Quick transition Treatment of ulcerative colitis
Ulcerative colitis is a rare chronic disease characterized by inflammation of the inner layer of the colon, the mucous membrane. In this case, blood appears in the stool, and bowel movements themselves can become very frequent. In severe forms of the disease, anemia (decreased hemoglobin), weight loss may develop, and joints and skin may become inflamed. Fortunately, most cases of ulcerative colitis present with only intestinal symptoms.
Symptoms of Ulcerative Colitis
The main manifestation of ulcerative colitis is blood in the stool. Due to inflammation, the vessels in the intestinal mucosa dilate and blood cells leak out. Often a lot of mucus is released along with the blood.
Due to inflammation, the colon stops absorbing water, and stools become loose and frequent. Many patients experience false urges to have a bowel movement: they constantly want to go to the toilet.
Abdominal cramps and pain may occur before a bowel movement. With severe inflammation, body temperature may rise and joints may ache.
Ulcerative colitis affects only the large intestine: food is no longer absorbed there (unlike the small intestine), so severe weight loss, vitamin deficiencies or anemia occur infrequently.
Causes of the disease
With nonspecific ulcerative colitis, it is impossible to accurately determine the causes of its development, since this disease is characterized by an unclear etiology. However, based on many years of experience, experts were able to compile a list of the main factors in the development of ulcerative colitis:
- unfavorable environmental conditions (working or living in difficult environmental conditions);
- unbalanced diet - lack of vitamins and beneficial microelements leads to a weakened immune system in general;
- presence of bad habits (for example, smoking, alcohol abuse);
- taking medications for a long period of time;
- constant psychological stress.
Additionally, the following factors can cause the development of ulcerative colitis:
- a history of dysbacteriosis;
- hereditary predisposition;
- the occurrence of a viral or bacterial infection in the body;
- development of autoimmune processes, etc.
Taken together, these factors increase the risk of ulcerative colitis. It is worth noting that colitis is often diagnosed against the background of Crohn's disease.
Causes of Ulcerative Colitis
Like many other chronic diseases (asthma or hypertension), ulcerative colitis does not occur due to any one cause. The disease is more common in people whose relatives suffer from autoinflammatory or autoimmune diseases; in those who in childhood often received antibiotics, painkillers, or moved to distant countries. However, none of these factors alone causes ulcerative colitis. Rather, a combination of many events causes the immune system to attack the intestines.
There are many immune cells in the intestinal wall, and in the intestine itself there are many bacteria. The immune system is able to identify obviously harmful bacteria and reacts to them: it releases substances that cause inflammation and destroy bacteria (cytokines, reactive oxygen species). In ulcerative colitis, this process is disrupted: the immune system does not work correctly and mistakes “normal” bacteria for “enemies.”
With an intestinal infection, the protective inflammation of the intestines quickly ends, but with ulcerative colitis, immune cells maintain inflammation in the colon, attracting more and more cells. Therefore, ulcerative colitis rarely goes away on its own, without medication.
Page 8 of 10
Treatment of ulcerative colitis
The objectives of treating a patient with UC are:
- achieving and maintaining remission (clinical, endoscopic, histological),
- minimizing indications for surgical treatment,
- reducing the incidence of complications and side effects of drug therapy,
- reduction in hospitalization time and treatment costs,
- improving the patient's quality of life.
The results of treatment largely depend not only on the efforts and qualifications of the doctor, but also on the willpower of the patient, who clearly follows medical recommendations. The modern medications available in the doctor’s arsenal allow many patients to return to normal life.
The complex of treatment measures includes:
- dieting (diet therapy)
- taking medications (drug therapy)
- surgical intervention (surgical treatment)
- lifestyle change.
Diet therapy. Usually, during an exacerbation period, patients with UC are recommended to have a slag-free diet (with a sharp restriction of fiber), the purpose of which is to mechanically, thermally and chemically spare the inflamed intestinal mucosa. Fiber is limited by excluding fresh vegetables and fruits, legumes, mushrooms, tough, stringy meat, nuts, seeds, sesame, and poppy seeds from the diet. If tolerated well, juices without pulp, canned (preferably at home) vegetables and fruits without seeds, and ripe bananas are acceptable. Bakery products and pastries only made from refined flour are allowed. For diarrhea, dishes are served warm, pureed, and foods high in sugar are limited. Consumption of alcohol, spicy, salty foods, and dishes with added spices is extremely undesirable. In case of intolerance to whole milk and lactic acid products, they are also excluded from the patient’s diet.
