Reflux gastritis - what is it?
The stomach is connected to the intestines by special valves - sphincters. Muscles close or open the passage. Digested food enters the intestines through the sphincters. Synchronized muscle activity ensures the normal digestion process. If their motility is impaired, then undigested food remains and gastric juice fall back into the stomach. This pathological process provokes irritation of the mucous membranes of the organ. In medical practice, this disorder of the digestive system is called reflux gastritis or bile reflux gastritis type C.
Features of the disease:
- the disease is difficult to treat and in most cases takes a chronic form;
- the intestinal mixture can corrode the mucous membranes of the digestive organs and disrupt their functional state;
- with reflux damage to the gastrointestinal tract, hydrochloric acid enters the duodenum in large quantities, causing irritation of the walls of the organ.
Risk factors
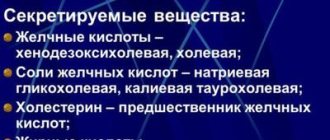
The movement of gastric contents is normal and with reflux. Some pathological conditions significantly increase the risk of reflux damage to the digestive tract. Such diseases include inflammation of the gallbladder, pancreas, and chronic gastrointestinal diseases. A particular risk group includes patients with stones in the kidneys, bladder or bile ducts. Some external factors can increase the likelihood of developing reflux gastritis.
Additional risk factors:
- eating disorder;
- alcohol abuse;
- regular stressful situations;
- uncontrolled use of medications.
How does the surface of the stomach change?
Morphological changes often occur years later. In the section closest to the intestine—the antrum—epithelial cells grow rapidly, and the mucous goblet glands disappear.
The surface becomes swollen, and an accumulation of basophilic leukocytes saturated with nucleic acids is observed. They cause mild inflammation. A long process leads to cell degeneration and then to necrobiosis. Erosion forms and the production of protective mucus stops.
First, a focal process develops. It is possible that areas of mixed inflammation may coexist, alternating with normal mucosa. Subsequently, areas of atrophy grow. If left untreated, the epithelium may transform into malignant with the development of a tumor.
Types of reflux gastritis
Based on the intensity of symptoms, reflux gastritis is classified into acute and chronic forms. In the first case, the development of the inflammatory process occurs at an accelerated pace, in the second - gradually. According to the degree of damage to the digestive tract, the disease is divided into diffuse and focal types. In the first form of pathology, all walls of the organ are affected, in the second - only certain areas. Determining the specific type of disease is necessary to create the most effective course of therapy.
Classification of the disease:
- superficial type (bile regularly enters the stomach, causing gradual irritation of the mucous membranes of the organ; in the absence of therapy, there is a risk of malignant formations);
- biliary type (sphincter muscles completely atrophy, bile is released into all digestive organs, complications of the inflammatory process cause dysfunction not only of the digestive, but also of the nervous and endocrine systems);
- catarrhal type (the inflammatory process affects the deep muscle tissues of the organ, the gastric epithelium undergoes dystrophic destruction, swelling of the mucous membranes occurs);
- erosive type (under the influence of bile, erosions and ulcers form on the epithelial tissue, the inflammatory process is accompanied by intense pain);
- duodenal type (pathological process associated with weakness of the sphincter muscles, complemented by the penetration of harmful substances from the duodenal intestine into the deep layers of the gastric epithelium);
- atrophic type (stomach juice corrodes the mucous membranes and tissues of the digestive organ; of all types of reflux gastritis, this form of the disease is considered the most dangerous).
What is the insidiousness of chronic atrophic gastritis?
There is no general division of chronic gastritis; the typological types of this disease are established according to several criteria. Acute, chronic, antacid, atrophic gastritis and gastritis with reflux are common. The worst thing is chronic focal atrophic gastritis, the treatment of which must be immediate. Its essence is demonstrated in the name: the cells of the glandular tissue caused by the action of death eventually cease to reproduce gastric juice, which negatively affects the functioning of the gastrointestinal tract. Doctors note 2 main causes of the disease: bacteria and autoimmune processes.
Inflammation of the gastric mucosa is often observed under the influence of the bacterium Helicobacter pylori. It is its negative influence that reduces the protective barrier of the mucous membrane; as a result, toxins and free radicals enter the tissues and injure cells. This process promotes the transformation of gastric tissue cells produced by gastric juice into intestinal ones.
Important information! Today, Helicobacter pylori is on the list of biological chemicals. The bacterium is believed to cause stomach cancer. It should be added that more than 85% of the population suffers from this infection. Among young people under 30 years of age, atrophic gastritis is detected only in 5% of cases, in the age category from 30 to 50 years - in 30%. In old age it is detected in 70% of patients.
