- home
- general surgery
- Hiatal hernia
- Treatment methods
Laparoscopic operations for diseases of the esophagus, stomach and duodenum are distinguished by their delicacy and functionality. The enlarged image on the monitor allows you to perfectly visualize all the finest anatomical formations in this area - the vagus nerve, gastric vessels and fascial spaces for gentle surgery.
Laparoscopic operations to remove hiatal hernia (HH), minimal recovery time, more than 2000 operations performed on HH.
Hiatal hernia and reflux esophagitis
Video from the operating room. Laparoscopic correction of the hiatal hernia with a mesh implant using the author’s method
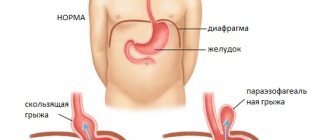
Hiatal Hernia (HH)
- pathological expansion of the esophageal opening of the diaphragm, in which the ligaments that fix the esophagus and stomach are stretched. As a result, the upper part of the stomach extends into the chest cavity and the functioning of the lower esophageal sphincter is disrupted. In this case, the patient begins to experience heartburn, especially at night in a horizontal position, pain in the chest, interruptions in the heart area, and a dry cough.
If there is no effect from drug therapy, surgical treatment is indicated, the essence of which is to restore normal anatomical relationships in the area of the esophagus and stomach.
The esophagus and upper part of the stomach are separated from the adhesions and brought down into the abdominal cavity to normal levels. I then perform a crurorrhaphy (reducing the hole in the diaphragm to normal size) and a fundoplication (creating a cuff from the stomach wall to prevent gastric contents from refluxing into the esophagus).
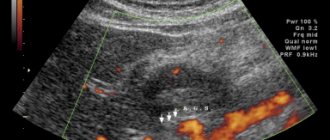
To identify the hiatal hernia and determine the extent of damage to the esophagus, as well as select the correct surgical treatment tactics, you must send me a complete description of gastroscopy, x-ray of the esophagus and stomach with barium for the hiatus, preferably an ultrasound of the abdominal organs, indicating your age and main complaints. In rare cases, if there is a discrepancy between complaints, X-ray data and FGS, it is necessary to perform daily pH measurements and manometry of the esophagus. Then I will be able to give a more accurate answer to your situation.
University
Nikolay Sivets , head of the surgical department of the 6th City Clinical Hospital of Minsk, professor of the department of military field surgery of BSMU, doctor of medicine. Sciences The essence of the operation is to correct the esophageal opening of the diaphragm and form a cuff from the fundus of the stomach around the abdominal esophagus and cardia. Interventions for hiatal hernia (HHH), as a rule, are performed using laparoscopic access, which reduces trauma, shortens the period of disability and speeds up rehabilitation.
Surgical treatment of hiatal hernia in the late postoperative period is accompanied by a fairly high percentage of relapses (from 11% to 30%). Good and excellent results are in the range of 84–86%. According to a number of authors, the relapse rate after laparoscopic correction of giant hiatal hernias (with a surface area of the esophageal opening of the diaphragm of more than 20 cm2) is 25–40%.
A characteristic feature of the operation: sutures are applied to the diaphragmatic legs that have already been separated from the fibers and have undergone degeneration. As a result, the diaphragm tissue erupts, creating conditions for the migration of the applied fundoplication cuff into the posterior mediastinum with the development of recurrent pathology. An attempt to apply sutures to intact tissue, while involving a large number of diaphragmatic crura, can lead to persistent postoperative dysphagia due to excessive narrowing of the esophageal opening of the diaphragm.
Specific mechanisms and types of relapses are well known: slipping of the fundoplication cuff, or telescope syndrome, displacement of the cuff into the chest cavity above the diaphragm, cutting through the sutures of the cuff or the sutures of the legs of the diaphragm, the formation of a paraesophageal hernia. Sliding of the fundoplication cuff above the diaphragm is most often observed when the crurorrhaphic suture fails. In second place is relapse due to rupture and disintegration of the diaphragmatic pedicle. The literature describes mechanical (manifested by dysphagia) and functional (manifested by heartburn) forms of relapse.
To improve the results of surgical treatment, plasty of the esophageal opening of the diaphragm is performed using a mesh implant. Many authors believe that the use of a mesh is advisable only for large sizes of the esophageal opening of the diaphragm, atrophy of the diaphragmatic legs and in old age. The attitude towards polypropylene mesh is currently very restrained. The limited use of them in plasty of the esophageal opening of the diaphragm is explained by frequent complications (long-term dysphagia in the postoperative period, cicatricial strictures, erosion of the esophagus by the implant and migration of the implant). At the same time, the indications for placing the mesh have not been worked out.
