Every year in Russia, up to 50,000 cases of stomach cancer are detected. Upon examination, 5–10% of patients are found to have a burdened family history: their close blood relatives once suffered from malignant tumors of the digestive tract. This allows doctors to suggest a diagnosis of hereditary stomach cancer. A genetic predisposition to cancer does exist. Neoplasms in this case have their own characteristics.
What is hereditary cancer
Stomach cancer can be caused not only by dysplasia of the mucous membrane, poor diet and bad habits. Sometimes the process of malignancy of cells in the body is triggered due to mutations of one or more genes. This feature is inherited, from older family members to younger ones, and the likelihood of developing the disease increases. If events develop unfavorably in one family, up to 40% of blood relatives may develop cancer. Hereditary forms of tumors account for 7% of the total number of oncological pathologies.
According to statistics, gastric tumors are diagnosed more often in men than in women. But with a hereditary form of the pathology, the likelihood of getting sick becomes the same in both sexes. Also, the hereditary disease has a fairly early manifestation - the average age of patients is only 38–40 years.
The capabilities of modern medicine make it possible to identify the presence of defective genes in a person and thereby determine the risk group. Such people need to pay special attention to preventive examinations.
How to collect honey. your family history?
The greatest benefit comes from information collected very carefully. It is necessary to collect information about all relatives: parents, grandparents, brothers and sisters. Families at increased risk of cancer are advised to do the following:
• Prepare information about at least three generations of relatives. • It is good to analyze the health data of representatives of the maternal and paternal line. This need is due to the fact that some gene syndromes are transmitted exclusively through the female line, and some - only through the male line. • Provide detailed information regarding ethnicity (on the lines of both parents), because certain pathologies are more characteristic of specific races and ethnic groups. • Write down information regarding medical care. problems of every relative. It is necessary to mention all the problems, because what seems unimportant can be the foundation for the development of cancer pathology.
For each member of your family line who has suffered from cancer, you must indicate the following information: • location of the cancer focus (if you have medical documents, it is recommended to attach a photocopy of the histological report); • at what age the cancer was diagnosed (this is extremely important for establishing a potentially dangerous age interval); • the influence of carcinogens (presence of bad habits, poor working conditions, poor environmental conditions in the place of permanent residence of a particular relative); these factors provoke the formation of cancer in a huge number of cases; • methods of diagnosis and subsequent treatment.
Reasons for development
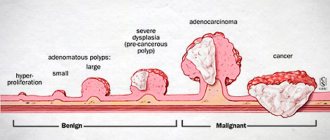
Absolutely all forms of tumors are the result of various DNA mutations, which result in the formation of “wrong” cells capable of uncontrolled reproduction. Sporadic forms are more common, when a person initially had healthy genes and, under the influence of internal and external factors, they mutated over time. The hereditary form suggests that the “broken” gene was passed on to the person from the parents.
Even if a genetic study has confirmed a predisposition to cancer, the risk of getting the disease will not be 100%. The likelihood of illness just increases. The extent to which this occurs depends, among other things, on the patient’s lifestyle, his age, and the presence of concomitant diseases. There are cases when a completely healthy person has 1–2 relatives suffering from cancer, but this is not the result of hereditary mutations, but an unfortunate combination of circumstances.
Hereditary gastric cancer is most often caused by mutations in the CDH1 gene. Normally, it acts as a suppressor - it suppresses random mutations and the development of pathological cells. If the gene “breaks,” favorable conditions are created for the process of malignancy (malignancy) of cells. CDH1 acts on a protein molecule that ensures the strength of intercellular connections. If the gene does not work correctly, interepithelial connections are disrupted, and uneven cell division occurs. This is how a tumor arises; over time, it grows into the submucosal and muscular layer of the gastric walls. More than 80 variants of CDH1 gene mutations are known. Each of them increases the risk of stomach cancer by 80%.
Predisposing factors include the habit of drinking alcoholic beverages and smoking, long-term consumption of fatty, fried foods with carcinogens. The occurrence of malignant formation is often preceded by various forms of gastritis and gastric polyps.