In severe cases of the disease with loss of body weight, decreased protein levels in the blood, increase the daily amount of protein in the diet, recommending lean meat of animals and birds (beef, veal, chicken, turkey, rabbit), lean fish (pike perch, pike, pollock), buckwheat and oatmeal porridge, chicken egg white. In order to replenish protein losses, artificial nutrition is also prescribed: special nutrient solutions are administered through a vein (usually in a hospital setting) or through the mouth or tube, special nutritional mixtures in which the main food ingredients have been specially processed for their better digestibility (the body does not need to waste its forces to process these substances). Such solutions or mixtures can complement natural nutrition or completely replace it. Currently, special nutritional mixtures have already been created for patients with inflammatory bowel diseases, which also contain anti-inflammatory substances.
Failure to comply with the principles of therapeutic nutrition during an exacerbation can lead to aggravation of clinical symptoms (diarrhea, abdominal pain, the presence of pathological impurities in the stool) and even provoke the development of complications. In addition, it should be remembered that the reaction to various products varies from patient to patient. If you notice a deterioration in your health after eating any product, then after consultation with your doctor, it should also be eliminated from the diet (at least during the period of exacerbation).
Drug therapy is determined by:
- prevalence of colon damage;
- the severity of UC, the presence of complications of the disease;
- the effectiveness of the previous course of treatment;
- individual patient tolerance to medications.
Treatment for mild and moderate forms of the disease can be carried out on an outpatient basis. Patients with severe UC require hospitalization. The attending physician selects the necessary medications step by step.
In mild to moderate cases of the disease, treatment usually begins with the administration of 5-aminosalicylates (5-ASA) . These include sulfasalazine and mesalazine. Depending on the extent of the inflammatory process in UC, these medications are recommended in the form of suppositories, enemas, foams that are administered through the anus, tablets, or a combination of local and tablet forms. The drugs reduce inflammation in the colon during an exacerbation, are used to maintain remission, and are also a proven means of preventing the development of colon cancer if taken long-term. Side effects more often occur when taking sulfasalazine in the form of nausea, headache, increased diarrhea and abdominal pain, and impaired renal function.
If there is no improvement or the disease is more severe, then the patient with UC is prescribed hormonal drugs - systemic glucocorticoids (prednisolone, methylprednisolone, dexamethasone). These drugs cope with the inflammatory process in the intestines faster and more effectively. In severe cases of UC, glucocorticoids are administered intravenously. Due to serious side effects (swelling, increased blood pressure, osteoporosis, increased blood glucose levels, etc.), they must be taken according to a specific scheme (with a gradual reduction in the daily dose of the drug to a minimum or even complete withdrawal) under the strict guidance and supervision of the treating physician doctor Some patients experience phenomena of steroid refractoriness (lack of response to treatment with glucocorticoids) or steroid dependence (resumption of clinical symptoms of exacerbation of UC when trying to reduce the dose or shortly after discontinuation of hormones). It should be noted that during the period of remission, hormonal drugs are not a means of preventing new exacerbations of UC, so one of the goals should be to maintain remission without glucocorticoids.
With the development of steroid dependence or steroid refractoriness, severe or often relapsing course of the disease, the administration of immunosuppressants (cyclosporine, tacrolimus, methotrexate, azathioprine, 6-mercaptopurine) is indicated. Drugs in this group suppress the activity of the immune system, thereby blocking inflammation. Along with this, affecting the immune system, they reduce the human body’s resistance to various infections and have a toxic effect on the bone marrow.
Cyclosporine and tacrolimus are fast-acting drugs (the result is obvious after 1-2 weeks). Their timely use in 40-50% of patients with severe UC allows one to avoid surgical treatment (removal of the colon). The drugs are administered intravenously or prescribed in tablet form. However, their use is limited by high cost and significant side effects (convulsions, kidney and liver damage, increased blood pressure, gastrointestinal disorders, headache, etc.).
Methotrexate is a medicine for intramuscular or subcutaneous administration. Its action takes place after 8 – 10 weeks. When using methotrexate, you also have to take into account its high toxicity. The drug is prohibited for use in pregnant women, as it causes malformations and fetal death. The effectiveness of use in patients with UC is being clarified.