In repeated operations for recurrent hiatal hernias, Nissen fundoplication is used in approximately 70% of cases, and Toupet fundoplication is used in 17–20% of cases. Indications for re-intervention: recurrent hiatal hernia, especially if there is recurrent development of reflux, reflux esophagitis or other manifestations of gastroesophageal reflux disease (heartburn, dysphagia, vomiting, chest pain). It has been proven that with repeated operations their effectiveness decreases, and the greater the number of previously performed interventions, the lower the effectiveness of each subsequent one. This fact requires a careful approach to determining indications for refundoplication. To accurately determine whether reoperation is feasible, it is necessary to conduct a comprehensive clinical and X-ray endoscopic examination.
Patient V., 69 years old, resident of Polotsk, was hospitalized in the surgical department of the 6th City Clinical Hospital of Minsk on May 29, 2022 with a recurrent hiatal hernia.
From the anamnesis: in 2009 she was operated on in one of the clinics in Vitebsk. An endoscopic operation involving posterior crurorrhaphy was performed with the installation of a polypropylene mesh behind the esophagus and Nissen fundoplication. A year later, a recurrence of the hiatal hernia occurred, and the patient was operated on again in the same clinic. A left-sided thoracotomy and plasty of the esophageal opening of the diaphragm by suturing it were performed. About four years after the second operation I felt satisfactory. The deterioration of the condition has been noted over the past two years. I began to experience chest pain, bitterness in my mouth, and belching.
In April 2022, the patient was consulted in the surgical department of the 6th City Clinical Hospital of Minsk. Additional examination was recommended for differential diagnosis. A comprehensive clinical, endoscopic and x-ray examination was carried out at the place of residence, as a result of which a clinical diagnosis was established: recurrent hiatal hernia. On May 29, the patient was hospitalized and operated on the next day. Reconstructive surgery was performed on the esophagus and stomach: laparotomy, hernia repair, anterior crurorrhaphy, Nissen refundoplication. The duration of the operation is 3 hours 40 minutes.
FROM THE OPERATIONAL REPORT: upper-median laparotomy with bypass of the umbilicus on the left. An audit of the abdominal organs revealed that there was a moderate adhesive process in the abdominal cavity after the previous operation. The greater omentum is soldered to the anterior abdominal wall, to the liver, and to the bed of the gallbladder. In the subhepatic space on the left, in the area of the esophageal opening of the diaphragm, there is a massive adhesive process.
Upon further inspection, it was determined that there was a recurrence of the hiatal hernia. The adhesions are separated, and the hernial orifice is isolated (diameter about 5 cm). Behind the esophagus, a mesh implant is palpated, which is fixed to the legs of the diaphragm. The area of the esophagogastric junction on the lower right is tightly fixed to the implant. An attempt to remove the mesh implant was accompanied by tissue trauma and moderate diffuse bleeding.
Two metal brackets removed. The mesh implant was left in its original place. The parietal peritoneum was dissected in the area of the hernial orifice along the left wall of the esophageal opening of the diaphragm. The stomach in the cardiac region was mobilized along the lesser curvature, two short gastrosplenic branches were crossed along the greater curvature. The abdominal part of the esophagus is isolated. The thoracic esophagus was mobilized down to 3 cm. The esophagus was displaced downward. There were no signs of the presence of a Nissen fundoplication cuff formed during the first operation. Self-destruction of the cuff occurred, apparently, due to the resorption of the suture material or cutting through the sutures.
Considering the above, an esophageal opening of the diaphragm up to 2.5 cm in diameter was formed by placing two sutures on the legs of the diaphragm in front of the esophagus. A Nissen fundoplication was performed with cuff formation using four sutures. The stomach, together with the esophagus, is fixed to the right leg of the diaphragm with one suture. On the left, the cuff is fixed to the diaphragm with one seam. Hemostasis control. Drainage tube into the subhepatic space to the plastic area, the second - above the spleen. Instruments were removed from the abdominal cavity. Layered suture of the wound with a mechanical skin suture. Bandage.
In the first days after surgery, severe dysphagia was observed. The patient could only take liquid food in small portions. On the 9th day after surgery, a control FEGDS was performed.
ENDOSCOPIC PICTURE : the esophagus is freely passable, the mucous membrane is pink, there are curdled mycotic deposits on it. The cardia closes. The cuff is formed in the area of the cardia and is passable without effort for endoscopes sequentially 5.2 mm and 8.0 mm in diameter. Empty contents with copious admixture of bile. The gastric mucosa is focally hyperemic, edematous, the relief is preserved. The pylorus, bulb and cavity of the duodenum are without features.
