The presented materials are based on the official recommendations of the Russian Gastroenterological Association and the European evidence-based consensus on the diagnosis and treatment of inflammatory bowel diseases, adapted for a wide audience.
Causes of nonspecific ulcerative colitis of the intestine
The etiology of nonspecific ulcerative colitis is currently not fully established. The disease develops as a result of a combination of several factors, including genetic predisposition, environmental factors, defects of innate and acquired immunity, intestinal infections and microbiocenosis disorders. Currently, more than 100 gene polymorphisms have been described that predispose to the development of ulcerative colitis and cause the development of immune defects. In the presence of a hereditary predisposition and the influence of trigger mechanisms, the intestinal barrier function changes, and an immune reaction is formed involving microflora. The triggers for this process can be smoking, vitamin D deficiency, insufficient consumption of vegetables, fruits, dietary fiber, excess consumption of animal protein, intestinal infections, including C.difficile infection. The interaction of all these factors leads to the formation of chronic inflammation in the colon of varying severity.
What is ulcerative colitis?
Nonspecific ulcerative colitis (UC) or ulcerative colitis is a chronic disease of the colon, which, together with Crohn's disease, is classified as “inflammatory bowel disease” (IBD).
The word “colitis” means inflammation of the large intestine, “ulcerative” - emphasizes its distinctive feature, the formation of ulcers. Compared to Crohn's disease, UC is diagnosed 3 times more often. According to statistics from American experts, per 100,000 people. on average there are 10-12 with this diagnosis. Women get sick somewhat more often than men. Most cases are diagnosed at the age of 15-25 years (20-25% of patients under 20) or 55-65 years. It is very rare in children under 10.
Manifestation of the disease
Symptoms of UC can be divided into typical, which are usually present at the onset of the disease, and extraintestinal.
The first include:
- diarrhea (increased frequency of bowel movements more than 3 times a day),
- the presence of blood in the stool, nighttime bowel movements (more often with pronounced activity of the process),
- tenesmus (false urge to defecate that does not end with bowel movement),
- weight loss,
- fever,
- anemia (a decrease in hemoglobin can be manifested by pale skin, rapid heartbeat, and weakness).
Extraintestinal manifestations include:
- diseases of skin joints, sclera of the iris,
- autoimmune liver damage,
- osteoporosis,
- psoriasis,
- formation of stones in the biliary system,
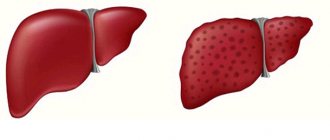
- fatty liver degeneration,
- thrombosis of peripheral veins.
However, extraintestinal manifestations are not strictly specific for UC, and their presence requires a careful assessment by specialists of the cause of occurrence.
Symptoms of ulcerative colitis can vary in severity. It depends on the stage of the disease, the nature of the disease (acute or chronic), severity and presence of complications. It should be remembered that, like any chronic disease, UC can occur with remissions and exacerbations, which also affects the clinical picture.
Causes and risk factors for developing ulcerative colitis
The causes of UC are unknown. Most researchers are inclined to think that this is an autoimmune problem. Risk factors identified:
- genetic. Ulcerative colitis often affects people who have blood relatives with the same diagnosis. To be precise, this pattern is observed in 1 out of 4 cases. Also, UC is particularly common among certain ethnic groups (for example, Jews), which also suggests the heritable nature of the disease;
- environmental factors. Most cases are registered among residents of the northern regions of Eastern Europe and America. The prevalence of ulcerative colitis is influenced by air pollution and diet. It has also been noted that in countries with a high level of hygiene, UC is more common;
- taking non-steroidal anti-inflammatory drugs.
Classification of ulcerative colitis (ICD codes)
According to the International Classification of Diseases, 10th revision, UC has code K51.
