Sometimes this occurs as a result of suppuration or inflammation at the scar site. In other cases - if the resulting connective tissue turns out to be weak due to concomitant diseases or metabolic disorders, which lead to diabetes mellitus, rheumatological diseases, and hereditary pathology of connective tissue.
Statistics show that postoperative hernias occur in 6-8% of patients who have undergone laparotomy or lumbotomy interventions. In 50% of patients, a hernia occurs within the first year after surgery, in all others within 5 years after that. Hernias often appear after emergency interventions, during suppuration of a surgical wound, or after major oncological operations. However, they can also occur after laparoscopic operations at the sites where trocars are installed or at the site of removal of a removed tumor or organ.
The problems of treating postoperative hernias are not always competently covered in the wider literature and on Internet sites. “Awareness” of the population about unsuccessful treatment results and their own negative experience of rehabilitation after the first surgery lead to the fact that many patients with postoperative hernias refuse planned surgical treatment for a long time. This helps to lengthen the time of herniation. At the same time, the size of the hernia increases, an adhesive process develops in the abdominal cavity, and irreversible changes occur in the tissues of the abdominal wall and in those organs that find themselves in an unnatural anatomical position. All of the above significantly worsens treatment results.
Some aspects of terminology
In any hernia, the hernial sac, hernial contents and hernial orifice are distinguished.
- A hernial sac
is a stretched section of the peritoneum, which, together with the internal organs, has emerged through a defect in the abdominal wall and covers them. With postoperative hernias, “multi-chamber” hernias often occur, when the scar has not one, but several adjacent defects. - Hernial contents
are those organs or parts thereof that have extended beyond the abdominal cavity. - Under hernial orifice
understand the hole itself or defect in the abdominal wall, through which the hernia subsequently emerges.
Diagnostics
Diagnostic measures include surgical examination with palpation and a number of laboratory and instrumental studies:
- Abdominal ultrasound
- Irrigoscopy
- Survey X-ray
- Herniography
- Blood and urine tests
To clarify some parameters, it may be necessary to prescribe MSCT or MRI of the abdominal cavity, colonoscopy and other examination methods.
You have questions? We will be happy to answer any questions Coordinator Tatyana
Why do postoperative hernias form?
Many factors contribute to the formation of a postoperative hernia. An important point in their occurrence is a violation of the dynamic balance between the pressure inside the abdomen and the ability of the abdominal walls to counteract it.
Factors in the formation of hernias.
- Predisposing factors include:
individual characteristics of each individual person - such as heredity, nutritional status, age, concomitant diseases and metabolic disorders. In some connective tissue diseases, for example, in Marfan syndrome, tissue weakness occurs and weak scars form at the site of the operation. Often weak connective tissue is formed due to malnutrition, in old people, and with cancer or rheumatological diseases. Diabetes mellitus and obesity also lead to slower scar formation.
- Producing factors
may be diseases or conditions of a person that lead to a significant increase in intra-abdominal pressure (bronchial asthma, chronic bronchitis with persistent cough, prolonged constipation, difficulty urinating due to problems with the prostate gland, pregnancy and childbirth, physical labor or sports activities associated with lifting and carrying severity. Under normal conditions, the formation of a durable scar occurs within 2.5-3 months, and its final organization - by 12 months. Untimely and, most importantly, a sharp increase in physical activity on an unformed scar leads to a decrease in its strength and the formation of hernias in the first year after surgery.
- There are also local factors
, which affect the healing of postoperative wounds and can cause the formation of a hernia. Inflammation (and especially suppuration) of a postoperative wound can have a significant effect on the scar, making it unreliable and fragile, increasing the risk of a hernia. This also leads to intolerance by the patient’s body to suture material. The resulting inflammatory reaction to the threads often leads to the formation of ligature fistulas, and subsequently to the appearance of defects in the postoperative scar. Now there are a large number of modern threads created on the basis of bioinert materials, which practically do not cause inflammation or rejection reactions. Impaired tissue restoration and a decrease in scar strength are also provoked by technical errors in closing the surgical wound (gross tissue trauma, non-compliance with the anatomical sequence of their connection, poor hemostasis) or the need to leave tampons or drains, which is more common in emergency surgery in the presence of purulent-inflammatory diseases.