CONCLUSION : condition after hernioplasty with fundoplication according to Nissen. Erythematous gastropathy of the 1st degree. Mycosis of the esophagus.
Over the next four days, conservative therapy was continued. Two weeks after the operation, on June 13, the patient was discharged in satisfactory condition for outpatient treatment.
Conclusions 1. In modern conditions, the use of a minimally invasive endoscopic method of surgical treatment of hiatal hernia is a promising direction in esophageal surgery.
2. To prevent recurrence of the hernia, it is necessary to observe the basic principle of surgical treatment: not only to eliminate the hernia, narrow the hernial orifice, but also to restore normal interaction between the stomach and the esophagus.
3. In case of failure of crurorrhaphy sutures, cutting of sutures or dissection of the diaphragmatic leg, the task of reoperation is to restore the usefulness of the plastic and the size of the esophageal opening of the diaphragm.
4. The use of synthetic mesh endoprostheses for surgical correction of the hernia is considered a convenient immediate solution to the problem, but in case of recurrence of the hernia, this may interfere with the quality of the reconstructive operation. Mesh implants can only be considered as an option for the surgical treatment of giant hiatal hernias. Medical Bulletin , July 18, 2017
Author's technique of modified fundoplication using the Tope method at 270 degrees
We have improved the technique of laparoscopic surgery in the treatment of hiatal hernia, which allows us to reduce the number of relapses to 2% after one year and 4% after 5 years after surgery. We have received a RF patent for this technique.
A distinctive feature of my technique is gentle surgery, restoration of the anatomy of the upper floor of the abdominal cavity and the creation of a functional esophagogastric valve, which allows the patient to continue to lead a normal life, without taking medications. When isolating the esophagus and stomach, I use a modern device for dosed electrothermal tissue ligation “LigaSure” (USA), which makes it possible to “seal” the vessels without damaging the surrounding structures. The use of modern synthetic absorbable suture materials and anti-adhesion barriers also increases the effectiveness of the operations I perform. Using fundoplication according to the Tope method (France, 1984) at 270 degrees allows me to guarantee patients the physiological functioning of the sphincter in the postoperative period.
Using a fundoplication modified by me according to the Toupe method (France, 1984) at 270 degrees allows me to guarantee patients the physiological functioning of the sphincter in the postoperative period. In comparison with 360-degree Nissen fundoplication, where an absolute valve is formed, which does not exist in nature, the proposed technique is devoid of all disadvantages.
Which operation is better according to Toupet or Nissen?
Based on the volume of fundoplication, a distinction is made between partial, 270 degrees, according to Toupet and Douro, and complete fundoplication, 360 degrees, covering the entire esophagus, according to Nissen. Which cuff to form is one of the most controversial issues in hiatal hernia surgery, and at conventions such discussions are the most heated. Adherents of the Toupet fundoplication and Douroplasty are practically not performed, as they are found to be ineffective, but adherents of the Toupet fundoplication believe that there are fewer motor impairments and less frequent disturbances in the passage of food through the esophagus (dysphagia), their opponents claim. that a correctly performed complete fundoplication does not lead to problems any more often, but in the case of such a fundoplication there are less recurrences of a hiatal hernia. And most surgeons still prefer to perform a full, 360-degree fundoplication in various Nissen modifications. This technique, when performed correctly, has complications comparable to the Toupet technique, but relapse of the hiatal hernia is less likely to occur.
Professor Puchkov's experience in the treatment of hiatal hernia
My experience includes more than 2000 operations for hiatal hernia and reflux esophagitis, and is summarized in three monographs: “Hiatal hernia”, “Hand suture in endoscopic surgery” and “Technology of dosed ligating electrothermal effects at the stages of laparoscopic operations”, as well as more than in 50 scientific publications
in various professional peer-reviewed scientific publications in Russia and abroad.
You can watch videos of operations performed by me on the website “Video of operations of the best surgeons in the world.”
My seminars on laparoscopic treatment of hiatal hernia
and other diseases of the abdominal organs are visited by medical specialists from large scientific centers, republican, regional and regional hospitals, and students of postgraduate education faculties.
