Gallbladder deformity
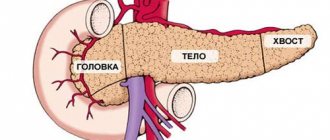
Gallbladder deformity is a common pathology that can be congenital or acquired throughout a person’s life. The gallbladder is a small, hollow organ for storing bile. It is an elongated sac, shaped like a pear when filled with bile. The gallbladder is divided into an upper narrowed part - the neck, from which the cystic duct arises, a middle part - the body, and a lower fundus. The most common deformities are kinks, twisting and constrictions of the gallbladder in the cervical area.
Main symptoms
If the deformation of the gallbladder does not affect the flow of bile into the duodenum, it may not manifest itself in any way and can only be detected by ultrasound. If the deformation interferes with the normal outflow of bile, the following symptoms are observed:
- heaviness in the stomach after eating;
- bitter taste in the mouth;
- nausea and vomiting after eating fatty foods;
- pain in the right hypochondrium, and laboratory tests indicate an increase in bilirubin levels.
Mechanism of disease development
Congenital deformation of the gallbladder occurs under the influence of various factors during intrauterine development; it usually does not manifest itself in any way and is detected only on an ultrasound examination.
Acquired deformity of the gallbladder has many causes, among them are:
- diseases of the gastrointestinal tract . For example, long-term cholecystitis, acute cholecystitis or cholelithiasis can lead to inflammation of the outer wall of the gallbladder - pericholecystitis and the formation of adhesions;
- sudden movements and heavy lifting can cause short-term incomplete twisting of the gallbladder around its axis. This deformity is asymptomatic and usually resolves without treatment;
- pronounced prolapse of internal organs in older people, stretching and sagging of the gallbladder when it enlarges and contains stones;
- eating disorders , fatty and heavy foods stimulate the secretion of large amounts of bile and lead to stretching and deformation of the gallbladder.
When to see a doctor
- if you are bothered by mild pain in the right hypochondrium, nausea, belching, heaviness in the stomach and a bitter taste in the mouth;
- for preventive examination in case of deformation detected on ultrasound;
- In case of severe pain, urgent medical attention is required.
Complications
The most dangerous is a rare deformity in which the gallbladder twists around its longitudinal axis several times. Such twisting leads to impaired blood circulation in the wall of the bladder, necrosis and perforation of the wall, bile enters the abdominal cavity and bile peritonitis develops. There is a sharp pain in the right half of the abdomen, vomiting, bloating, sweating and weakness. This condition is life-threatening, only urgent surgery can help, so you must immediately call an ambulance.
The use of ultrasound and computed tomography in the diagnosis of Klatskin tumor
Ultrasound scanner WS80
An ideal tool for prenatal research.
Unique image quality and a full range of diagnostic programs for an expert assessment of a woman’s health.
Introduction
Klatskin tumor - extrahepatic cholangiocarcinoma, cholangiocarcinoma of the proximal bile ducts. It accounts for about 10-20% of all neoplasms of the liver ducts, 70-80% of cases of bile duct cancer and about 15% of all malignant liver tumors. In the literature it is also found under the names “portal cholangiocarcinoma”, “hilus tumor”, “portal liver cancer” [2-5, 7, 8].
A primary malignant tumor of the bile ducts was first described by Durand-Fardel in 1840. The term “Klatskin tumor” appeared later when Gerald Klatskin in 1965 reported a tumor (cholangiocarcinoma) arising from the bifurcation of the common hepatic duct.
Bile duct cancer accounts for about 2% of all malignant tumors and is thus the fifth most common malignant tumor of the gastrointestinal tract [1-3, 5, 6, 9].
Cholangiocarcinomas are rare tumors. In recent years, there has been an increase in incidence: 3-4 new cases per 100,000 people. Most common in men over 50 years of age. Carcinomas grow rather slowly and do not manifest themselves clinically. Therefore, about half of all patients have regional lymph node metastases at the time of diagnosis, and thus treatment begins at advanced stages. Previously, central cholangiocarcinoma was considered an inoperable tumor; only palliative treatment was carried out. It is only over the past three decades that invasive surgical methods for tumor removal have replaced a purely palliative approach as a potentially radical treatment. However, even today cure is achieved in approximately 30% of all patients. Despite significant progress in the surgical treatment of hilar cholangiocarcinoma, the prognosis of the disease remains unsatisfactory [2, 4, 6-9].