Deadline
We conduct a full study and formulate a conclusion within 35 working days.
The deadline may seem significant, but it is not. This is the fastest speed on the market for studies of this volume using NGS technology.
The specified time is required to perform a multi-stage high-tech study, which includes a large number of laboratory stages and intermediate quality control. The result is a large array of genetic data that requires separate analysis and interpretation using bioinformatics methods, which also takes time.
Symptoms
Cancer in its course is an insidious disease. In the initial stages, when the tumor has not yet penetrated the submucosa, specific symptoms are completely absent. Diagnosis of neoplasms at this stage is most often an accident.
As the disease progresses, the following symptoms occur:
- pain in the epigastric region;
- nausea;
- quick satiety with small amounts of food;
- stomach bleeding.
The pain syndrome has its own characteristics: it spreads to the entire epigastric region, is not localized to specific points, is not relieved by taking conventional painkillers, and is not associated with the time of day or meals.
When internal organs are affected by metastases, symptoms associated with these organs occur, for example, jaundice with liver metastases, hemoptysis with lung metastases.
At stage 4 of the disease, symptoms of general intoxication of the body appear, since the tumor poisons it with decay products. Headaches, weakness, anemia, increased fatigue, sweating, pain in bones and joints are observed.
Anatomy of the esophagus
The esophagus is a tube that connects the pharynx to the stomach. The place of transition of the pharynx into the esophagus in an adult corresponds to the level of the VI cervical vertebra or the lower edge of the cricoid cartilage; the place of transition to the stomach is projected at the level of the XI thoracic vertebra. The length of the esophagus in an adult reaches 25 cm. Lying in a small part in the neck area, the esophagus descends into the chest cavity through the apertura thoracis superior, and then, after passing through the latter, through the hiatus esophageus of the diaphragm it penetrates into the abdominal cavity, passing into the cardiac part of the stomach. In this regard, three sections are distinguished in the esophagus: the cervical part, the thoracic part and the abdominal part.
The cervical esophagus extends from the level of the VI cervical vertebra to the I-II thoracic vertebra. Its length ranges from 5 to 8 cm.
The thoracic region has the greatest length - 15-18 cm and ends at the level of the X-XI vertebrae, that is, at the point where the esophagus enters the diaphragmatic opening.
The abdominal section is the shortest, reaching a length of 1-3 cm. At the junction with the stomach, the esophagus expands slightly.
The lumen of the esophagus is not the same, and along its entire length it is customary to distinguish three narrowings and two expansions. The first narrowing is at the junction of the pharynx with the esophagus, the second is where the esophagus adjoins the aorta, and the third is at the point of passage through the hiatus esophageus. Between these narrowings there are two expansions.
The wall of the esophagus has three membranes: internal (mucosal), middle (muscular) and external (adventitial); the abdominal part is, in addition, covered with a serous membrane.
The mucous membrane is represented by multilayered squamous epithelium. The thickness of the purulent layer is formed by loose fiber and developed lamina muscularis mucosae, consisting of smooth fibers, the role of which is to reduce the mucous membrane when the lumen of the esophagus decreases.
On a cross section, the lumen of the esophagus has the appearance of a star-shaped fissure due to the compressed walls and well-defined longitudinal folds. The size of the latter is associated with the significant development of loose connective tissue, which forms the submucosa, lying between the mucous membrane and the muscular layer. The submucosa contains many vessels and mucous esophageal glands.
The muscular layer consists of two layers: internal (circular) and external (longitudinal). In the intermuscular layer, in its loose connective tissue, there are vascular networks and nerve plexuses. In the upper part of the esophagus, the muscle layers are represented by striated muscles, which in the middle third becomes smooth, and, finally, in the lower third consists exclusively of smooth muscles.