Sources
- Romain B., Fabacher T., Ortega-Deballon P., Montana L., Cossa JP., Gillion JF., Antor R., Beck M., Barrat C., Berney C., Binot D., Bousquet J., Blazquez D., Bonan A., Cas O., Champault-Fezais A., Chastan P., Chollet JM., Cossa JP., Dabrowski A., Delaunay T., Démaret S., Drissi F., Demian H., Dubuisson V., Dugue T., Fromont G., Gillion JF., Jacquin C., Jurczak F., Khalil H., Launay-Savary M., Lepère M., Lépront D., Longeville JH., Le Toux N. , Loriau J., Magne E., Ngo P., Oberlin O., Passot G., Pavis d'Escurac X., Putinier JB., Renard Y., Romain B., Soler M., Roos S., Thillois JM ., Tiry P., Vu P., Verhaeghe R., Warlaumont M., Zaranis C. Longitudinal cohort study on preoperative pain as a risk factor for chronic postoperative inguinal pain after groin hernia repair at 2-year follow-up. // Hernia - 2022 - Vol - NNULL - p.; PMID:33891224
- Santos DA., Zhang L., Do KA., Bednarski BK., Robinson Ledet C., Limmer A., Gibson H., You YN. Chemotherapy and Abdominal Wall Closure Technique Increase the Probability of Postoperative Ventral Incisional Hernia in Patients With Colon Cancer. // Am Surg - 2021 - Vol - NNULL - p.31348211011149; PMID:33877925
- Min JS., Seo KW., Jeong SH., Kim KH., Park JH., Yoon KY., Kim TH., Jung EJ., Ju YT., Jeong CY., Kim JY., Lee YJ. A comparison of postoperative outcomes after open and laparoscopic reduction of Petersen's Hernia: a multicenter observational cohort study. // BMC Surg - 2022 - Vol21 - N1 - p.195; PMID:33858393
- Du Z., Wei SW., Zhang XY., Xiang Z., Qu SQ. The effect of dexmedetomidine premedication on postoperative systemic inflammatory response in children undergoing hernia repair surgery: A randomized controlled trial. // Paediatr Anaesth - 2022 - Vol - NNULL - p.; PMID:33825304
- Danneberg S., Sayk F., Marquardt JU. [61/m-Postoperative wound healing disorder after umbilical hernia repair and unclear elevation of transaminases: Preparation for the medical specialist examination: part 41]. // Internist (Berl) - 2022 - Vol - NNULL - p.; PMID:33822244
- Yörükoğlu H.U., İçli D., Aksu C., Cesur S., Kuş A., Gürkan Y. Erector spinae block for postoperative pain management in lumbar disc hernia repair. // J Anesth - 2022 - Vol - NNULL - p.; PMID:33751203
- Espinosa-de-Los-Monteros A., Frias-Frias R., Alvarez-Tostado-Rivera A., Caralampio-Castro A., Llanes S., Saldivar A. Postoperative Abdominal Bulge and Hernia Rates in Patients Undergoing Abdominally Based Autologous Breast Reconstruction: Systematic Review and Meta-Analysis. // Ann Plast Surg - 2022 - Vol86 - N4 - p.476-484; PMID:33720921
- Rodoman GV., Malgina NV., Razbirin VN., Epiphanova SV., Dolgina TY., Kuznetsov AI. . // Khirurgiia (Mosk) - 2022 - Vol - N3 - p.36-41; PMID:33710824
- Seher N., Nayman A., Koplay M., Çiftci İ. Comparison of Preoperative and Postoperative Testicular Elasticity and Vascularity in Pediatric Patients with Inguinal Hernia. // J Ultrasound Med - 2022 - Vol - NNULL - p.; PMID:33665883
- Schaaf S., Willms A., Schwab R., Güsgen C. Recommendations on postoperative strain and physical labor after abdominal and hernia surgery: an expert survey of attendants of the 41st EHS Annual International Congress of the European Hernia Society. // Hernia - 2021 - Vol - NNULL - p.; PMID:33629178
Classification of postoperative hernias
Hernial protrusions are classified by size. Highlight:
- a small postoperative hernia,
which is located in any one area of the abdomen and does not change its configuration. Determined only by palpation or ultrasound examination with the size of the hernial orifice up to 5 cm; - medium postoperative hernias
, which occupy part of one area of the abdomen with the formation of a visible protrusion and the size of the hernial orifice from 5 to 10 cm; - large postoperative hernias,
completely occupying any area of the anterior abdominal wall, changing the shape of the abdomen, with the size of the gate from 10 to 15 cm; - giant postoperative hernias
, occupying two or three areas of the abdomen or more, sharply deforming the abdomen, interfering with everyday life, with the size of the hernial orifice more than 15 cm. In 2006, the Society of Herniologists of Russia recommended adhering to the SWR Classification, recognized in Madrid at the XXI International Congress herniologists.
This classification takes into account three main parameters: the localization of the hernia in relation to the navel (median, lateral and combined), the size of the hernia orifice and the presence of relapses.
