (C. botulinum, C. perfringens, C. difficile);
- traumatic and post-traumatic (C. tetani, C. perfringens, C. novyi, C. histolyticum, C. septicum);
- generalized infections: septicemia , sepsis .
Clostridium novyi
Clostridium novyi is one of the main causative agents of gas gangrene. During the Great Patriotic War, gas gangrene was caused by bacteria of this type in 42% of cases. The pathogen was first isolated and given the name Clostridium oedematiens by E. Segen and M.V. Weinberg in 1891. Later, this type of clostridia was more fully described by the American bacteriologist F. Novi, whose name later began to be called this type of bacteria.
Morphology of Clostridium novyi
Clostridia are rods, large, sometimes slightly curved, measuring 4 - 22 x 1.4 - 2 microns, mobile, have up to 25 flagella, often arranged in chains. The pathogen, like all clostridia, are obligate anaerobes. A capsule is not formed. Gram-stained violet (Gram-positive). Old cultures are losing this ability. They form oval spores located centrally and subterminally.
Rice. 14. Clostridium novyi. Large sticks, arranged singly or in chains.
Cultivation
Clostridium novyi are strict anaerobes. Highly sensitive to oxygen. They grow on simple media: carbohydrate, casein and meat peptone.
- When growing on solid media, translucent, juicy grayish colonies are formed after 48 hours. The edges are uneven. The surface is grainy. Clostridia types A, B and C sometimes form daughter colonies. The colonies are surrounded by a zone of hemolysis. Clostridia type D does not destroy red blood cells.
In the depths of the agar, colonies resemble lumps of cotton wool or snow flakes, often colored brown or yellow.
- When growing in liquid media, gas is formed and the nutrient medium becomes cloudy, and sediment falls to the bottom. The pH shifts to the acidic side due to the formation of H2S and organic acids.
Antigenic structure
Clostridium novyi is identified by the detection of somatic antigens. There are 4 serovars, different in antigenic characteristics and synthesized toxins - serovars A, B, C and D.
Biochemical properties
Serovars types A, B and C ferment fructose, glucose and maltose; serovars type D ferment only glucose. Serovars types A, C and D degrade glycerol. All strains curdle milk and break down gelatin. Type D clostridia produce hydrogen sulfide and indole, other types of bacteria do not.
Clostridium novyi toxins
Clostridium novyi produces a pathogenic enzyme such as phospholipase (a-toxin), as well as b, y, sigma, e and n - toxins that have necrotic, hemolytic and lethal effects. By disrupting the permeability of blood vessels, they lead to the development of jelly-like edema.
Rice. 15. The photo shows gas gangrene.
Causes
Normally, clostridia are present in the intestinal microflora in adults and children. Clostridia in the feces of an adult should not exceed 105 CFU/g. But, if they are activated and, accordingly, multiply too quickly, this leads to a deterioration in well-being and the development of the disease. The activation of these bacteria can be triggered by some external and internal factors:
- Consumption of low-quality food - stitched, low-quality, spoiled products, as well as fast food and other junk food.
- Regular stressful situations.
- Unfavorable environmental conditions.
- Constant lack of sleep, insomnia .
- Weakened immunity .
- Taking antibiotics, hormonal drugs, immunosuppressants.
- Intestinal infections.
- Immaturity of the central nervous system.
- Frequent colds, flu .
- Surgical operations.
Epidemiology
To date, about 80 species of bacteria of the genus Clostridium have been described. The cause of gas gangrene in humans is only pathogenic species of clostridia: Clostridium perfringens (70 - 80% of all cases of the disease), Clostridium novi and Clostridium septicum. Other types of pathogenic bacteria of the genus Clostridium have also been described, but they are much less common. All microorganisms are obligate anaerobes - they grow and reproduce in the absence of oxygen.
Under unfavorable conditions, bacteria form spores. They can remain in this state for a significant amount of time. The spores are resistant to sunlight, drying and high temperature. The growth and development of clostridia occurs only under anaerobic conditions. Humans and all types of animals are susceptible to the disease.