If we talk about the need for timely detection and treatment, it should be noted that chronic antral focal atrophic gastritis is considered the cause of gastric cancer. If more than 20% of the mucous membrane is subject to proliferation, then the risk of encountering oncology is 100%. In other words, chronic atrophic gastritis transforms into a tumor in 13% of cases. This parameter is 5 times higher than with other types of gastritis. Therefore, the gastroenterologist is faced with the task of creating and maximizing the use of simple and effective methods for accurately diagnosing the disease at an early stage. Timely detection of the disease and the prescription of correct treatment for its causes make it possible to return the functioning of the gastric mucosa to normal and significantly reduce the size of the injured area.
Naturally, the atrophied cells of the stomach walls cannot be restored at this stage of treatment. But the risk of degeneration into a malignant tumor can be minimized by following proper drug therapy, diet and maintaining a healthy lifestyle.
Causes
The main cause of reflux gastritis is impaired motility and weakness of the sphincters. External and internal factors can provoke pathology. In some cases, the disease becomes a consequence of congenital abnormalities in the structure of the digestive system. External provoking factors include poor nutrition, uncontrolled use of medications, abuse of bad habits and constant emotional overload of the body.
Other reasons:
- congenital anomalies of the digestive tract;
- malignant neoplasms in the digestive organs;
- consequences of surgery to narrow the duodenum;
- weakness of the sphincter muscles and decreased motor skills;
- increased intestinal pressure;
- chronic diseases of the digestive system;
- consequences of surgery to remove part of the stomach;
- duodenal obstruction;
- consequences of surgery to remove the gallbladder;
- anatomical displacement of the stomach.
Food normally moves in a certain direction in the stomach.
Symptomatic manifestations
The symptoms of reflux damage to the digestive tract depend on the degree of progression of the inflammatory process. Some signs of the disease are common to all its types. It is difficult to independently determine the type of reflux gastritis. Only a specialist can identify a specific type of pathology by conducting a comprehensive examination of the patient.
General symptoms:
- excessive gas formation;
- cracks in the corners of the lips;
- pain in the solar plexus area;
- regular attacks of nausea or vomiting;
- regurgitation of air;
- white coating on the tongue;
- tendency to heartburn attacks;
- feeling of heaviness in the stomach after eating;
- signs of vitamin deficiency;
- bitter or sour taste in the mouth;
- weight loss due to loss of appetite;
- the presence of bile in the vomit;
- pale skin;
- signs of dehydration;
- release of food residues during belching;
- alternating diarrhea with constipation;
- general weakness of the body.
Respiratory infections in children
According to bronchoprovocation tests (with histamine and methacholine), the third threshold of hyperreactivity was detected in all children with severe BA, in 20% of children with a moderate course of the disease and in 2% of children with a mild form (the differences between the severe form and the other two are significant).
In patients with severe CF, the maximum (third) threshold of hyperreactivity was diagnosed in 66% of children.
In the group of children with recurrent bronchitis III, the hyperreactivity threshold was not diagnosed.
Based on the above, the following conclusions can be drawn:
1) in 65% of children with BA, in 88% of children with CF and 50% of children with recurrent bronchitis, GER of varying severity was detected;
2) a relationship was noted between the severity of GER and the severity of COLD (in severe forms of BA and CF, high-grade GER was detected significantly more often (p<0.05) than in patients with milder forms of these diseases and recurrent bronchitis);
3) in the vast majority of children with COLD who have GER, an endoscopically positive version of the latter has been proven;
4) the most unfavorable is the combination of BA or CF (regardless of the severity) with a sliding hiatal hernia and reflux esophagitis; in these children, significantly more often (p<0.05) than in children with recurrent bronchitis, positive tests with histamine and methacholine with a high threshold of hyperreactivity are detected, and serious disorders are determined according to pulse oscillometry;
5) there was no connection between HP infection and the degree of esophageal damage in children with COLD;
6) all cases of GER-associated BA were identified in children with atopic and/or infectious-dependent forms of this disease;
7) all children with CF should be prescribed a special instrumental examination for early detection of esophageal damage.
Despite significant advances in recent years, there are still many “blank spots” in the topic of respiratory manifestations of GERD in children. In particular, the role of alkaline GER and other non-acidic stimuli in the genesis of respiratory disorders is not fully understood, and not all aspects of the reflex mechanism of reflux-dependent laryngo- and broncho-obstruction have been revealed. The question remains to be answered why only 18–20% of children with pathological GER develop respiratory manifestations to one degree or another, while the opposite situation occurs with a 4-fold prevalence. Answers to these questions may be the topic of future publications.
Diagnosis of pathology
Diagnosis of reflux lesions of the gastrointestinal tract is carried out in several stages. Laboratory and instrumental procedures are prescribed after examining the patient, compiling a list of complaints and collecting an anamnesis. Additionally, a specialist may prescribe daily monitoring of gastric acidity. This procedure is in most cases carried out in a hospital setting. A gastroenterologist diagnoses the disease. If complications are suspected, the patient is scheduled for additional consultation with specialized doctors.