The adventitia of the esophagus is formed by loose connective tissue containing a small amount of elastic fibers. The main blood vessels, lymphatic vessels, and nerve trunks pass through the thickness of the adventitia. The blood supply to the esophagus in the cervical region is carried out by the inferior thyroid artery, in the thoracic region by the esophageal and bronchial vessels, in the abdominal region by the left gastric and phrenic left arteries.
Features of hereditary gastrointestinal tumors
There are two forms of hereditary stomach tumors:
- Diffuse
. It is represented by undifferentiated and signet ring cell cancer and poorly differentiated adenocarcinomas. The tumor does not have clear boundaries; it is characterized by infiltrating growth in the mucous membrane over a large area. The diffuse form is characterized by a high level of malignancy and a long asymptomatic period, which explains the low percentage of 5-year survival. Transmitted by CDH1 mutations.
- Intestinal
. Represented by differentiated adenocarcinomas. The formation has clear boundaries and is characterized by a relatively low level of malignancy. Often develops against the background of atrophic gastritis, and may accompany Lynch syndrome - non-polyposis cancer of the rectum and other parts of the large intestine.
Lynch syndrome is caused by mutations in the MLH1, MSH2, MSH6 genes. This cancer is transmitted in an autosomal dominant manner. Along the way, tumors of the ureter and small intestine are often detected in patients, and in women, tumors of the uterine body.
Family history also affects intestinal cancer. Patients are often diagnosed with FATK, familial adenomatosis of the colon. The hereditary disease is caused by a mutation in the APC gene.
Ovarian oncology
The hereditary type of this deviation is diagnosed in 10% of cases. This defect is combined with oncology of the breast or large intestine. Like breast cancer, this disease manifests itself in young women whose relatives also suffer from it. It is important to note the fact that hereditary ovarian cancer has been studied better than gene mutations in spontaneously forming tumors.
The following gene elements are responsible for the appearance of ovarian cancer pathology: BRCA1, BRCA2, PMS1, PMS2, MSH1, MSH6, MLH1. In order to control and timely detect the disease in question, it is recommended to systematically undergo a gynecological examination; Also, you need to periodically do ultrasound. Today, the most effective method of prevention is organ removal.
What other cancers are genetically transmitted?
There is a family predisposition to oncology of the female reproductive system: ovaries, uterus, mammary gland, as well as lung tumors. As with the digestive system, it is caused by genetic abnormalities. Most often this is a mutation of the BRCA1 and BRCA2 genes. They are responsible for suppressing the growth of malignant cells.
Hereditary neoplasms also include:
- retinoblastoma is an intraocular tumor, inherited in an autosomal dominant manner;
- nephroblastoma is a highly malignant kidney cancer, detected in children under 5 years of age;
- Li-Fraumeni syndrome is a tumor syndrome, manifested by tumors of the central nervous system, the development of sarcomas, and acute leukemia.
These neoplasms are often detected at a young age, before 30 years of age.
Sources
- Allgayer H., Redher H., Fulda S. Hereditary Tumors: From Genes to Clinical Consequences. Weinheim: Wiley-VCH, 2009.
- Ferguson L.R., Chen H., Collins AR, Connell M., Damia G., Dasgupta S., etal. Genomic instability in human cancer: Molecular insights and opportunities for therapeutic attack and prevention through diet and nutrition. Seminars in Cancer Biology. December, 2015. 35 Suppl: S5–S24.
- Genetic risk, race and ethnicity. Cancer Fighters Thrive Magazine. CancerCenter.com. Archived Last reviewed: 2018-02-21
- Genetics. National Cancer Institute. 2015-04-22. Last reviewed: 2018-02-20.
- Hodgson S. Mechanisms of inherited cancer susceptibility. Journal of Zhejiang University Science. 2022, B. 9 (1): 1–4.
- Roukos DH Genome-wide association studies: how predictable is a person's cancer risk?. Expert Review of Anticancer Therapy. April, 2009, 9 (4): 389–92.
- Stewart BW, Wild CP Cancer etiology. World Cancer Report 2014. World Health Organization. 2014, pp.16–54.