Sources of infection
Clostridia are constantly present in the soil, intestines of humans and herbivores; in some cases, with poor hygiene, bacteria can be found on the skin.
Transmission routes
Gas gangrene develops when clostridia infect extensive crushed wounds (gunshot wounds, lacerations, bruises), most often the lower extremities and torso, and wounds of the large intestine. Bacteria penetrate damaged tissues with soil, dust, through scraps of clothing, shell fragments, during surgical interventions, drug injections, and out-of-hospital abortions. In mine and transport injuries, injuries often occur in the buttocks and thighs. Persons injured by cattle, pigs, sheep and goats are susceptible to the disease. The wounds become contaminated with animal dung. In some cases, the disease develops from small but contaminated cuts. The disease develops quickly. Its first signs appear from the first day of injury.
Rice. 2. 90% of all cases of gas gangrene are caused by Clostridium perfringens.
Symptoms
Clostridiosis does not have a typical clinical picture. Manifestations depend on which system the pathological process began in. But still, several signs stand out that appear regardless of the type of pathogen:
- Increased body temperature – it can reach 39 degrees.
- The appearance of sharp abdominal pain of a spastic nature. When palpation is performed, the pain becomes more pronounced, the walls of the abdominal cavity become tense.
- Flatulence , bloating.
- Weight loss due to lack of appetite and deterioration in health.
- Diarrhea , blood and parts of food are sometimes detected in liquid stool.
- Nausea, frequent vomiting, sometimes the presence of blood in the vomit.
Clostridiosis difficile develops as pseudomembranous colitis, in more rare cases - diarrheal syndrome or necrotizing enterocolitis.
As a type of pseudomembranous colitis, the disease most often develops in newborns and infants. The disease begins acutely - the body temperature rises, the child spits up, vomits, and diarrhea syndrome develops. Watery stools contain mucus and sometimes blood. Often the child defecates thick mucus with fibrous patches. The stool may also be purulent. The skin takes on a gray-pale color, and a network of veins is visible on the abdomen. Children experience bloating and refuse to eat. Accordingly, babies lose weight. It is possible to develop bleeding in the intestines, which is an extremely life-threatening condition.
The disease is severe in newborns, especially in premature babies. Without proper treatment, death is possible.
Clostridium septicum
Clostridium septicum was first described in 1877 by L. Pasteur. These bacteria are opportunistic. Under normal conditions, they reside in the human intestine and do not cause disease. In the case of intestinal defects, such as colorectal cancer, the infection damages the intestines and spreads through the blood (hematogenously) throughout the body. Unlike Clostridium perfringens, gas gangrene can occur without prior injury or damage. The infection is more common in people with injuries and burns of the skin, after surgery and septic abortions, peripheral vascular diseases, diabetes, and colon cancer.
The disease develops quickly. Up to 80% of adults die within the first 2 days. Survival rates increase in individuals without concomitant diseases of the lower extremities.
Clostridium septicum affects both humans and domestic animals: large and small livestock.
Morphology
Clostridium septicum is a rod-shaped bacterium. with dimensions 3 - 4 x 1.1 - 1.6 microns. In cultures, filamentous forms of bacteria are sometimes formed, up to 50 microns in length. Motile (have flagella). A capsule is not formed. Gram positive. Over time, clostridia lose this feature. They are strict anaerobes.
Clostridium septicum produces spores. The spores are most often located subterminally, less often - centrally.
Rice. 16. Clostridium septicum under a microscope.
Cultural properties
Clostridium septicum grows well on casein and meat media supplemented with glucose.
- On the surface of glucose-blood agar, bacteria form translucent colonies, shiny, consisting of intertwined threads with a zone of hemolysis along the periphery.
- When growing on 2% agar, the colonies have the appearance of disks.
- When growing on Zeissler agar, after 48 hours, a continuous, delicate coating forms with a zone of hemolysis along the periphery.