Depending on the location of inflammation, several subclasses are distinguished:
K51.0 - small and large intestine (enterocolitis)
K51.1 - ileum (ileocolitis)
K51.2 - rectum (proctitis)
K51.3 - rectus and sigmoid (rectosigmoiditis)
K51.4 - colon
Also included in this group of diseases is mucosal proctocolitis (K 51.5), a left-sided colitis that affects the rectum and sigmoid colon, and the descending part of the colon to the splenic angle.
Symptoms and signs of ulcerative colitis
Depends on the location, area of inflammation and severity of inflammation.
Main signs of UC:
- recurring diarrhea (diarrhea), often with blood, mucus or pus;
- stomach ache;
- frequent urge to have bowel movements.
Many patients complain of weakness, loss of appetite and weight.
UC is characterized by alternating exacerbations and periods with moderate symptoms or even asymptomatic ones. If it worsens, the following may be added:
- joint pain (arthritis);
- ulcers of the oral mucosa;
- soreness, redness and swelling of skin areas;
- eye inflammation.
In severe cases, the temperature rises, breathing becomes rapid and shallow, the heartbeat becomes fast or irregular, and blood in the stool becomes more noticeable.
In most patients, it is difficult to identify specific factors that provoke exacerbation. However, it is known that these can be infectious diseases and stress.
Diagnosis of UC
It is impossible to make a diagnosis based solely on symptoms. Only by excluding other probable and more common causes of the painful condition can the doctor confirm the presence of this particular disease. Usually carried out:
- colonoscopy, examination of the intestinal mucosa. If necessary, a small sample of tissue may be taken for examination (biopsy);
- general blood test - the presence of anemia (decreased number of red blood cells) and leukocytosis (increased number of white blood cells);
- stool analysis - the presence of red blood cells and white blood cells. It will also help to exclude other possible causes of poor health (presence of parasites, pathogenic bacteria);
- X-ray examination with contrast - prescribed for severe symptoms to exclude intestinal perforation (formation of a through hole in the intestinal wall);
- Computed tomography or magnetic resonance imaging are auxiliary diagnostic methods that are used to visualize the intestines.
Treatment of Crohn's disease and ulcerative colitis according to the rules
The basis is diet therapy, which is aimed at consolidating stool and reducing inflammation in the intestines. This means that you will have to exclude milk and dairy products, fresh fruits and vegetables, juices, and gluten-containing foods from your diet. In addition, you need to ensure that all products are fresh and follow basic hygiene rules. Doctors prescribe therapeutic enteral nutrition to such patients, which helps to heal the intestinal mucosa and also gain normal weight. As for medications, treatment is selected individually and includes hormone therapy, cytostatics and modern biological drugs.
Treatment of ulcerative colitis
Only surgical intervention can get rid of the problem forever. And even surgery does not guarantee a complete recovery.
The main goal of drug therapy is to mitigate the symptoms, transform the disease into an asymptomatic form and try to ensure that such remission lasts as long as possible.
The following groups of drugs are prescribed:
- anti-inflammatory drugs. As a rule, they form the basis of treatment. At the first stage - aminosalicylates in the form of tablets or rectal suppositories. In severe cases or if there is no effect, corticosteroids are added to the treatment regimen. They have a more pronounced anti-inflammatory effect, but also serious side effects. The purpose of taking them is to restrain the development of exacerbation for as long as possible. They are often prescribed to maintain remission.
- immunosuppressants (cyclosporines, infliximab, azathioprine) - drugs that suppress immune reactions. They are prescribed to relieve symptoms and put people into remission.
- antibiotics – to control infection;
- antidiarrheal drugs;
- painkillers (paracetamol). Patients with UC are contraindicated from taking ulcerogenic drugs: ibuprofen, diclofenac, naproxen and products containing them;
- Iron supplements – for the treatment of anemia.
Surgical treatment for ulcerative colitis
The main disadvantage of the operation is its traumatic nature. In most patients, a portion of the large intestine is removed, sometimes including the anus. To remove feces, an ileostomy is formed: a small hole is made in the abdominal wall, to which the edge of the small intestine is attached. The feces are collected in a small bag (colostomy bag) that is attached to the ileostomy.