Azathioprine and 6-mercaptopurine are slow-acting drugs. The effect of taking them develops no earlier than after 2-3 months. The drugs can not only induce, but also maintain remission with long-term use. In addition, the appointment of azathioprine or 6-mercaptopurine allows you to gradually stop taking hormonal drugs. They have fewer side effects than other immunosuppressants and combine well with 5-ASA drugs and glucocorticoids. However, due to the fact that thiopurines have a toxic effect on the bone marrow in some patients, patients should be sure to periodically perform a complete blood count to monitor this side effect and initiate timely treatment measures.
At the end of the 20th century, a revolution in the treatment of patients with inflammatory bowel diseases (Crohn's disease, UC) was the use of fundamentally new drugs - biological (anti-cytokine) drugs. Biological drugs are proteins that selectively block the work of certain cytokines - key participants in the inflammatory process. This selective action contributes to a faster onset of positive effects and causes fewer side effects compared to other anti-inflammatory drugs. Currently, active work is underway all over the world to create and improve new and existing biological drugs (adalimumab, certolizumab, etc.), and large-scale clinical trials are being conducted.
In Russia, the only drug of this group is so far registered for the treatment of patients with inflammatory bowel diseases (UC and Crohn's disease) - infliximab (trade name Remicade) . Its mechanism of action is to block multiple effects of the central pro-inflammatory (inflammation-supporting) cytokine, tumor necrosis factor α. First, in 1998, the drug was licensed in the USA and Europe as a reserve drug for the treatment of refractory and fistulous forms of Crohn's disease. In October 2005, based on the accumulated experience of high clinical efficacy and safety of the use of infliximab in the treatment of patients with UC, a round table dedicated to the development of new standards for the treatment of UC and CD in the EU and the USA decided to include infliximab and UC in the list of indications for treatment. Since April 2006, infliximab (Remicade) has been recommended for the treatment of patients with severe ulcerative colitis in Russia.
Infliximab has become a real breakthrough in modern medicine and is considered the “gold standard” with which most new drugs (adalimumab, certolizumab, etc.) currently in clinical trials are currently compared.
For UC, infliximab (Remicade) is prescribed:
- patients for whom traditional therapy (hormones, immunosuppressants) is ineffective
- patients dependent on hormonal drugs (withdrawal of prednisolone is impossible without resumption of exacerbation of UC)
- patients with moderate and severe disease, which is accompanied by damage to other organs (extraintestinal manifestations of UC)
- patients who would otherwise require surgical treatment
- patients in whom successful treatment with infliximab caused remission (to maintain it).
Infliximab is administered as an intravenous infusion in a treatment room or at an anticytokine therapy center. Side effects are rare and include fever, joint or muscle pain, and nausea.
Infliximab is faster than prednisolone in relieving symptoms. Thus, some patients already feel better within the first 24 hours after administration of the drug. Abdominal pain, diarrhea, and bleeding from the anus are reduced. Physical activity is restored and appetite increases. For some patients, hormone withdrawal becomes possible for the first time, while for others, the colon can be saved by surgical removal. Due to the positive effect of infliximab on the course of severe forms of UC, the risk of complications and deaths is reduced.
This drug is indicated not only for achieving remission of UC, but can also be administered as intravenous infusion over a long period of time as maintenance therapy.
Infliximab (Remicade) is currently one of the most studied drugs with an optimal benefit/risk profile. Infliximab (Remicade) is even approved for use in children over 6 years of age.
However, biological drugs are not without side effects. By suppressing the activity of the immune system, just like other immunosuppressants, they can lead to an increase in infectious processes, in particular tuberculosis. Therefore, before prescribing infliximab, patients need to undergo chest x-ray and other studies for timely diagnosis of tuberculosis (for example, the quantiferon test is the “gold standard” for detecting latent tuberculosis abroad).
A patient receiving infliximab therapy, as with any new drug, should be closely monitored by his or her physician or anticytokine therapy specialist.
Before receiving the first infliximab (Remicade) infusion, patients undergo the following tests:
- chest x-ray
- Mantoux skin test
- blood analysis.
Chest X-ray and Mantoux skin test are done to rule out latent tuberculosis. A blood test is necessary to assess the patient's general condition and rule out liver disease. If an active, severe infection (eg, sepsis) is suspected, other tests may be needed.