Method for assessing the barrier function of valves of hollow organs in abdominal surgery
It is worth noting that a hiatal hernia is often combined with cholelithiasis and duodenal ulcer, which also require surgical treatment. In this situation, endoscopic access seems ideal and allows simultaneous operations on different abdominal organs. With appropriate qualifications of the surgeon, the duration of the operation increases by only 30–40 minutes, and the number of complications remains low. In this case, cholecystectomy (chronic calculous cholecystitis) and selective proximal vagotomy (chronic duodenal ulcer) are simultaneously performed using laparoscopic access through the same punctures on the anterior abdominal wall.
After the operation, 3-4 incisions 5-10 mm long remain on the skin of the abdomen. From the first day, patients begin to get out of bed, drink, and the next day take liquid warm food. Discharge from the hospital is carried out on days 1–6, depending on the severity of the disease. The patient can begin work in 2 - 3 weeks. A strict diet should be followed for one and a half to two months, a softer one - for six months. Further, as a rule, the patient leads a normal lifestyle - without medications or diet.
In the “Doctors” program on the TVC channel, I spoke in detail and clearly about the latest methods of radical treatment for hiatal hernia and chronic heartburn.
Preparation for surgical treatment of hiatal hernia
Before surgery, an examination is carried out to determine the volume and type of operation. For this purpose, gastroscopy and radiography of the esophagus, stomach and duodenum with barium are performed. Sometimes a CT scan is performed if necessary. Patients are also advised by related specialists, a cardiologist, a therapist, and, if necessary, a pulmonologist.
Usually two weeks before surgery, proton pump blockers (omez, Nexium, etc.) are prescribed. This is done to relieve inflammation in the esophagus and facilitate surgical intervention.
Before the operation you should not drink or eat anything. In modern clinics, bowel preparation is not performed before surgery. Men need to shave the hair on their abdomen, from the xiphoid process to the groin; it is advisable to do this two or three days before surgery. In some clinics, the patient is admitted on the day of surgery.
Questions most often asked by patients with hiatal hernia
What anesthesia do you use for laparoscopic treatment of hiatal hernia?
If you would like to learn in more detail about the methods of pain relief used in the surgical treatment of a hiatal hernia, please read the information posted on the website carefully.
Is it necessary to somehow prepare for surgery for laparoscopic treatment of a hiatal hernia?
If you are planning surgical treatment of the hiatal hernia, I ask you to carefully study the preoperative preparation section.
Is it possible to perform surgery for the esophagus and uterine fibroids at the same time?
Minimally invasive surgery techniques allow two and sometimes three operations to be performed simultaneously during one anesthesia by a team of several surgeons. The issue of simultaneous operations is discussed in more detail in a special section of the site. Simultaneous performance of several surgical interventions will reduce the load on the body, reduce hospitalization time, and speed up the body’s recovery compared to performing several operations with an interval of 5-6 weeks.
Where can I undergo surgery with you regarding the hiatal hernia?
I conduct the initial consultation with all patients in Moscow at the Swiss University Clinic. Get acquainted in more detail with my main clinical sites in Moscow and Switzerland.
Symptoms and course
Often, a hernia does not manifest itself in any way and is defined as a “finding” when examining the stomach for other diseases. The classic version is represented by reflux esophagitis syndrome: spontaneous pain or when bending forward, pain in the lower third of the sternum or behind it, radiating upward or to the back, heartburn of varying intensity when the patient is lying down, which goes away if he sits or stands up, hiccups, belching of air. The most serious complications are strangulated hernia and bleeding from formed ulcers of the esophagus or stomach.
How I perform surgical treatment of hiatal hernia
For more than 15 years I have been performing surgical treatment using the method of Professor V.I. Onopriev and V.M. Durleshter. My teachers developed a method for open surgery, which I adapted for the laparoscopic approach. This technique is protected by two invention patents, and Vladimir Ivanovich received a state prize, including for the introduction of this operation.
We perform a full 360-degree fundoplication; the technique involves more thorough mobilization of the gastroesophageal junction, which almost always allows the stomach to be lowered into the abdominal cavity without any tension, forming a free, soft fundoplication cuff, which prevents the development of dysphagia (impaired swallowing). Careful mobilization avoids damage to the vagus nerves and prevents their inclusion in the cuff, which significantly improves functional outcome. After the lower third of the esophagus and the stomach are returned to the abdominal cavity, the legs of the diaphragm are sutured, after which the fundus of the stomach is fixed to its legs in 4 places, which allows the formation of a cuff without tension, and at the same time strengthens the legs of the esophageal opening, thereby reducing the number of relapses . On average, the operation lasts an hour, an hour and twenty
Method of surgical treatment Onoprieva V.I., Durleshtera V.M.