This solution may be permanent or temporary. In the second case, a reservoir is formed in parallel from the small intestine, which is attached to the anus. While this artificial “bag” heals, bowel movements occur through a temporary ileostomy. During the next operation it will be stitched up. It becomes possible to remove feces naturally. But the frequency of bowel movements is much higher than normal (up to 8-9 times a day).
Modern aspects of the treatment of nonspecific ulcerative colitis in children
Why is nonspecific ulcerative colitis a medical and social problem? What are the principles of treatment?
In the tenth edition of the International Classification of Diseases, this disease is designated as ulcerative colitis (nonspecific), code K51 - “necrotizing inflammation of the mucous membrane of the colon and rectum, characterized by exacerbations.”
Peak age of onset is in the second and third decades of life, but the disease occurs in both infants and the elderly [4]. Nonspecific ulcerative colitis (UC), characterized by a progressive course and causing a number of complications, is therefore a big social problem, as it disrupts the child’s lifestyle and leads to early disability. All this indicates the severity of the disease.
Despite the commonality of many therapeutic approaches, the peculiarities of the physiological development of the child and differences in the clinical course of UC in children and adults, as well as insufficient experience in the use of modern drugs in pediatric practice, determine the difference in approaches to the treatment of children and adults.
Conservative treatment of UC in children is based on the following principles:
- diet therapy;
- basic therapy with 5-aminosalicylic acid and/or glucocorticoids (systemic and local action);
- antibacterial agents;
- cytostatics (immunosuppressants);
- immunomodulators;
- symptomatic (“accompanying”) therapy.
Treatment of UC in children should be comprehensive, always with careful adherence to the daily regimen and nutrition. An important condition for treating children in a hospital is to create for them an atmosphere of physical and mental peace. If your condition and well-being are satisfactory, only restriction of outdoor games is indicated. Quiet walks in the fresh air are necessary. If there is a significant disturbance in the general condition, fever, exhaustion, metabolic changes, etc., bed rest should be done.
Nutrition
For UC, a mechanically and chemically gentle diet with a high content of protein and vitamins is prescribed, milk is excluded, and the amount of fiber is limited. Sometimes even the slightest violation of the diet in children can lead to a worsening of the condition. Strict adherence to the diet is especially important in the presence of secondary malabsorption syndrome.
In the acute stage, fruits and vegetables are excluded. Pomegranate juice is allowed, and pomegranate peels are dried and used in decoctions as an astringent. Decoctions and jelly from dry blueberries, bird cherry, chokeberry juice, and black currant are widely used.
In addition, the so-called “astronaut food” is recommended, consisting of highly refined products that require almost no additional enzymatic breakdown. For this purpose, an elemental diet is used (isocal, cosylate, enshur, nutrichim, renutril, etc.). These drugs are also used for enteral tube feeding. This diet is especially indicated for patients with intestinal fistulas or obstructions, as well as for children who are stunted [4].
Most children with UC have severe protein deficiency due to protein loss, malabsorption, anorexia and vitamin deficiency, which leads to body weight deficiency. Therefore, in any form and phase of the disease, food should be as high in calories as possible, mainly from protein.
It is very important to exclude additional sensitization of patients with food allergens, therefore a hypoallergenic (elimination) diet is recommended: extractive substances, eggs, chocolate, cocoa, coffee, citrus fruits, strawberries, wild strawberries, red apples, baked goods, industrial canned products are prohibited, individual intolerance should also be taken into account food products.
Because cross-allergy is possible (children with a cow's milk allergy may have an allergic reaction to beef), it is often recommended to exclude beef from the diet [3].
The diet for UC is less strict only if remission is achieved.
Parenteral nutrition is prescribed for children with severe UC. For this purpose, infusion solutions such as alvesin, aminosol, aminopeptide, vamine, casein hydrolyzate, combined with glucose and polyionic solutions are used.
Preparations of 5-aminosalicylic acid (5-ASA)
The basis of basic therapy for UC is 5-aminosalicylic acid (5-ASA) preparations, or salicylates.
