Pyloric stenosis - symptoms and treatment
The diagnosis is made on the basis of anamnesis, an objective examination of the child and laboratory and instrumental studies.
History taking
When talking with parents, it is possible to find out that in the first days after birth, the child experiences persistent regurgitation. As the disease progresses and the volume of the stomach increases, profuse “fountain” vomiting occurs. .
Inspection
During an objective examination of the child in the early stages of pyloric stenosis, a thickened pylorus is palpated (palpated). It is usually found under the rectus abdominis muscle on the right. You can note the peristalsis of the stomach in the epigastric region in the form of an “hourglass”. The above-described disturbances in the activity of the cardiovascular, digestive and nervous systems are characteristic [3].
Instrumental diagnostic methods
If pyloric stenosis is suspected, an ultrasound examination (ultrasound) . On ultrasound you can see a long pylorus with thickened walls. Diagnostic errors with this research method can be 5-10% [8][11][12].
X-ray examination reveals an increase in the size of the stomach and the presence of fasting fluid levels. Contrast testing shows that the evacuation of the contrast agent occurs with a delay, and narrowing and lengthening of the pyloric canal (beak sign) can also be observed [9].
One of the most informative methods for diagnosing pyloric stenosis is esophagogastroduodenoscopy (EGD). This is an examination method in which the doctor can examine the esophagus, stomach and duodenum using a microcamera. Endoscopy allows you to identify a narrowed pyloric opening, the convergence of the folds of the mucous membrane of the antrum (outlet) of the stomach towards the narrowed pylorus. If you insufflate (insufflate) with air, the pylorus will not open, and it will be impossible to pass the endoscope into the duodenum.
, electrogastrography (EGG) may be recommended - a non-invasive method for studying the motor function of the stomach. It is based on recording the biopotentials of the stomach from the surface of the body. A close connection between the electrical and contractile function of the gastrointestinal tract has been proven [20]. This method allows you to determine the tone, frequency and amplitude of stomach contractions.
Pylorotsenosis is a very serious disease, so examination of other organs and systems, ECG, urine and stool examinations, consultations with specialists, etc. may be required.
Laboratory diagnostic methods
To diagnose pyloric stenosis, an atropine test . Atropine is a drug that relieves spasms; in case of pylorospasm, relief or disappearance of symptoms is noted after its use. With pyloric stenosis, no changes occur, the pylorus remains closed. In many cases, antrum gastritis (gastritis of the outlet of the stomach at the border with the duodenum) and reflux esophagitis are detected.
A general blood test for pyloric stenosis often shows that hemoglobin is reduced, i.e. anemia has developed. Signs of inflammation of the gastric mucosa and ulcers may also be present: leukocytosis and accelerated erythrocyte sedimentation rate (ESR).
In case of pyloric stenosis, a hematocrit test is important - the percentage of blood cells (mostly red blood cells) in its total volume. Hematocrit decreases during the compensated stage of the disease, when vomiting still occurs very rarely.
An increase in hematocrit during pyloric stenosis is a formidable symptom of the severity of the disease. It means that the blood has clotted due to repeated vomiting and dehydration. Hematocrit is always elevated in the decompensated stage of the disease.
A biochemical blood test is especially relevant for subcompensated and decompensated stages of pyloric stenosis.
Patients note:
- hypoproteinemia (decreased protein levels);
- increase in aminotransferases (ALT, AST);
- increase in bilirubin (if liver function is impaired, usually during the decompensated stage of pyloric stenosis).
Also important for pyloric stenosis is the study of electrolytes, since when the body is dehydrated, the level of chlorine, sodium and potassium decreases.
Differential diagnosis with pylorospasm
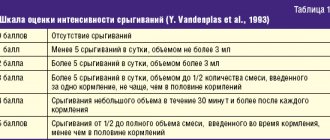
Pylorospasm, in contrast to pyloric stenosis, is successfully treated with therapeutic methods, because this is a functional condition (only the function of the organ is impaired, but not its structure) [5]. Due to similar symptoms (vomiting and regurgitation in the first weeks of life), the doctor always has to differentiate these pathological condition. The differences between the symptoms of pyloric stenosis and pylorospasm are presented in the table.