Diagnostic measures:
endocopia - performed using an optical device with a long tube. general blood and urine analysis;- analysis of stool for occult blood;
- biochemical analysis of urine and blood;
- gastroscopy;
- antroduodenal manometry;
- Ultrasound of the gastrointestinal tract;
- radiography of the gastrointestinal tract;
- histological examination;
- biopsy;
- electrogastrography;
- FGDS.
Treatment
Therapy for reflux lesions of the stomach is aimed at eliminating the symptoms of the inflammatory process, improving the functional state of the digestive tract, increasing the protective functions of the body, normalizing the acidity of gastric juice and reducing the aggressiveness of bile. Such results are achieved using an integrated approach. Treatment of the disease is carried out with medications, physiotherapeutic procedures and diet. Additionally, you can use some traditional medicine methods. In case of complications, the patient may undergo surgery.
Drug treatment
If you have reflux damage to the gastrointestinal tract, you should not self-medicate. Drugs are prescribed depending on the degree of damage to the gastric epithelium, the spread of the inflammatory process and the general clinical picture of the patient’s health. Only a specialist can correctly draw up a drug therapy regimen.
Examples of drugs:
Medicines are chosen depending on the cause of the disease and symptoms. Drugs to relieve excess bile production (Urdoxa, Ursofalk, Ursosan);- medicines with an enveloping effect (Pariet, Omez, Omeprazole);
- bismuth-based preparations (De-Nol);
- medications to reduce the acidity of gastric juice (Almagel, Phosphalugel);
- enzyme agents (Creon, Mezim);
- antispasmodics (No-Shpa, Drotaverine);
- antibiotics for infection (Amoxiclav);
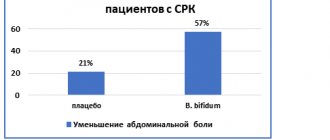
- probiotics (Linex, Bifiform, Bifindumbacterin);
- drugs to restore intestinal motility (Motilak, Motilium).
Treatment with folk remedies
Alternative medicine prescriptions should not be used as the primary treatment for reflux gastritis. Folk remedies improve the digestion process and strengthen local immunity, but they are not able to cure the disease. Recipes based on herbal ingredients can only be used as an addition to drug therapy.
Examples of folk remedies:
- dandelion syrup (plant flowers should be placed in a jar in layers with sugar, crush the mixture until the juice appears, dilute a tablespoon of juice in 100 ml of water, take several times a day);
- herbal mixture (combine yarrow, mint and St. John's wort in equal proportions, pour three tablespoons of the preparation into a liter of boiling water, leave for several hours, take the product in small portions throughout the day);
- potato juice (grate potatoes, squeeze out the juice, take the product in small portions several times a day).
Physiotherapy
Electrophoresis is highly effective in the treatment of reflux lesions of the digestive tract. The standard course of therapy is ten to fourteen days. If there are complications, the doctor may prescribe repeat procedures. Electrophoresis accelerates the tendency to recovery and increases the effect of drug therapy.
Video: Heartburn, reflux - causes and treatment.
Surgery
Surgery is used only in the presence of complications of reflux gastritis. Indications for operations are malignant and benign formations, deep ulcers and erosions, internal bleeding or insufficient activity of the pylorus. The decision about the need for surgical intervention is made by the doctor.
Diet and nutrition
A diet for reflux gastritis implies the exclusion of mechanical, thermal, and physical factors affecting the gastrointestinal tract. Food is consumed only warm. To prepare dishes, methods of steaming, boiling, stewing or baking are used. During the period of exacerbation of the disease, food should have a liquid or semi-liquid consistency. Meals are provided in fractions (at least five times a day). Drinking medicinal mineral water without gas is considered a good addition to the diet.
Other nutritional principles:
- exclusion from the diet of salted, fried, pickled, smoked, fatty, spicy foods;
- sweet pastries, fresh bread and confectionery are prohibited;
- during the period of remission, the menu is supplemented with fermented milk products;
- It is allowed to include vegetarian soups, water-based porridges, steamed cutlets, heat-treated vegetables, and juices into the diet.
Diet for reflux gastritis
Dumping syndrome
Gastritis of the gastric stump and dumping syndrome are postoperative complications, between which there is no direct connection. A patient may have dumping syndrome without inflammation, or inflammation without dumping syndrome. But a situation is possible when dumping syndrome is accompanied by inflammatory processes in the mucous membrane .
Symptoms of dumping syndrome
What is dumping syndrome? In short, this is a common complication of Billroth type 2 gastrectomy with the creation of a gastrojejunostomy. The syndrome manifests itself in attacks with deterioration of well-being after eating . Symptoms increase sharply after eating certain foods, particularly simple carbohydrates and dairy products.