For many years, sulfasalazine, the active component of which is 5-ASA, has remained the preferred drug for the treatment of ulcerative colitis.
5-ASA inhibits the activity of neutrophil lipoxygenase and the synthesis of arachidonic acid metabolites (prostaglandins and leukotrienes), which become mediators of inflammation. It inhibits the migration, degranulation and phagocytosis of neutrophils, as well as the secretion of immunoglobulins by lymphocytes, inhibits the production of free oxygen radicals and is their inactivator [1, 4, 11]. 5-ASA also acts on the surface receptors of epithelial cells, electrolyte transport and permeability of the intestinal epithelium. In addition, 5-ASA affects adhesion molecules, chemotactic peptides and inflammatory mediators (eikanoids), platelet-activating factor, and cytokines [4, 11].
In addition to 5-ASA, sulfasalazine contains sulfapyridine, an inert substance that ensures the delivery of 5-ASA to the colon, which is the direct cause of frequently occurring side effects. Treatment with sulfasalazine in 10-30% of cases is accompanied by the development of side effects: gastrointestinal manifestations (anorexia, nausea, vomiting, pain in the epigastric region); general symptoms (headache, fever, weakness, arthralgia); hematological disorders (agranulocytosis, pancytopenia, anemia, hemorrhagic syndrome); signs of damage to the reproductive sphere, etc. [1, 6, 8].
Sulfasalazine blocks the conjugation of folic acid in the brush border of the jejunum, inhibits the transport of this vitamin, and inhibits the activity of the enzymatic systems associated with it in the liver, therefore, it is necessary to include folic acid in an age-specific dosage in the complex of therapeutic measures carried out in patients with ulcerative colitis receiving treatment with sulfasalazine.
Sulfasalazine is prescribed 3 times a day after meals: children under 5 years old - 1-3 g per day, from 6 to 10 years old - 2-4 g, over 10 years old - up to 5 g, depending on the severity of the disease. When the condition stabilizes, the dose is gradually reduced - initially by 1/3, after 2 weeks in the absence of deterioration - by another 1/3. The minimum dose at which the patient’s condition stabilizes is determined; if deterioration occurs, return to the previous dose.
The incidence of complications with sulfasalazine has led to the development of new drugs that do not contain sulfapyridine, such as mesalazine. To ensure that drugs enter the colon unchanged, they are covered with special coatings. There are three types of such drugs. The first are 5-ASA coated with acrylic gum (klaverzal, salofalk, asakol, rovaza), so such drugs are broken down only at pH = 6-7, which is characteristic of the large intestine. The drug Pentasa (5-ASA, encapsulated in ethylcellulose) begins to act already at pH>4.5 in the small intestine. Pentasa is prescribed at a rate of 20-30 mg/kg per day.
The second type of drugs is azo compounds of two 5-ASA molecules, which are broken down in the colon by the bacterial enzyme azoreductase (olsalazine). The third type is the non-absorbable polymer 5-ASA (balsalazide).
A number of 5-ASA preparations are available not only in the form of tablets, but also in the form of enemas and suppositories, for example, ready-made Pentasa and Salofalk suppositories, foam for microenemas, which are used rectally for distal lesions of the colon. Suppositories with sulfasalazine (sulfasalazine and cocoa butter) and microenemas with sulfasalazine (sulfasalazine tablets and distilled water), etc. are also prepared.
Salofalk tablets contain 250 mg or 500 mg of mesalazine and are prescribed in a dose of 500-1500 mg/day (30-50 mg/kg). In addition, the drug is used in the form of suppositories (250 mg, 500 mg) 1-2 times a day, in the form of enemas (2 g/30 ml and 4 g/60 ml) 1-2 times a day.
Mesacol (tablet contains 400 mg of 5-ASA) is prescribed in a dose of 400-1200 mg/day, depending on the child’s body weight and the severity of UC.