| Symptoms of the disease | Pyloric stenosis | Pylorospasm |
| Age of onset | Vomiting more often from the end of the second week of life | Vomiting from birth |
| Frequency of vomiting | Rare, mostly regurgitation | Frequent |
| Character of vomiting | Abundant, “fountain” | Not abundant |
| Frequency of vomiting | More permanent | Various |
| Amount of milk or formula vomited | More food eaten | Less food consumed |
| Chair | Constipation | Unstable |
| Number of urinations | Sharply reduced due to dehydration | Norm |
| Peristalsis of the stomach | Reinforced, hourglass shaped | Norm |
| Child behavior | Lethargy, occasional restlessness | Increased nervous excitability |
| Body mass | Pronounced deficiency | Maintained or moderately reduced |
As can be seen from the table, differential diagnosis of these two diseases, similar in clinical picture, can be carried out in the early stages. Considering the severity of the condition with pyloric stenosis and the likelihood of complications leading to death, it is necessary to promptly exclude this pathology in all infants with vomiting and regurgitation.
Do I need to feed my baby after spitting up?
- If the baby has eaten a long time ago, the milk/formula has almost been digested; if the body position changes, the baby may still burp. This is not a reason for additional feeding.
- If regurgitation occurs after feeding, this is a sign of overeating. It’s also not worth feeding.
- If the baby spits up profusely, this is a reason to discuss this issue with the pediatrician. We also don’t supplement feeding.
- If regurgitation is minimal, then you can feed as usual.
Taking into account the physiology of children, it is not possible to find a clear connection between feedings and regurgitation.
Actions to take when spitting up
Sometimes spitting up is easier to prevent than to treat. This does not always apply to cases where regurgitation is not physiological in nature and requires specialist supervision and possible surgical intervention.
So, simple tips to help minimize regurgitation:
- The first time the baby is put to the breast. Try to master this skill while still in the maternity hospital, turning to medical staff for help. You can also seek advice from a breastfeeding specialist. A baby who is properly attached to the breast will swallow less air during feeding, which will reduce the risk of regurgitation and stomach problems in the form of excessive gas formation.
- Get your baby used to lying on his tummy on a hard surface before feeding. This is a kind of massage that also has a beneficial effect on the baby’s stomach, reducing regurgitation and preventing colic and bloating.
- Before feeding, you can do a light massage of the abdomen in a clockwise direction, and light exercises.
- Try not to make your baby scream from hunger, as he will definitely swallow excess air, which will become a likely cause of regurgitation and just a bad mood. If this happens, try to calm the baby down first, and then start feeding.
- If feeding formula from a bottle, make sure it is full. The nipple of the bottle should be filled with milk, not air. Particular attention should be paid to the nipple, namely the hole in the nipple. It must be selected according to the age of the child. The inscription on the box of the bottle will help with this, indicating what age the nipple is designed for. The hole in the nipple regulates the flow of fluid and avoids choking during feeding.
- If during the feeding process the baby stops or begins to arch and cry, you can stop feeding and help the baby burp out excess air. To do this, take him in your arms, position him facing you so that the baby's arms and his head are on your shoulder. The baby will burp and perhaps return to eating again.
- Don't overfeed your baby. It is worth increasing the number of feedings, but reducing the portion. When bottle-feeding, the doctor will calculate the rate of food intake at a time and the total amount per day, based on the age and weight of the baby.
Many pediatricians, gastroenterologists, and surgeons take into account the recommendations of the working group of the European Society of Gastroenterology and Nutrition:
- position treatment
- use of therapeutic nutrition
- medication use
- surgery
- Treatment by position. During feeding, it is important to ensure that the baby is in a position in which the head and upper body are raised above the rest of the body. For this purpose, you can use a pillow or diaper. After feeding, hold the baby in a column to allow excess air to escape. Do not swaddle your baby tightly so as not to squeeze the stomach. After feeding, it is recommended to place the baby on his stomach or right side. But WHO recommends putting your baby to sleep only on his back.
- Medical nutrition. This means more frequent feedings with smaller portions. For children who are bottle-fed, the doctor may recommend the use of a therapeutic antirefluxor formula (AR is its designation on the package). These mixtures have an increased proportion of casein relative to whey proteins, so they are thicker, which prevents their release through the esophagus. Also, these types of foods are often enriched with thickeners, for example, starch or gum - a substance that, under the influence of the acid of the stomach contents, becomes thicker. This substance has the peculiarity of not being dissolved by enzymes, which allows it to remain thick in the stomach longer. It also promotes the active movement of food into the intestines from the stomach.