Dumping syndrome is manifested by the following symptoms. 10-20 minutes after eating, a feeling of fullness appears in the epigastric region. The patient complains of weakness, drowsiness, dizziness. Sweating increases and headache occurs. The condition may be accompanied by increased heart rate, chills, tinnitus, shortness of breath, and paresthesia of the skin of the upper extremities. A typical symptom is polyuria (frequent and copious urination).
Development mechanism
The cause of the development of dumping syndrome is the too rapid evacuation of food from the stomach into the intestines through gastrojejunostomy. Since the gastric phase of digestion is virtually absent, food unprepared for absorption enters the jejunum. Such a food bolus has a negative mechanical and chemical effect on the mucous membrane of the small intestine .
As a result of irritation of the mucous membrane in the intestines, blood flow sharply increases. In simple words, “blood rushes to the intestines.” Due to the large difference between the osmotic pressure of the blood and the food bolus (the osmotic pressure of food is much higher), fluid from the vascular bed exits into the lumen of the small intestine . Accordingly, hypovolemia develops (the volume of circulating blood decreases), and cerebral circulation suffers.
Deterioration of cerebral perfusion is the main reason for the development of symptoms such as dizziness, weakness, tinnitus, and drowsiness. A decrease in blood volume provokes shortness of breath and tachycardia. Mechanical irritation of the intestines is accompanied by a feeling of fullness in the epigastric zone.
There is a humoral component in the pathogenesis of dumping syndrome. The acute phase is accompanied by the release of catecholamines (norepinephrine) with activation of the sympathetic nervous system; hence the tremors in the hands, tachycardia, increased systolic pressure. Diastolic pressure is usually reduced.
In addition, cells of the gastroenteropancreatic endocrine system secrete the hormones motilin and enteroglucagon. Motilin enhances small intestinal and also increases kidney perfusion with increased urine formation. This explains another symptom of dumping syndrome - polyuria.
At the end of the attack, patients feel rumbling in the abdomen (explained by increased peristalsis under the influence of motilin). The attack ends with diarrhea, which has a simple explanation: the osmotically active bolus of food retains a large volume of liquid in the intestine, which is excreted with feces.
Dumping syndrome: degrees of severity
In mild forms of dumping syndrome, attacks occur rarely, only 1 or 2 times a month. They are always provoked by dietary violations, namely, the consumption of dairy products and/or simple carbohydrates. The attack does not last long, from 15 minutes to half an hour, and proceeds easily. The mild form does not require special treatment. It is enough for the patient to exclude foods that provoke attacks.
Dumping syndrome of moderate severity occurs with frequent exacerbations, 3-4 times a week. The attack lasts up to an hour and a half and is accompanied by a significant deterioration in well-being. The clinical picture contains many of the symptoms listed above.
Due to frequent attacks, metabolic processes suffer. The balance of electrolytes (mainly potassium, sodium, calcium, chlorine) is disrupted. Loss of calcium negatively affects bone mineralization. Patients are weakened, lose weight, and many develop anemia.
Despite the pronounced manifestations and serious consequences, with moderate severity, dumping syndrome is treated conservatively. Only if conservative therapy is ineffective is the need for surgery considered.
Severe dumping syndrome is characterized by daily attacks that occur with a sharp deterioration in health, up to loss of consciousness. Nutrition is disrupted, patients suffer from exhaustion and cachexia. Demineralization of bone tissue is observed, and osteoporosis develops. Working capacity is sharply reduced. Conservative treatment is ineffective. Patients are indicated for surgical treatment with reconstruction of the upper gastrointestinal tract by creating a gastroduodenoanastomosis.
Complications
With reflux gastritis, the inflammatory process spreads to the tissues and mucous membranes of the digestive organs. The functional state of the gastrointestinal tract is disrupted. The consequence of irritation of the walls of the intestines and stomach is the formation of erosions and ulcers. Numerous ulcerations can cause internal bleeding. The risk of peritonitis, which poses a threat to the patient's life, will increase.
Other complications:
- reflex laryngospasm;
- peptic ulcer;
- precancerous condition;
- perforation of the intestinal and stomach walls.
Prevention
One of the main preventive measures for reflux gastritis is diet. The diet can significantly prolong periods of remission. Violation of the nutritional program will provoke an exacerbation of the inflammatory process. Prevention also includes a number of recommendations that can improve the condition of the gastrointestinal tract and the body as a whole.
Other preventive measures:
- elimination of bad habits (alcohol abuse, smoking);
- strengthening the immune system (active lifestyle, replenishing the supply of vitamins in the body);
- complete and timely treatment of diseases of the digestive system;
- taking medications strictly according to the instructions or indications of the doctor;
- preventing excessive emotional stress on the nervous system;
- exclusion of a sedentary lifestyle.