When using 5-ASA drugs, in some cases a dose-dependent effect is observed, which forces the drug dose to be increased to achieve remission. Maintenance therapy (half the prescribed therapeutic dose) is carried out over a long period of time, which allows for stable remission and reduces the risk of colon malignancy [9]. When carrying out maintenance therapy from 6 months to a year, every 2 weeks the dose is reduced to 1/4 tablet and increased to 1/2-1/4 tablet (general blood and urine analysis - once every 2 weeks).
With long-term use of sulfasalazine (maintenance therapy), the side effects of the drug are taken into account, primarily hepatotoxicity [6, 11].
In spring and autumn, anti-relapse courses are carried out with 5-ASA drugs (0.25-0.5-1 g once a day, depending on age).
Hormone therapy
Glucocorticoids (GC) occupy a leading place in the treatment of severe forms of UC. This is due, firstly, to the fact that 5-ASA drugs are not always effective in treating this disease. Secondly, the use of GCs gives a relatively quick positive effect, which is associated with their anti-inflammatory and immunosuppressive properties.
Indications for hormone therapy: acute course of the disease; severe forms; moderate forms (if a 2-week course of treatment with aminosalicylates was ineffective); chronic forms that are difficult to treat with other methods; systemic (extraintestinal) manifestations (polyarthritis, uveitis, hepatitis, high fever); intolerance to aminosalicylates [1, 7, 15].
For UC, GCs are used: locally (rectal administration); systemically - low doses, high doses, alternating therapy, pulse therapy, combination therapy (with 5-ASA, cytostatics).
Typically, the dose of GC (prednisolone, methylprednisolone) varies from 1 to 2 mg/kg. First, the daily dose of the drug is divided into three doses, then switched to a single dose in the morning.
If prednisolone is well tolerated, therapy at the prescribed dose is recommended until the desired result is achieved (within 3-4 weeks), after which the dose is reduced according to a stepwise scheme - by 10 mg every 5-7 days. Starting from 1/2 the initial dose, a single dose of prednisolone in the morning is recommended, which practically does not cause serious complications. The dose of prednisolone is reduced to 1/3 of the initial dose gradually, 5 mg every 7-10 days for 2-2.5 months. The full course of hormonal therapy takes from 10 to 20 weeks, depending on the form of UC.
If a long course is required, it is possible to switch to an alternating regimen of GC therapy, which consists of prescribing short-acting GCs without pronounced mineralocorticoid activity once, in the morning (about 8 hours) every 48 hours (every other day). The goal of alternating (decade) therapy is to reduce the severity of side effects of GCs while maintaining therapeutic efficacy [5].
In severe forms of UC, “hormone dependence” is observed, when hormone withdrawal leads to an exacerbation of the disease. In such cases, an alternating regimen of GC therapy is prescribed for a long time, for 3-6-8 months.
Sometimes, in severe forms of UC, pulse therapy is used, which involves intravenous administration of large doses of GC once a day for three days (methylprednisolone is often the drug of choice).
In addition to prednisolone, metypred is used, which is devoid of unwanted mineralocorticoid activity. The dose ratio of prednisolone-metipred is 5:4.
When the dose of prednisolone is reduced by half, sulfasalazine or 5-ASA is prescribed in a minimum dose (1/3 of the therapeutic dose). Next, the dose of 5-ASA is increased and, with complete withdrawal of hormones, it is brought to the maximum (therapeutic dose), selected depending on age (1-2 g per day). When remission is achieved, the dose of 5-ASA can be reduced to maintenance (1/2 therapeutic dose).
For distal lesions of the colon, prednisolone is prescribed in the form of microenemas and suppositories (microenemas are made from prednisolone tablets and distilled water, suppositories are made from prednisolone tablets and cocoa butter). “Drip” microenemas with hydrocortisone (hydrocortisone and distilled water) are successfully used, the doses of which depend on the child’s body weight and the severity of the disease.