Tumors of the bile duct bifurcation present certain difficulties for surgeons, which is primarily due to the complexity of the operation, as well as the severity of the condition of this category of patients. In such patients, any surgical intervention carries a high operational and anesthetic risk. Even after radical tumor resection, the 5-year survival rate is only 23 to 46%, and only 9 to 34% if the tumor was detected microscopically at the resection margin [1, 3, 5, 7-9].
For a better understanding of the location of the tumor, below is a diagram of the biliary tree (Fig. 1).
Rice. 1.
Diagram of the biliary tree.
This tumor develops in the upper parts of the bile ducts, in the area of their division between the right and left lobes of the liver. The bile ducts located inside the liver are divided into right and left ducts. A tumor can develop in one of them, or in both of these ducts, in the area where they leave the liver. According to the Bismuth-Corlette classification [9], a distinction is made between tumors that do not reach the bifurcation of the bile ducts (type I) and tumors that extend to the bifurcation (type II). Type III tumor grows through the bifurcation and spreads to the right (type III a) or left (type III b) bile duct. Type IV Klatskin tumor extends from the bifurcation into the left or right bile duct and is a multicentric tumor (Fig. 2). The bile ducts are located next to the blood vessels of the liver, so they are often involved in the process.
Rice. 2.
Classification of Klatskin tumor according to Bismuth-Corlette.
A distinction is made between tumors that do not reach the bifurcation of the bile ducts (type I) and tumors that extend to the bifurcation (type II). Type III tumor grows through the bifurcation and spreads to the right (type IIIa) or left (type IIIb) bile duct. Type IV Klatskin tumor extends from the bifurcation to the left or right bile duct and is a multicentric tumor.
The clinical picture has all the signs of obstructive jaundice.
Ultrasound examination (US) and computed tomography (CT).
With ultrasound, visualization of the tumor itself is extremely difficult. However, its indirect signs are revealed: the presence of biliary hypertension (high block).
The accuracy of CT is 85-88%, and the detection of obstruction is up to 98.1%. Ultrasound and CT with puncture biopsy increases diagnostic accuracy to 94-96%.
On native CT scans, cholangiocarcinoma appears as a hypodense space-occupying formation with isolated calcifications in it. The expansion of the intrahepatic bile ducts proximal to the tumor location is also determined. After a bolus injection of a contrast agent, a weak peripheral “enhancement” of the tumor and a lack of accumulation of contrast in its central part may occur, even in the late phase. According to other data, after contrasting in the early arterial phase, cholangiocarcinoma quickly and unevenly accumulates the contrast agent over the entire area. Cholangiocarcinoma is characterized by tumor delay of contrast in the delayed phase (hyperdensity), which complicates its differential diagnosis with hemangioma.
The optimal research method for Klatskin tumor can be considered magnetic resonance imaging, which allows not only to determine the precise location of the tumor, but also to visualize in detail the structure of the liver vessels.
With MRI, T2-weighted images are the most informative: on them the tumor gives a relatively high signal intensity, especially in its periphery; areas of low signal in the central part of the tumor appear to correspond to a scar zone. Due to the low vascularity of cholangiocarcinomas, dynamic contrast-enhanced MR imaging is not very effective. In the early, arterial phase of contrast, as with CT, there is an unpronounced peripheral enhancement of the tumor, which in the later, parenchymal phase is replaced by the appearance of a hypointense rim.
As an illustration, we present our own clinical observations.
Clinical observation 1
Patient S., 63 years old, was admitted to the hospital with complaints of yellowing of the skin. She considers herself sick since February 2013, when she began to notice epigastric pain. When jaundice appeared, she was hospitalized in our hospital, where a biochemical blood test revealed: bilirubin 233 µmol/l, direct bilirubin 140.8 µmol/l, indirect bilirubin 92.2 µmol/l, AST 181 U/l, ALT 101 , amylase 25 U/l.