The share of postoperative ventral hernia is 6-8% of all hernias of the anterior abdominal wall. Due to the steady annual increase in the number of laparotomies, there is an increase in the number of patients suffering from this disease. According to consolidated data from a number of domestic authors, such a hernia occurs in approximately 500 thousand people in Russia [3, 4]. A postoperative hernia causes atrophy and flabbiness of the muscles, thinning of the aponeurosis, sharply disrupts the function of both the abdominal wall and the abdominal organs, which leads to frequent cases of temporary disability, and often (with a large and giant hernia) to the disability of patients. The well-known medical aphorism “a disease is easier to prevent than to treat” best suits the problem of preventing postoperative ventral hernia [18].
Currently, prevention is carried out in four areas. The first and most studied are the prevention and treatment of complications in the early postoperative period. During operations on the abdominal organs, it is necessary to strictly observe the rules of asepsis and antisepsis to prevent infectious material from entering the surgical wound, to carry out thorough hemostasis, and to exclude unnecessary drainage and packing of the abdominal cavity through the wound [24, 35].
It is necessary to rationally choose an surgical approach that excludes the intersection of nerve trunks, carefully suturing the wound layer by layer with modern biocompatible (no toxic, allergenic, carcinogenic and teratogenic effects on the body) suture material.
In the early postoperative period, it is necessary to prevent an increase in intra-abdominal pressure due to vomiting, coughing, urinary retention, and bloating, as this creates an increased load on the sutures of the abdominal wall and often leads to the development of eventration. Dosed compression of the wound using an elastic, air-permeable bandage prevents increased stress on the sutures and promotes the formation of a durable postoperative scar [38, 39].
The second direction is to stimulate reparative processes in the wound. For this purpose, the timely elimination of hypoproteinemia, anemia, vitamin deficiency, and candidiasis is essential. Glucocorticoids, sulfonamides and antibiotics should be used rationally, since these drugs can cause depression of reparative processes. Some authors propose the introduction of fibrinogen, cryoprecipitate, bone marrow cells into the deep layers of the wound (subaponeurotic, interaponeurotic, intermuscular) during the repair phase of the wound process, which contributes to the early induction of fibroplastic activity and the formation of a durable connective tissue scar adapted to specific conditions [5, 10].
The third direction is the optimization of methods for closing a laparotomy wound with local tissues. The technique of closing the abdominal wall is one of the most important factors in the prevention of postoperative hernia. There is still no definitive opinion on the best method of closing a laparotomy wound. The success of surgical intervention largely depends on the properties of the suture materials used in its implementation. The main requirements for a suture thread: biocompatibility, smooth surface, high handling properties, minimal wicking effect [11]. A promising direction is the introduction into surgical practice of biologically active suture materials - threads, which include substances that have the ability to have a biological effect when implanted into tissue. Antimicrobial suture threads containing the antiseptic triclosan are most often used abroad [31, 37]. In
vitro
and
in vivo
studies have proven their pronounced and prolonged effect on a wide range of microorganisms [32]. Domestic suture materials with the antibiotic doxycycline and the fluoroquinol drug ciprofloxacin also showed high antimicrobial activity. The maximum portions of antibacterial drugs were released from the threads in the first 5-7 days, which provided the most intense effect on the course of the wound process [8]. In recent years, Russia has begun to use suture materials that not only have antimicrobial activity, but also stimulate regenerative processes. Stimulation of tissue repair is achieved by introducing organic compounds containing germanium into the structure of the thread shell. Suture material, which has antimicrobial and reparative activity, can reduce the number of purulent complications in the abdominal wall wound by 2 times compared to the control group of patients in which nylon threads were used [9].
The method of using suture material has a certain significance in the prevention of postoperative hernias. The tensile strength of interrupted sutures is 80% less than that of a continuous suture, so it is advisable to use a continuous suture for suturing the abdominal wall [29, 30].
Domestic and foreign surgeons propose to modify the existing methods of closing a wound of the abdominal wall with local tissues by using various technical techniques: creating a duplication of the aponeurosis, applying submersible two-story sutures, figure-of-eight and retention sutures [4, 35]. However, the use of any method of autoplasty of the abdominal wall does not lead to a reduction in the frequency of postoperative hernias, since it does not take into account changes in the abdominal wall due to sagging, muscle atrophy and degenerative processes in the aponeurotic structures. The preoperative weakness of the abdominal wall becomes even greater after surgical interventions [19].