For more information about artificial feeding, read our article “Artificial feeding: feeding rules and types of formulas.”If the child is breastfed, then, on the recommendation of a doctor, the mixture can be added to the diet and enter the child’s body before milk. The duration of use of this mixture is about 3 months.
- Drug treatment. It is prescribed by a doctor, if the previously indicated methods have not brought results, then it is possible to treat with medications that can significantly improve the contraction of the intestinal walls.
- Surgical intervention. This is an extreme measure when the main cause of regurgitation is pathology.
Now more specifically about each:
Forms
There are 2 forms of pylorospasm:
- Compensated. The stomach begins to contract more strongly, and its “efforts” are enough to push food into the intestine. As a result, there is no stagnation of food, although severe pain and other symptoms of pathology are present.
- Uncompensated. The contractions of the stomach are not enough, and the food stagnates. The walls of the stomach cannot cope with the work and stop contracting altogether. If this condition persists for a long time, there is a risk of developing serious complications, and urgent surgical intervention may be required.
Based on the nature of development, there are 2 types of pathology:
- primary – pylorospasm occurs as an independent pathology, is often congenital, and is diagnosed at an early age;
- secondary – develops against the background of other gastroenterological diseases or lesions of the nervous system, more common in adults.
Treatment of the compensated form of pylorospasm is often successful, complete recovery and improvement of the functioning of the pylorus and stomach are possible.
Actions to prevent regurgitation
- hold in a column after feeding until burping;
- do not place on the stomach after eating;
- if the child is bottle-fed, then after consulting a doctor, you can choose an antirefluxor formula. It will prevent regurgitation due to its thickness;
- We do not play active games after feeding, we do not swaddle. Due to the physiological immaturity of the sphincter located between the stomach and esophagus. After food products pass through it, it may not close. Food can easily pass through the esophagus into the oral cavity. In children of the first year of life, this sphincter is poorly developed and may not work well.
Manifestations of pylorospasm
With pylorospasm, the following may occur:
- colicky pain in the stomach area,
- painful spasms in the pit of the stomach,
- weight loss occurs
- after the pain goes away, a “urinary crisis” occurs, the patient excretes a large amount of urine with low density and light color,
- may cause nausea and heaviness in the stomach, especially after eating,
- in severe cases, vomiting occurs, which brings relief,
- vomiting causes loss of salts, weakness,
- When food stagnates in the stomach for a long time, the vomit has a foul odor.
The last three symptoms may be a sign of the transition of pylorospasm to stenosis, which requires more active therapeutic measures.
Causes
The causes of congenital pylorospasm in children are often pathologies of the nervous system that are inherited, prolonged hypoxia, or difficult childbirth. In other words, there may be genetic factors in which pathology develops as the embryo develops. There may also be acquired factors in which a woman encounters difficulties during labor and childbirth, as a result of which the baby develops pyloric spasm.
Other causes of pathology in children and adults are conventionally divided into 2 groups: primary and secondary. The primary form of pathology occurs due to:
- disruptions in the functioning of the nervous system, which lead to the fact that relaxing stimuli do not reach the pylorus and its contractions are disrupted;
- deficiency of vital vitamins and other beneficial microelements, especially vitamin B;
- physical or mental fatigue, severe stress;
- intoxication with morphine, nicotine, and other strong toxic substances;
- disruptions in the functioning of the autonomic nervous system.
A common cause of intoxication of the body, which provokes pylorospasm, is work in hazardous chemical industries.
The secondary form of pathology develops as a consequence or complication of long-term diseases of the digestive system and other internal organs. These include:
- stomach ulcer, the focus of which is located in the pyloric region;
- chronic gastritis with high acidity;
- pyloroduodenitis (inflammatory process in the area between the outlet of the stomach and the beginning of the intestine);
- polyposis of the stomach;
- Crohn's disease and other chronic diseases associated with the inflammatory process in the lower parts of the digestive system;
- chronic diseases of the biliary tract;
- diseases associated with the inflammatory process in the pelvic organs (in women).
Predisposing factors to the development of pyloric spasm include smoking, other bad habits, and uncontrolled use of certain medications.