Ultrasound of the abdominal organs: the liver is enlarged in size, the contours are smooth, the echogenicity is increased, the intrahepatic ducts are dilated, lobar up to 7 mm. Portal vein 12 mm. The gallbladder measures 110x38 mm, the wall has a double contour, is completely filled with thick bile, in the projection of the neck there is a fixed calculus up to 14 mm. CBD 6 mm. In the 6th segment of the liver, closely adjacent to the wall of the gallbladder, extending onto the contour of the liver, a liquid formation up to 4 cm in diameter with multiple septations is visualized. The pancreas is of normal size, smooth contours, heterogeneous structure, increased echogenicity, duct 1 mm. The spleen is of normal size and structurally unchanged. Splenic vein 7 mm. Conclusion: Ultrasound signs of biliary hypertension - a high block at the level of the porta hepatis. Gallbladder calculus (wedging of a calculus into the neck of the gallbladder). Ultrasound signs of acute cholecystitis. Paravesical abscess? (Fig. 3).
Rice. 3.
Sonographic picture of patient S.
a)
Double contoured gallbladder (red arrow) and paravesical fluid formation (blue arrow).
b)
An enlarged gallbladder filled with thick bile (red arrows), a fixed stone in the neck of the gallbladder (green arrow), dilated intrahepatic ducts (blue arrow).
c)
Interruption of duct visualization at the confluence of the lobar ducts of the liver (blue arrows), lobar ducts (red arrows).
d)
Paravesical formations are liquid in nature, with a large number of septa inside and thick liquid (blue arrows).
According to the MRI conclusion, a gross expansion of the ducts of the right and left lobes of the liver is determined with their break in the projection of the confluence (porta of the liver). The CBD looks normal, no filling defects were found, diameter is 6 mm. The gallbladder contains a large number of small round stones, the contents with a reduced percentage of fluid. The Wirsung duct is 3 mm, not deformed, the contours are even. Conclusion: tumor of the hepatic porta with a separate block (Fig. 4).
Rice. 4.
MRI for Klatskin tumor. CBD (red arrow), common pancreatic duct (blue arrow), intrahepatic ducts in the bifurcation area (green arrow) - break in the fusion projection.
For therapeutic and diagnostic purposes, a percutaneous transhepatic cholecystostomy was performed, a diagnostic puncture of the paravesical abscess and fistulography were performed.
Under local anesthesia with a 25% solution of novocaine 60.0 ml, a Pigteil 9 Fr drainage was installed into the gallbladder cavity and fixed to the skin with two sutures. About 130 ml of cloudy, dirty gray liquid was removed. The cavity was washed with an aqueous solution of chlorhexidine.
A puncture of the paravesical formation was performed from a separate access, and about 7 ml of turbid bile was obtained.
Fistulography. Water-soluble contrast was introduced through the drainage tube, and the gallbladder measuring 60x30 mm was contrasted. The remaining sections are not contrasted (Fig. 5).
Rice. 5.
Fistulography of patient S. Tumor of the porta hepatis. After percutaneous transhepatic cholecystostomy. Drainage in the gallbladder cavity.
Percutaneous transhepatic cholangiostomy. Puncture of the right segmental duct is impossible due to technical difficulties. Under local anesthesia with a 0.25% novocaine solution, a puncture of the segmental flow of the left lobe of the liver was performed. Cholangiography (Fig. 9) - the ducts of the left lobe are contrasted, the ducts of the right lobe are not contrasted (the block is at the level of the initial section of the left lobar duct). A 9 Fr direct drain is installed along the conductor. When contrast is administered, the ducts of the left lobe of the liver are contrasted. The drainage is fixed to the skin (Fig. 6).
Rice. 6.
Cholangiography of patient S. Tumor of the porta hepatis. Contrasting ducts of the left lobe of the liver (blue arrows).
Ultrasound after installation of cholangiostomy. In the dynamics of free fluid in the abdominal cavity and subdiaphragmatic space on the left. The degree of dilation of the ducts in the left lobe decreased.
Final diagnosis. Tumor of the porta hepatis T4NXMX with a separate block (Klatskin tumor). Mechanical jaundice. GSD acute calculous cholecystitis. Paravesical abscess. Subhepatic infiltrate.
It is impossible to perform a biopsy minimally invasively due to inaccessibility. It is impossible to perform laparotomy due to severe impairment of hemostasis. The patient was discharged for outpatient follow-up treatment.
Clinical observation 2
Patient M., 36 years old, was admitted with complaints of yellowing of the skin without pain and weight loss.