The use of corticosteroids is associated with the development of a number of complications (immunosuppression, osteoporosis, hyperglycemia, Cushing's syndrome, growth retardation, peptic ulcers, hypertension, etc.). In addition, refractory forms of inflammatory bowel diseases are becoming increasingly common, treatment of which with glucocorticoids does not give the expected effect.
In recent years, “local” hormones (enterocort, budenofalk, budesonide) have been developed and are widely used in clinical practice (especially in hormone-resistant forms). They are distinguished by high affinity for hormonal receptors and first-pass metabolism. As a result, side effects are minimized [4, 15].
Budesonide is a local, potent, non-halogen glucocorticoid with anti-inflammatory, anti-allergic, anti-exudative and decongestant properties. The advantage of the drug is that it has a local effect and, due to poor absorption and rapid metabolization, does not have systemic effects. High affinity for hormonal receptors in the mucous membrane of the colon enhances the local therapeutic effect of budesonide (budenofalk). Due to its chemical composition, budesonide is highly lipophilic, it is able to perfectly penetrate cell membranes and distribute into tissues, quickly undergoing hepatic and extrahepatic metabolism. A gradual dose reduction is not required, since withdrawal syndrome does not occur [4, 15].
Antibacterial agents
Antibiotics for UC are used only when indicated: after surgical treatment, in febrile patients with septic complications, with toxic dilatation of the colon [13]. Trichopolum (metronidazole) is often used in long courses at a dose of 10-20 mg/kg per day. Antibiotics, if necessary, are prescribed cephalosporins.
Immunosuppressants
Immunosuppressants (cytostatics) are prescribed to children very rarely due to the large number of side effects [2]. The question of their use arises only in the case of ineffectiveness of corticosteroids and with a continuous course of the disease. In case of UC, especially when it comes to hormone-resistant forms, immunosuppressants are prescribed 6-mercaptopurine, azathioprine, methotrexate, cyclosporine, etc. [12, 14].
Azathioprine is close in its chemical structure and biological action to mercaptopurine, has cytostatic activity and has an immunosuppressive effect. However, compared to mercaptopurine, the immunosuppressive effect of the drug is relatively stronger with slightly less cytostatic activity.
Azathioprine is prescribed at a dose of 100 mg per day for 9-12 months, beginning to act by the 3rd month.
Methotrexate is a metabolite and antagonist of folic acid. It interferes with the synthesis of purine nucleotides, disrupts the synthesis of DNA and RNA, inhibits cell division and growth, causing their death. For UC, the drug is used intramuscularly at a dose of 25 mg once a week for 12 weeks.
Cyclosporine has a selective effect on T-lymphocytes, inhibits the reactions of cellular and humoral immunity and is currently considered as a reserve method when other treatments are ineffective.
Immunomodulators
The mechanism of action of immunomodulatory drugs in UC is associated with the suppression of the activity of natural killer cells and the function of cytotoxic T-lymphocytes.
It has been proven that the use of immunomodulators thymalin and tactivin in the complex treatment of patients with UC helps to correct the state of immunological imbalance, in particular eliminates the deficiency of the T-link of immunity, normalizes helper-suppressor ratios and the index of immune regulation, which leads to the elimination of the inflammatory process, as it relieves autosensitization and increases the body's defenses.
It is known that inflammatory bowel diseases are characterized by excessive production of anti-inflammatory cytokines. Recently, reports have begun to appear on the use of biotechnological drugs that can suppress inflammation [10, 16]. Particular attention is paid to two molecules: interleukin-1 and tumor necrosis factor (TNF-a), since at the present stage they are the main targets of anti-inflammatory therapy for various diseases. In 2001, a new generation drug infliximab (Remicade), which is a monoclonal antibody to tumor necrosis factor, was registered in our country. Remicade has increased anti-inflammatory activity.
Symptomatic (“accompanying”) therapy
As additional therapy aimed at normalizing digestive processes and increasing the body's immunoreactivity, angioprotectors, enterosorbents, intestinal antiseptics, antidiarrheal drugs, enzymes, biological products, vitamins, minerals, sedatives, and herbs are prescribed.