The fourth direction is the primary closure of the laparotomy wound with a mesh endoprosthesis in order to prevent the occurrence of a postoperative hernia. This direction is the least studied, but the most promising. In Russia, most surgeons are reserved in this direction, believing that the main reasons for the development of a postoperative hernia are defects in the surgical technique for suturing the abdominal wall or wound purulent complications.
The first publications on preventive endoprosthetics appeared in foreign literature in the 70-80s of the last century. Until the middle of the first decade of the 21st century, this technology for strengthening the abdominal wall was used sporadically in coloproctology to prevent parastomal hernia, in vascular surgery after a complete midline laparotomy performed for an abdominal aortic aneurysm, in abdominal surgery in elderly and senile people suffering from obesity. Summarizing the results of these studies are presented in the previously published commentary by B.Sh. Gogia et al. [2].
The first subject of discussion is the determination of indications for preventive endoprosthetics of the abdominal wall. It should be emphasized that in the works of foreign authors there was no scientifically based system for determining indications for preventive endoprosthetics of the abdominal wall. This shortcoming was corrected in the works of domestic surgeons, in which a scale for quantitative assessment of risk factors for the development of postoperative hernia was presented [12].
A study of the effectiveness of predicting the development of postoperative ventral hernia using this scale in 93 patients who underwent midline laparotomy gave the following results. With a score of 0 to 5 (low risk), a postoperative hernia developed in 5.3% of cases, from 6 to 10 (medium risk) in 13.3%, from 11 to 15 (high risk) in 17.3% and from 16 and above (extremely high risk) - in 30% of cases [16].
In the first place among the indications for preventive endoprosthetics is anatomical and functional insufficiency of the abdominal wall (weakness), which is manifested by sagging, ptosis of the abdomen with the formation of a skin-fat apron, a dome-shaped abdomen with pronounced diastasis of the rectus muscles, and the absence of a decrease in abdominal circumference with abdominal tension. Women are characterized by postoperative flabbiness in combination with abdominal ptosis, and men are characterized by a dome-shaped abdomen in combination with diastasis of the rectus muscles.
Ultrasound studies of the abdominal wall of patients before and after operations on the abdominal organs and retroperitoneal space made it possible to clarify the main mechanisms of development of its anatomical and functional insufficiency. Thus, damage was detected to all layers of the abdominal wall - skin, subcutaneous tissue, aponeurosis, muscles. The skin becomes flabby and thinner. The subcutaneous fatty tissue thickens, connective tissue develops in it, which leads to a change in its structure, which turns from homogeneous to lobulated. The aponeurotic layer becomes thinner, its structure becomes heterogeneous. The width of the white and Spigelian lines of the abdomen increases 2 times with mild and 4 times with severe anatomical and functional insufficiency. There is a thinning and expansion of the muscle layer of the abdominal wall by 1.5 times in case of mild and 2 times in cases of severe damage, with a decrease in the degree of narrowing and thickening of the muscles during tension by 2.5 and 3.5 times, respectively. The structure of the muscle layer loses its homogeneity, its echogenicity increases due to fatty and connective tissue degeneration. The following critical parameters were identified, indicating anatomical and functional insufficiency of the abdominal wall: heterogeneous structure of subcutaneous fatty tissue 5.2±0.4 cm thick with the appearance of connective tissue inclusions, width of the white line of the abdomen 2.2±0.09 cm, heterogeneous echostructure of the rectus muscles abdomen with increased echogenicity, thickness 1.35±0.04 cm and width 11.76±0.1 cm, with contractility of the rectus muscles at a tension of 20.7±1.0% of the initial value, width of the Spigel line 0.5±0 .04 cm, heterogeneous structure of the broad muscles of the lateral abdominal wall with increased echogenicity, thickness 1.3±0.1 cm and contractility 20.3±1% of the original value [12].
When conducting genetic studies in patients with and without a ventral hernia, it was established that the basis for the development of anatomical and functional insufficiency of the abdominal wall, which is directly proportional to the frequency of development of postoperative hernias, is a decrease in the functional activity of ribosomal genes [1].
Interesting data were obtained from polarization microscopy of the skin and aponeurosis in patients with and without abdominal hernia. It turned out that in patients with ventral hernia the ratio of collagen types I and III is sharply disturbed in the direction of increasing the content of collagen type III. When comparing genetic and histological data, it was established that the ratio of collagen types I and III in the skin and aponeurosis of less than 2.1 is associated with the mutant AA genotype in the EGF +61G/A gene polymorphism and the identification of a mutant allele of the 1117 5A/6A polymorphism of the matrix metalloproteinase 3 gene, which is a reliable prognostic criterion for the risk of developing a ventral hernia [7].