Infliximab (Remicade) is administered directly into a vein, by drip, as an intravenous infusion, slowly. The procedure takes approximately 2 hours and requires constant supervision by medical personnel.
The standard recommended dose of a single dose of infliximab in patients with UC is 5 mg per 1 kg of body weight.
An example of calculating a single dose of infliximab required for one infusion. For a patient weighing 60 kg, a single dose of infliximab is: 5 mg x 60 kg = 300 mg (3 vials of Remicade 100 mg each).
Infliximab (Remicade), in addition to its therapeutic effectiveness, provides patients with a gentle treatment regimen. In the first 1.5 months at the initial, so-called induction stage of therapy, the drug is administered intravenously only 3 times with a gradually increasing interval between subsequent injections, carried out under the supervision of a physician. At the end of the induction period, the doctor evaluates the effectiveness of treatment in this patient and, if there is a positive effect, recommends continuing therapy with infliximab (Remicade), usually on a schedule of once every 2 months (or every 8 weeks). It is possible to adjust the dose and mode of administration of the drug depending on the individual course of the disease in a particular patient. Infliximab is recommended for use throughout the year, and, if necessary, for a longer period.
The future in the treatment of inflammatory bowel diseases (UC and Crohn's disease) appears very promising. The inclusion of infliximab (Remicade) in the government scheme for patients with UC and Crohn's disease means more patients can access the latest treatment.
If conservative (drug) therapy is ineffective, the need for surgical intervention is decided.
- Back
- Forward
Diagnosis of ulcerative colitis
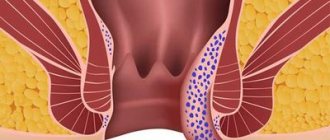
The main method for diagnosing ulcerative colitis is colonoscopy, an examination of the inner surface of the colon using an endoscope. A thin, flexible device is inserted into the intestine through the anus and the entire colon and the last centimeters of the small intestine are examined. Common signs of ulcerative colitis are erosions (small superficial ulcers), tenderness (the appearance of blood when pressure is applied to the wall) and the absence of visible vessels (they are located deeper in the wall and become invisible when the inner layer of the intestine is severely inflamed).
Ulcerative colitis is usually suspected when there is prolonged and causeless bleeding in the stool or prolonged diarrhea. Ulcerative colitis is a fairly rare disease (0.2% of the population), so even with obvious inflammation of the colon, doctors suspect other pathologies. For example, inflammation of the colon (colitis) can occur after taking antibiotics due to the growth of the bacterium Clostridiodes difficile. Temporarily, the intestine becomes inflamed due to salmonellosis, shigellosis, campylobacteriosis (therefore, the doctor will definitely ask if there have been any recent trips and if any of your loved ones have been “poisoned”). The intestines can also become inflamed from excessive use of painkillers, such as ibuprofen.
The diagnosis of ulcerative colitis is established if inflammation occurs for no apparent reason and recurs over and over again.
Who is at risk?
According to statistics, approximately 0.6% of the total population of the Russian Federation is diagnosed with IBD. It is also known that these values are increasing, that is, every year an increasing number of diseases are recorded.
Main features of the development of ulcerative colitis:
- Both men and women are equally susceptible to the disease (the disease is not gender specific);
- Every year approximately 30 thousand cases of Crohn's disease and ulcerative colitis are recorded;
- men aged 50 to 60 years are more susceptible to the disease than women at this age;
- The average age of people who develop ulcerative colitis ranges from 15 to 25 years;
- According to statistics, Europeans are more likely to suffer from ulcerative colitis than representatives of other races;
- Most often people living in highly developed countries and large cities get sick.
Research shows that ulcerative colitis is a disease that can be inherited from relatives. The risks of developing the disease are quite high and amount to 5.2–22.5%. At the same time, many questions remain about the disease and the characteristics of its spread.
Treatment of ulcerative colitis
In most cases, inflammation can be controlled with very safe drugs: mesalazine or sulfasalazine. They are taken orally in tablets or granules, and during an exacerbation they are also administered into the rectum in the form of suppositories or suspensions (enemas).
If the exacerbation is severe, glucocorticosteroids (for example, prednisolone) are temporarily prescribed. These are powerful anti-inflammatory drugs that quickly eliminate inflammation, but can cause unpleasant side effects. To avoid this, steroids are used in short courses and the dose is quickly tapered off once the symptoms of ulcerative colitis improve.