Of the angioprotectors, parmidine (0.125-0.25 mg 3 times a day) and trental (0.05-0.15 mg 3 times a day) are used to improve microcirculation.
Often there is a need to prescribe enterosorbents (polyphepane, carbolene), the most promising of which are considered to be enterosgel, algisorb, SUMS, vaulin.
Intestinal antiseptics from the quinoline series (intestopan, intetrix, enterosediv) and nitrofuran series (furazolidone, ercefuril), etc. are successfully used in children.
For persistent diarrhea, coatings and astringents (almalox) are prescribed, which, however, should be used very carefully. For the same purpose, atropine-containing antidiarrheal drugs (reasec-lomotil, which contains codeine and atropine; the drug has not only antidiarrheal but also antispasmodic effects), lispafen (atropine sulfate and diphenoxin hydrochloride) are sometimes prescribed. In recent years, imodium has become more popular (it has an opioid effect). Long-term use of this drug for ulcerative colitis is fraught with toxic dilatation of the colon.
Sandostatin should be recognized as a new and promising drug, which affects the absorption of water and electrolytes in the small intestine, reduces the concentration of vasoactive peptides in the blood, reduces the frequency of bowel movements and fecal weight.
Among enzyme preparations for UC, Mezim Forte, Creon, Lycrease, and Pancreatin are used.
Today, the most promising is the use of the drug Creon 10,000. It meets all the requirements for modern enzyme preparations: Creon 10,000 is characterized by an optimal qualitative composition of enzymes in physiological proportions, is resistant to acid, the size of the mini-microspheres of the drug ensures its uniform mixing with food and simultaneous chyme passage through the pylorus. Upon entering the stomach, the capsule containing minimicrofers dissolves within 1-2 minutes. More than 90% of enzyme activity is achieved after 45 minutes at a pH of more than 5.5. Creon 10000 is a safe drug and can be used in all groups of patients, regardless of gender and age.
Since in UC the colon mucosa provides favorable conditions for the development of dysbiosis, there is often a need to prescribe biological products. When the normal flora decreases, bifidumbacterin, lactobacterin, and bificol are prescribed. Metronidazole affects the anaerobic flora (clostridia, bacteroides), while drugs of the nitrofuran series are effective for Proteus dysbiosis.
You can prescribe enemas with preparations of sodium salts of propionic and butyric acids, as well as pantothenic acid (a coenzyme precursor) to regulate the metabolism of colon epithelial cells and ensure the normalization of colonocyte metabolism.
All patients should receive a complex of vitamins - potassium, calcium, a complex of microelements, and for iron deficiency anemia - iron supplements.
For UC, bromine, valerian root, rudotel, glycine, novopassit, etc. have a calming effect on the central nervous system.
Herbal medicine (chamomile, St. John's wort, burnet, kolgan, etc.) is one of the components of the complex treatment of UC in children.
For UC, astringents are also used: common oak (bark), St. John's wort (herb), gray alder (cones), bird cherry, common blueberry (fruits), common quince (fruits, seeds), common pomegranate (skin), burnet (burnet). roots); hemostatic: kolgan, burnet, pepper knotweed (herb), stinging nettle (leaves), alder, horsetail (herb), etc.
Above is a treatment plan for UC depending on the severity of the disease.
The problem of surgical treatment of ulcerative colitis has not yet been resolved. There are very conflicting opinions regarding palliative and radical operations, as well as the timing and scope of reconstructive operations.
An operation (colectomy) is performed for emergency indications (intestinal perforation or its threat, massive bleeding), as well as when carcinoma develops in the affected intestine. Often, the indication for surgical intervention is a long, debilitating course of colitis, especially growth retardation, which developed against the background of unsuccessful intensive drug therapy.
The most common surgical treatment for UC is subtotal resection of the colon with ileosigmostomy. After 10-12 months, when the condition has stabilized, reconstructive operations are performed - anastomosis between the ileum and the rectum or sigmoid colon, as well as the formation of a small intestinal reservoir.