The second place is occupied by obesity in patients with a body mass index exceeding 30 kg/m2, which is clinically manifested by a significant increase in the size of the abdomen due to the excessive development of subcutaneous fatty tissue, the thickness of which exceeds 6 cm. In these patients, the lateral surface of the body is not tightened, the waist is absent. The centrally located tissues of the abdominal wall are flabby, the skin is stretched. On palpation, the abdominal wall is not elastic, muscle contractility is practically absent [2]. Reparative processes are especially severely disrupted during the development of metabolic syndrome (insulin resistance syndrome), which is manifested by abdominal obesity, type 2 diabetes mellitus, arterial hypertension and coronary heart disease. With this syndrome, the probability of developing a ventral hernia after laparotomy is 100% [23].
The third place among the indications for endoprosthetics is the age of patients. In elderly (over 60 years old) and especially senile (over 75 years old) patients, involution processes begin to develop in the connective tissue and muscle structures of the abdominal wall, and the intensity of reparative processes decreases. In addition, older patients have other risk factors: constipation, difficulty urinating, chronic respiratory failure, abdominal aortic aneurysm. The incidence of the disease is directly dependent on age: the older the patient, the more often a postoperative hernia develops. All this suggests that when performing a wide median laparotomy in elderly and senile patients, one should resort to preventive endoprosthetics of the abdominal wall [20].
One of the indications for the primary closure of a laparotomy wound with a mesh endoprosthesis should be considered repeated laparotomy, which is an important predictor of the development of a postoperative ventral hernia. According to a number of authors, repeated surgery in the same anatomical zone of the abdominal wall, where a primary laparotomy was previously performed, reduces the vascularization of the scar in the fascia area, increases the likelihood of bacterial contamination of the wound, and impairs its healing [27]. A study conducted by domestic surgeons found that postoperative hernia develops 2 times more often during reoperation than in patients who underwent a median laparotomy for the first time [16].
One of the problems in the treatment of widespread peritonitis is the development of a postoperative hernia in the majority of patients who have undergone wide midline laparotomy with programmed sanitation of the abdominal cavity [33]. The development of a systemic inflammatory reaction and abdominal sepsis, intra-abdominal hypertension syndrome, enteral insufficiency, endothelial dysfunction and oxidative stress during peritonitis sharply inhibits the healing processes of the laparotomy wound. We studied the effect of closing a laparotomy wound in widespread peritonitis with a polypropylene mesh on the results of treatment of patients. Of the 45 cases in which this technology was used to close the abdominal wall wound, none observed eventration in the immediate postoperative period or the development of a postoperative hernia in the long term [14].
Studies conducted in recent years have found that the incidence of postoperative ventral hernias in cancer patients after laparotomy ranges from 18.6 to 44.4%, depending on the location of the primary tumor [6]. Chemotherapy, radiation therapy and the number of laparotomies in a patient have a statistically significant effect on hernia formation. During operations performed against the background of radiation and/or chemotherapy, the authors recommend closing the laparotomy wound using autodermal lacing, which, in their opinion, helps reduce the incidence of postoperative ventral hernias [5]. In the foreign literature, we found the only publication devoted to the study of the quality of life of patients after oncological operations on the abdominal organs, which indicates that the formation of a postoperative hernia is a negative factor and substantiates the need for preventive endoprosthetics of the abdominal wall [21].
The second subject of discussion is the choice of prosthesis for preventive endoprosthetics. Studies of the late tissue reaction to implantation of various polypropylene prostheses into the abdominal wall have shown that their biocompatibility depends on the thickness of the thread. Around a standard polypropylene endoprosthesis with a thread thickness of 120 microns, in the late stages of implantation, a coarse fibrous deformed capsule with a predominance of giant cells of foreign bodies is formed. In the long-term postoperative period, as a result of mesh wrinkling, the mobility of the abdominal wall is limited, which causes a sensation of a “foreign body” at the implantation site in 5-10% of patients [18]. When studying the late tissue reaction of the abdominal wall to the implantation of a lightweight polypropylene prosthesis with a thread thickness of 90 microns, it was found that the endoprosthesis is completely overgrown with connective tissue 2-4 months after implantation. The connective tissue capsule around the light prosthesis also contains giant cells of foreign bodies, but in smaller quantities, which, when strengthening the intact tissues of the abdominal wall, can cause an inflammatory reaction in them. A super-light endoprosthesis with a thread thickness of 70 microns after 2 months is surrounded by a very thin connective tissue capsule with a minimal number of cellular elements and a predominance of fibrous structures, which does not cause inflammatory changes in the abdominal wall and is the optimal material for its preventive endoprosthetics [15].