- When grown in 1% sugar agar, colonies form in depth. They have a dense center, with intertwining threads extending from the periphery.
- When growing in meat peptone broth, a uniform cloudiness is formed. Further, loose sediment and gas formation are observed.
- When growing on Kitta-Tarozzi medium, bacteria grow with intense gas formation.
Rice. 17. When growing in 1% sugar agar, colonies form in depth. They have a dense center, with intertwining threads extending from the periphery.
Antigenic structure
Clostridium septicum has H and O antigens. The H antigens identify 6 serovars: A, B, C, D, E and F.
Biochemical properties
Clostridium septicum synthesizes a number of enzymes. They live on various organic substrates, including those containing sugars and amino acids, releasing carbon dioxide and molecular hydrogen.
Bacteria ferment some carbohydrates: glucose, maltose and lactose, producing gas and acid. Nitrates are converted to nitrites. They break down proteins releasing ammonia and hydrogen sulfide. Milk curdles slowly under the influence of bacteria. They do not decompose sucrose, glycerin and mannitol. They do not form indole.
Tests and diagnostics
To make a diagnosis, a specialist must study the patient’s medical history, paying attention to whether antibiotic therapy was carried out.
A laboratory test of stool is required to check for the presence of Clostridium difficile and their toxins. If necessary, an endoscopic examination of the large intestine is performed, which reveals characteristic signs - yellowish plaques on the mucosa, a thick layer of overlays, ulcerated areas, which can be important in the process of differential diagnosis. Radiography may be performed.
A blood test is also performed, in which nonspecific changes are noted in the manifest forms of infection.
Prevention
To avoid clostridiosis, you must adhere to the following preventive measures:
- Do not take broad-spectrum antibiotics without a doctor’s prescription, especially for long courses. The risk of clostridiosis increases especially strongly when using ampicillin and aminoglycosides (enteral forms).
- It is important to maintain good hygiene.
- It is necessary to properly process food thermally and not eat spoiled or expired foods or canned food.
Diet
Diet for intestinal dysbiosis
- Efficacy: therapeutic effect after 15-21 days
- Time frame: 1-2 months
- Cost of food: 1280-1360 rubles per week
If an adult or child is undergoing treatment for an illness caused by clostridia, he must adhere to a special diet.
It is important to exclude the following foods from your diet:
- Those that have a laxative effect: legumes, cabbage, beets, dried apricots, prunes, etc.
- I love any kind of preservation.
- Pickled and spicy foods.
- Fast food, any sausages.
- Mushrooms, onions, garlic, radishes, radishes.
- Fried, fatty foods.
- Sweets, soda.
- Alcoholic drinks.
The following products and dishes must be included in the menu:
- Those that have a binding effect: raisin decoction, rice, bananas, etc.
- Products with lactic acid bacteria: yogurt, kefir.
The diet can be composed of the following products:
- Meat and fish of lean varieties.
- Boiled and baked vegetables, herbs.
- Non-acidic berries and fruits.
- Eggs.
- Cereals.
- Vegetable oils.
You need to eat in small portions and often. Avoid very hot and very cold foods.
List of sources
- Atlas of medical microbiology, virology and immunology: Textbook for students of medical universities / Ed. A. A. Vorobyova, A. S. Bykova. - M.: Medical Information Agency, 2003. - P. 66. - 236 p. — ISBN 5-89481-136-8.
- Kovaleva E.P., Semina N.A., Semenenko T.A., Galkin V.V. Handbook of Hospital Epidemiologists. – M.: Chrysostom, 1999. – P. 136–139.
- Medical microbiology./ Ed. V.I. Pokrovsky, O.K. Pozdeev. – M: GEOTAR MEDICINE, 1999.
- Uchaikin V.F., Nisevich N.I., Shamsheva O.V.. Infectious diseases in children: textbook. - M.; GEOTAR-Medka, 2011.-688 p.. 2011