- Afanasyev A. Hereditary tumor syndromes: genetics and diagnosis. Publisher: Aurora, 2022.
How to identify a predisposition to cancer
If a patient is concerned about the possibility of passing on a mutated gene, genetic testing may be performed. This is a simple test that can detect mutations in the CDH1, MLH1, MSH2 genes.
Indications for analysis:
- more than 3 cases of stomach tumors in the family on the father’s or mother’s side;
- stomach cancer in a blood relative under 40 years of age;
- 2 cases of malignant neoplasms in close relatives under 50 years of age.
The material for the study is venous blood. You need to take the test on an empty stomach. Carriers of identified oncogenic mutations are recommended to register with a dispensary.
How can healthy relatives of a cancer patient be examined?
If there is a proven carriage of malignant heredity, such a question should not arise; the patient follows a certain diagnostic program all his life and is assigned to a state medical institution.
The vast majority of relatives of 95% of cancer patients should undergo regular screening for malignant processes, included in the standard medical examination program, which involves examination every 3 years.
For timely detection of malignant processes, women need to:
- every 2 years, perform a breast ultrasound or mammography ;
- in case of initial breast pathology, MRI of the mammary glands ;
- be examined annually by a gynecologist using colposcopy and taking a Pap test .
For men, the PSA level is important and the older they are, the more often it is determined, of course with a urological examination.
Regardless of gender, you should annually undergo:
- X-ray of the chest organs , often replaced in government institutions by harmful and useless fluorography, despite the fact that the ideal examination of the lungs is only CT , which is the one that can detect early cancer.
- Ultrasound of the abdominal cavity and pelvic organs using special sensors.
- Colonoscopy at intervals according to age and existing intestinal diseases.
- Gastroscopy with tests for Helicobacter can be done less often or more often, depending on the pathology present.
Analysis for tumor markers is not used for preventive diagnostics; it is used only to monitor the dynamics and effectiveness of cancer treatment.
Great importance is attached to diagnostic equipment; it must be not just modern, but highly accurate. It is not wise to undergo a CT or MRI scan every year in different institutions; the resolution of the equipment may differ significantly, making it impossible to see the pathology or compare the previous picture with the present one.
The benefits of regular examination are offset by poor quality of its implementation, therefore it is advisable to conduct a preventive examination in specialized oncological institutions, where thousands of such examinations are done, and doctors have not only been trained, but also have rich clinical and diagnostic experience.
Highly professional oncological examination is an integral characteristic of Euroonco; we successfully treat malignant processes and are able to see a tumor at an early stage of growth. We know what else needs to be added to a well-conducted examination in order to live long and not be afraid of cancer.
Book a consultation 24 hours a day
+7+7+78
Preventive measures
In order to promptly notice the slightest changes in the mucous membrane of the organ, it is recommended to perform preventive fibrogastroduodenoscopy (FGDS). The procedure is performed with local anesthesia; the doctor numbs the oropharynx with lidocaine.
A special instrument, a gastroscope, is inserted into the body through the oral cavity. With its help, the doctor examines the condition of the mucous membrane of the esophagus and stomach. Polyps, ulcerative lesions, and reflux disease may be detected.
The following symptoms are considered a clear indication for the procedure if you are predisposed to stomach cancer:
- intense pain in the epigastric region;
- stomach bleeding;
- swallowing disorders;
- long-term stomach upsets;
- weight loss for no obvious reason.
FGDS can be performed for preventive purposes once every 6–12 months. Is it possible to suspect oncology based on this study? If the doctor has reason to suspect a malignant tumor, during the procedure he will be able to perform a biopsy - taking a tissue sample. The material will be sent to the laboratory for histological examination. Based on its results, an accurate diagnosis will be established.
You can also get tested for Helicobacter pylori. This is a bacterium that infects the stomach and duodenum. Helicobacter does not cause cancer, but provokes various forms of dysplasia of the organ mucosa, which are, in fact, precancerous conditions. Analysis for Helicobacter is carried out using the PCR method, the research material is venous blood.