The third point of discussion is the placement options for the prosthesis. When plasticizing the midline of the abdomen after emergency surgery for an acute inflammatory process of the abdominal cavity with a transition to the parietal peritoneum, it is advisable to place a mesh implant over the aponeurosis, which reduces the risk of infection during the intervention, is simpler than other options and only slightly increases the duration of the manipulation. The prosthesis applied to the aponeurosis should be 4 cm longer and 5-6 cm wider than its suture line, since this is enough to eliminate tissue tension. It is recommended to fix the endoprosthesis with interrupted sutures to the aponeurosis along its entire length in a checkerboard pattern. This makes it possible, in case of relaparotomy, to cut the endoprosthesis at the beginning of the operation and stitch it at the end [12, 33]. Unfortunately, the supraponeurotic location of the prosthesis is accompanied by the development of seromas, which requires long-term drainage of the wound with active aspiration [26].
In planned abdominal surgery, after performing a median laparotomy to strengthen the linea alba, it is advisable to place the prosthesis under the aponeurosis, which is more justified from the pathogenetic point of view of the development of a postoperative hernia. It should be emphasized that the subaponeurotic placement of the prosthesis is much more technically complex and increases the duration of the operation. A positive point is the absence of seromas at the site of implantation of the prosthesis [4, 22, 28].
Subgaleal endoprosthetics should also be used for plastic surgery of the lateral abdominal walls during urological surgery on the urinary tract and vascular operations on the abdominal aorta performed from a retroperitoneal approach. After completing the main stage of the operation, layer-by-layer suturing of the transverse and internal oblique muscles is performed from the lateral approach, edge to edge. An endoprosthesis is placed on top of the applied suture in the retromuscular space between the internal and external oblique muscles, which should be 4 cm longer and 3 cm wider on each side of the suture line. The prosthesis is fixed to the latissimus dorsi muscle, the sheath of the rectus abdominis muscle, the aponeurotic structures of the iliac crest and tissue in the area of the lower edge of the costal arch. In this way, the endoprosthesis covers the weak point of the abdominal wall - the Spigelian line and the dissected internal oblique muscle, which is most susceptible to atrophic degeneration due to the transverse intersection of its fibers. No wound drainage is required [13]. The subgaleal location of the prosthesis is used to prevent parastomal hernia in coloproctology [36].
In the presence of morbid obesity, diabetes mellitus, and anemia, some authors suggest intraperitoneal placement of the prosthesis using video-assisted support, which, in their opinion, reduces the risk of postoperative complications. To strengthen the abdominal wall, a composite endoprosthesis is used, consisting of polypropylene and polytetrafluoroethylene endoprostheses fixed to each other, the latter of which faces the abdominal organs [17].
Intra-abdominal fixation of endoprostheses can be carried out using herniostaplers and fibrin glue. The use of seamless technology for fixing polymer endoprostheses reduces the incidence of wound postoperative complications and ensures reliable fixation of endoprostheses to the tissues of the anterior abdominal wall. In the immediate postoperative period after preventive implantation of a polypropylene mesh, an intestinal fistula is formed in 3.5-5% of cases. In this regard, for intra-abdominal implantation it is advisable to use prostheses made of polytetrafluoroethylene, which do not cause adhesions in the abdominal cavity [39].
Currently, the results of the operation are assessed based on studying the quality of life of patients, which is directly dependent on the size of the postoperative ventral hernia: the larger the hernia, the worse the quality of life [34, 40, 43]. A number of foreign authors have conducted a comparative study of the quality of life of patients who underwent midline laparotomy in combination with and without preventive endoprosthetics. Observation during the first year after surgery showed a statistically significantly higher level of quality of life in patients who underwent primary wound closure with a mesh endoprosthesis [22, 25, 40—42].
Thus, preventive endoprosthetics is becoming increasingly widespread in abdominal and vascular surgery, coloproctology, urology, and oncology. Indications for the use of this technology for the prevention of postoperative ventral hernia are as follows: severe anatomical and functional insufficiency of the abdominal wall; obesity of III-IV degree in combination with or without metabolic syndrome, elderly and senile patients in combination with other risk factors; repeat laparotomy on the old surgical scar; closure of a laparotomy wound in patients with peritonitis and treated using programmed sanitation of the abdominal cavity; laparotomy against the background of neoadjuvant radiation and/or chemotherapy in patients with cancer. For preventive endoprosthetics, it is better to use super-light endoprostheses with a thread thickness of 70 microns. In the presence of an inflammatory process in the abdominal cavity, prostheses should be placed supraponeurotically, and in the absence of an infectious agent - subaponeurotically or intraabdominally, using endoscopic technologies.