An ultrasound scan of the abdominal cavity revealed that the gallbladder was collapsed and did not contain bile. CBD 6 mm. The pancreas is diffusely heterogeneous, increased echogenicity, duct 1 mm. Signs of intrahepatic hypertension are determined, the right lobar is up to 17 mm, the left lobar is not visualized, the left segmental is up to 10 mm. In the projection of the porta hepatis, a hypoechoic formation 28x26 mm with uneven, indistinct contours is visualized. Enlarged groups inside the abdominal lymph nodes are visualized. Conclusion: Ultrasound picture of a high liver block: Klatskin tumor (Fig. 7).
Rice. 7.
Sonographic picture of patient M.
a)
Dilation of the intrahepatic ducts (arrow).
b)
Collapsed gallbladder (red arrow), paraportal lymph node (blue arrow).
c)
Hypoechoic formation 28 x 26 mm with uneven, indistinct contours at the porta hepatis (arrow).
d)
Enlargement of the right lobar and left segmental ducts (arrows).
When performing a CT scan of the abdominal cavity at the border of the right and left lobes of the liver, with an irregularly shaped (infiltrative type) formation spreading into the gates of the liver, a formation measuring 25x37x59 mm, unevenly of average intensity, accumulates contrast (CT tumor), at its level the left lobar duct is not visualized and the right one breaks off lobar duct (diameter of the right lobar up to 22 mm). The intrahepatic bile ducts of both lobes are grossly dilated. CBD is not dilated. Lymph nodes of the porta hepatis up to 16 mm. Collapsed gallbladder. The left branch of the portal vein is compressed by the tumor infiltrate. The spleen is of normal shape, not enlarged, the structure and density of the parenchyma is not changed. The pancreas is diffusely heterogeneous, the contours are smooth and clear (Fig. 8).
Rice. 8.
CT scan of the abdominal cavity of patient M.
a)
Native phase.
b)
Arterial phase.
c)
Arterial phase.
d)
Excretory phase.
Palliative intervention was performed under ultrasound control: two drainages were installed transhepatically in the right and left lobar ducts. The patient has been discharged.
conclusions
Thus, modern diagnostic capabilities using ultrasound, CT and MRI make it possible to clearly establish the localization of the tumor process in the bile ducts and determine the scope of the upcoming intervention.
Literature
- Boyko V.V., Maloshtan A.V. Clinical and anatomical rationale for radical operations for cancer of the extrahepatic bile ducts // Kharkov surgical school - 2008. - N 4(31). — P. 105-113.
- Buryakina S.A., Karmazanovsky G.G. Klatskin tumor: modern aspects of differential diagnosis // Annals of Surgical Hepatology. - 2012. - T. 17. - N 1. - P. 100-109.
- Kozlov A.V., Tarazov P.G., Granov D.A. Methods of interventional radiology in patients with liver and bile duct cancer complicated by obstructive jaundice // Annals of Surgical Hepatology. - 2004. - T. 9. - N 1. - P. 10-19.
- Nazyrov F.G., Ikramov A.I., Akrabov M.M. Diagnosis and tactics of surgical treatment of patients with tumors of the proximal parts of the extrahepatic bile ducts // Surgery. - 2010. - N 6. - P. 36-39.
- Sedov A.P., Parfenov I.P., Mishustin A.M. Klatskin tumor: problems of diagnosis and treatment // Annals of surgical hepatology. - 2006. - T. 11 - N 3. - P. 11-16.
- Ercolani G., Grazi GL, Ravaioli M. Results of surgical treatment for hilar cholangiocarcinoma: a singlecenter experience // HPB. - 2004. - Vol. 6, N 1. - P. 26.
- Harmeet M. Cholangiocarcinoma: modern advances in understanding a deadly old disease // M. Harmeet, J. Gregory // J. Hepatol. - 2006. - Vol. 45, N 6. - R. 856867.
- Kawasaki S., Imamura H., Kobayashi A. Results of surgical resection for patients with hilar bile duct cancer // Ann. Surg. - 2003. - Vol. 238, N 1. - P. 8492.
- Yalcin S. Diagnosis and management of cholangiocarcinomas: a comprehensive review // Hepatogastroenterology. - 2004. - Vol. 51, N 55. - P. 4350.
Ultrasound scanner WS80
An ideal tool for prenatal research.
Unique image quality and a full range of diagnostic programs for an expert assessment of a woman’s health.