Literature
- Zlatkina A. R. Treatment of chronic diseases of the digestive system. M., 1994. pp. 163-217.
- Kanshina O. A. Experience in the treatment of nonspecific ulcerative colitis in children and adolescents // Pediatrics. 1992. No. 1. P. 78-82.
- Levitan M. Kh., Fedorov V. D., Kapuller L. L. Nonspecific colitis. M., 1980. S. 201-205.
- Loginov A. S., Parfenov A. I. Intestinal diseases. M., 2000. P. 32.
- Nosonov E. L. General characteristics and mechanisms of action of glucocorticoids // Breast Cancer. 1999. No. 8. T. 7. P. 364-371.
- Paykov V. L. Pharmacotherapy in pediatric gastroenterology. St. Petersburg, 1998. pp. 188-189.
- Ryss V.S., Fishzon-Ryss Yu.I. Some features of the clinical picture and treatment of nonspecific ulcerative colitis and Crohn's disease // Ter. archive. 1990. No. 2. P. 25-32.
- Frolkis A.V. Modern pharmacotherapy in gastroenterology. St. Petersburg, 2000. pp. 56-57, 62.
- Eaden JA, Abrams K., Mayberry JF The true risk of colorectal cancer in ulcerative colitis: a meta-analysis // Castroenterology. 1999. Vol. 116. P. A398.
- Evans RS, Clarce I, Heath P et al. Treatment of ulcerative colitis wits an engineered human anti-TNF-a antibody CD P571//Aliment Pharmacol Ther. 1997. P. 1031-1035.
- Hanacur SB Inflammatory bowel disease // N. Engl. J. Med. 1996. Vol. 334. P. 841-848.
- Kirschner BS Safety of Azathioprine and 6-Mercaptopurine Pediatric patients wits inflammatory bowel disease // Gastroenterology. 1998. Vol. 115. P. 813-821.
- Prantera C., Scribano ML, Berto E. Antibiotic use of Crohn's disease: Why and how? Bio Drugs, 1997. Vol. 8. P. 293-306.
- Reimund JM, Duclos B., Baumann R. Cyclosporin treatment for severe ulcerative colitis Seven cases // Ann Med Int. 1997. Vol. 148. P. 527-529.
- Rutgeerts P. Medical therapy of inflammatory bowel disease //Digestion. 1998. Vol. 59. P. 453-469.
- Worcester S. Biologic Agent Promising for Children with Crohn's disease // Pediatric News. 1999. Vol. 33. P. 8.
Note!
Conservative treatment of UC in children is based on the following principles:
- diet therapy;
- basic therapy with 5-aminosalicylic acid and/or glucocorticoids (systemic and local action);
- antibacterial agents;
- cytostatics (immunosuppressants);
- immunomodulators;
- symptomatic (“accompanying”) therapy.
Diet for ulcerative colitis
Nutrition is important to prevent exacerbations. If the condition worsens, the diet must be followed. General recommendations:
- limit consumption of dairy products;
- choose foods low in fat;
- reduce the content of coarse fiber in the diet (fresh fruits, vegetables, whole grain cereals). It is better to steam, stew or bake vegetables and fruits;
- avoiding alcohol, spicy foods, and caffeinated drinks.
Also, each patient has “personal” products that aggravate the disease. To identify them, it is useful to keep a food diary.
It is important to eat little and often, drink enough water, and take multivitamins.
Is it possible to be completely cured?
If the diagnosis is made in the early stages and is mild, long-term remission can be achieved, which will last for years or even decades. There are no serious restrictions in the lives of such patients - they study, get a job, get married, have children.
“True, children should avoid open sunlight, intense sports and taking a number of medications (for example, immunomodulators). In general, a healthy lifestyle and reasonable nutrition allow you to avoid relapses of these diseases,” says Elmira Aliyeva.
If you still have questions, you can ask them to a pediatrician or gastroenterologist online in the Doctis application.