Survey
Detecting a hernia is usually not difficult. Most often, a visual inspection and palpation of the protrusion is enough. If necessary, an ultrasound examination is performed.
However, when preparing for surgical treatment, it is necessary to conduct a full examination in order to identify and timely correct concomitant diseases that may become risk factors for hernia recurrence. And also evaluate the function of the respiratory and cardiovascular systems in order to choose the most suitable method of operation for each patient.
If difficulties arise in diagnosis - in case of complex multi-chamber hernias, when it is necessary to determine the topography of the hernia defect, measure the hernial orifice for individual selection of a mesh implant - an MRI of the abdominal organs is performed.
Do you want to get rid of a hernia quickly and permanently?
You're lucky to have found us. Contact us for advice.
- We will conduct an in-depth diagnosis of the condition of your abdominal cavity
- We will select for you the optimal treatment method from the entire range of modern high-tech surgical techniques
- Our highly qualified specialists - candidates and doctors of medical sciences - will perform the operation using the latest technologies, expensive specialized equipment and materials
- Your stomach will become healthy and beautiful, and traces of the intervention will be completely invisible to prying eyes
- We will carry out follow-up examinations and monitor your abdominal condition for six months to ensure there is no recurrence (free of charge)
Preoperative preparation
Necessary for patients with large and giant postoperative hernias, as well as in the presence of diseases that predispose to the occurrence of hernias. Preparation should include not only drug correction of concomitant diseases, but also preparation of the skin in the area of surgery (treatment of ligature fistulas, diaper rash, maceration); bowel preparation (constipation treatment); prevention of respiratory and cardiovascular complications, prevention of intra-abdominal hypertension syndrome. Most of the preparatory activities are carried out on an outpatient basis under the supervision of a therapist (cardiologist) and a surgeon.
Course of the disease
Postoperative hernias in the early stages are reducible and are not accompanied by pain. However, with sudden straining, falling, or lifting, pain appears and the protrusion increases. As the hernia progresses, the pain intensifies, sometimes becoming cramping in nature. At the same time, intestinal lethargy, constipation, flatulence, nausea, belching develop, the activity of patients sharply decreases, fecal stagnation, accompanied by intoxication, is periodically observed.
Treatment of postoperative hernia
The only way to treat any type of hernia, including postoperative ones, is surgical, the main task of which is to return the hernial contents into the abdominal cavity to the correct anatomical position and restore the integrity of the abdominal wall (that is, its plasticity). It is important to distinguish between two main types of abdominal wall plastic surgery.
1) Plastic surgery of the anterior abdominal wall using one’s own tissues (muscular-aponeurotic or fascial-aponeurotic).
The advantage of this method is the connection of homogeneous fabrics and the absence of the need to use synthetic materials. However, the possibility of its implementation depends on the size of the hernia gate and the condition of the tissues of the abdominal wall. Repair of a postoperative hernia with local tissues is only feasible if the defect size is small, less than 5 cm, there is no tissue tension, and the aponeurosis and muscle tissue are in good condition. If small postoperative hernias are repaired, local anesthesia is allowed; in other cases, anesthesia is given.
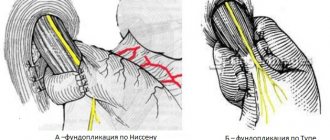
2) Prosthetic plastic surgery: plastic surgery with synthetic “mesh” implants, closing the aponeurosis defect in case of a postoperative hernia with a synthetic prosthesis.
The need to install an implant arises in the vast majority of cases of postoperative hernias. The implant can be installed either during complete suturing of the hernial orifice in order to strengthen the suture line, or to close the hernial orifice “without tension.”
Prosthetic hernioplasty is performed for recurrent hernias, in the presence of multiple hernia defects along the postoperative scar, in the presence of a systemic disease of connective and muscle tissues.
For large and giant postoperative hernias, in the presence of respiratory or cardiovascular failure, only “tension-free” methods of plastic surgery are used, when the mesh closes the hernial orifice in the form of a patch.
The mesh prosthesis is installed both traditionally after excision of the old postoperative scar, and laparoscopically through punctures on the lateral surfaces of the abdomen. For laparoscopic installation, special “anti-adhesive” mesh implants are used, which prevent the intestinal loops from “sticking” to the surface of the mesh. Such implants are selected individually depending on the size of the hernial orifice in the patient’s abdominal cavity. The advantage of the laparoscopic installation is faster recovery after surgery, less pain, the possibility of early activation and return to normal life. In addition, the risk of implant infection from inflammatory granulomas around the old suture material is eliminated. But there are a number of contraindications that exclude the choice of this method of operation.