If it is not possible to stop frequent use of steroids, drugs that regulate the immune system are prescribed. Some of them suppress the division of immune cells (azathioprine and mercaptopurine). Others—infliximab, golimumab, adalimumab, and ustekinumab—block cytokines, substances that support inflammation in the intestines. A drug is also used that prevents immune cells from penetrating into the intestines from blood vessels (vedolizumab).
In severe forms of the disease (if medications do not help), the colon has to be removed. Fortunately, modern drugs in the vast majority of cases make it possible to avoid surgery.
Classification of the disease
There are classifications of UC depending on the location of the lesion, the nature of the course, the severity of the attack, the presence of complications, and the effectiveness of drug therapy.
To assess the extent of the lesion, the Montreal classification is used, which is based on the extent of visible changes during endoscopic examination of the colon:
Montreal classification of UC by extent of lesion
| Proctitis | The lesion is limited to the rectum |
| Left-sided colitis | The lesion extends to the left flexure of the colon (including proctosigmoiditis) |
| Total colitis | The lesion extends proximal to the left flexure of the colon (including subtotal colitis, as well as total UC with retrograde ileitis) |
According to the nature of the flow, they are distinguished:
- 1. Acute course (less than 6 months from the onset of the disease);
- 2. Chronic continuous course (absence of more than 6-month periods of remission against the background of adequate therapy);
- 3. Chronic relapsing course (presence of more than 6-month periods of remission).
Experts also use other classifications to assess the severity of ulcerative colitis according to clinical, laboratory and endoscopic criteria, to assess the risk of oncological complications and the need for frequency of observation.
Features and benefits of treatment for ulcerative colitis at the Rassvet Clinic
Doctors at the Rassvet Clinic use treatment protocols for ulcerative colitis developed by the world's leading associations (ACG, ECCO) and based on reliable scientific research. Our specialists do not use unproven methods for treating ulcerative colitis, such as a strict diet, and help create a treatment plan during pregnancy and breastfeeding. To protect against the side effects of immunosuppressants, the doctor will propose a vaccination plan and draw up a schedule of blood tests that will allow timely recognition of unwanted reactions to medications.
Author:
Golovenko Alexey Olegovich gastroenterologist
Etiology and pathogenesis
The development of the disease can begin under the complex influence of several factors (for example, genetic predisposition, intestinal microflora, immune disorders, negative environmental influences, etc.). It is worth noting that approximately hundreds of single nucleotide polymorphisms are associated with ulcerative colitis. Accordingly, this phenomenon increases the risks of the innate immune response, as well as the processes of recognition of microorganisms, functions of the epithelial barrier, etc.
Impaired recognition of bacterial molecular markers by dendritic cells is the main pathology of the immune system, which more often provides hyperactivation of pro-inflammatory signaling pathways. If a person with such a history additionally eats poorly, abuses alcohol and smokes, then he significantly increases the risk of developing ulcerative colitis.
Emotions and stress
Since the human body is a single system, the disease of some organs inevitably leads to the defective functioning of others. Thus, stress and emotional stress often negatively affect human health. However, there is no clear evidence that stress is an irritating factor for the recurrence of the disease.
It is important for people with ulcerative colitis to receive support and understanding from friends, family and doctors.
The chronic course of the disease can lead a person to depression, so the doctor always pays attention to the patient’s emotional state and, if necessary, prescribes antidepressants.
What questions should you ask your doctor?
To get the desired results from interacting with doctors, you need to find a common language with them. The patient’s interest in his own health is the best proof that he will follow all the specialist’s recommendations completely.
Ask your doctor the following questions:
- Could another disease in the body cause similar symptoms?
- What tests will be required to diagnose ulcerative colitis or another disease?
- What are the features of taking tests?
- What areas of the gastrointestinal mucosa are affected?
- Does current treatment need to change?
- What are the consequences if you stop taking the medication?
- What side effects may the prescribed medications have?
- How to behave if side effects occur while taking medications?
- What should be the behavior when symptoms of the disease appear?
- What symptoms should be considered extreme to promptly seek medical help?
- Do I need to change my usual diet? If so, what principles should be followed?
- Do I need to visit a doctor regularly to monitor the progress of the disease?
These and other questions with answers will help you adjust your behavior and lifestyle to make it more comfortable in combination with ulcerative colitis