You can receive detailed explanations and choose the optimal method of treating a postoperative hernia in each case by contacting our clinic for a consultation with the doctors of our surgical department. The clinic provides treatment for any hernia, including postoperative ones. Treatment of patients is carried out using various sources of financing: under compulsory and voluntary health insurance programs, and on a self-supporting basis.
Why surgery is needed
The only reliable way to get rid of the pathology is an operation with the installation of a mesh prosthesis - tension-free hernioplasty. All other methods of treatment (medicines, exercise therapy, traditional methods) are powerless. Such a hernia occurs due to insufficient conditions for the formation of a postoperative scar:
- Insufficient preoperative preparation (for emergency interventions).
- Defect in surgical technique (poor quality suture material, excessive tissue tension, broken suture, etc.).
- Long-term drainage or packing of the abdominal cavity.
- Violation of the postoperative regime (physical stress, diet violations, refusal to wear a bandage, etc.).
- Connective tissue pathologies.
- Diseases accompanied by tension in the abdominal wall (intestinal diseases, pneumonia, bronchitis, etc.).
Scar tissue defects can only be eliminated through surgery. Therefore, you should not delay your visit to the doctor; even the smallest hernia is dangerous due to strangulation and the development of life-threatening conditions, including blood poisoning.
Symptoms of pathology
A postoperative ventral hernia forms at the site of a scar in the operated area. It is impossible not to notice the pathology, as a characteristic protrusion appears. You can verify that it is a hernia in a fairly simple way: standing in an upright position, there is an increase in the protrusion; when lying down, the hernia will decrease.
In the early stages of formation, the hernia is practically invisible; during this period, the hernial contents can be reduced without surgical intervention. Subsequently, the size of the hernia begins to increase, causing discomfort and pain. That is why it is important to seek medical help as soon as even the slightest signs of pathology are detected.
A patient with a postoperative ventral hernia may experience symptoms such as:
- Attacks of nausea and vomiting.
- Heartburn and belching.
- Pain in the abdomen.
- Bloating.
- Constipation.
- Decreased activity, weakness.
A postoperative ventral hernia can develop complications and give rise to the development of perforation of the intestinal wall, blockage of the hernia, and intestinal obstruction. Complications of the pathology enhance its clinical picture. In this case, the symptoms listed above are accompanied by severe pain and the presence of blood clots in the stool.
How common are hernias of the white line of the abdomen?
The most common hernias are inguinal and umbilical, while hernias of the white line of the abdomen are much less common. This type of hernia mostly affects women after pregnancy and young men who engage in heavy physical activity.
There are many reasons for the formation of white line hernias.
The most significant factor may be genetic predisposition. Inherited physiological and anatomical failure of the connective tissue structures of the body can lead to stretching of the linea alba, the formation of ectasia (expansion) of the rectus abdominis muscles, which subsequently entails thinning of the fascia; dilatations and gaps form in it, through which the formation of a hernia is possible.
Metabolic disorders, diabetes mellitus and other pathological conditions of the body that lead to changes in metabolic processes can cause depletion of the connective tissue structure of the white line. There are many diseases that can lead to a tendency to herniation, as well as effects that lead to an increase in pressure in the abdominal cavity: accumulation of fluid in it, heavy physical activity, pregnancy, difficult childbirth, chronic lung diseases, chronic constipation .
Stages of formation of a hernia of the white line
The formation of this type of hernia occurs in several stages.
- At the earliest stage, usually invisible to the patient, preperitoneal adipose tissue protrudes through the slit-like defect in the connective tissue, forming a so-called preperitoneal lipoma.
- Following this, the peritoneum is stretched and a hernial sac is formed, which can be palpated. Subsequently, at the stage of an already formed hernia, other abdominal organs are involved: omentum, loops of the small intestine, umbilical-hepatic ligament, transverse colon. At this stage of an already formed hernia, absolutely all components of the pathological process can be detected: the hernial orifice and the hernial sac with hernial contents. The risk of strangulation of a hernial protrusion, as a very dangerous condition, directly depends on the shape and size of the hernial orifice, the size of which can vary from several millimeters to several centimeters and take the shape of an oval, circle or even a rhombus; Moreover, the smaller the gate, the higher the likelihood that the hernia will suddenly be strangulated.
It is rare, but it happens that the type of hernia described in this article reaches large sizes; in their total mass they are relatively small. Often, the formation of a hernia does not occur beyond the stage of preperitoneal lipoma, which does not cause pain, and without the influence of aggravating factors does not evolve in progression and does not spread beyond the boundaries of the white line.