In gastroenterological diagnostics, laboratory tests are carried out to establish or confirm the diagnosis, differentiate with other forms of the disease, assess the dynamics of lesions and assess the functional reserves of the digestive system.
While the diagnosis of diseases of the digestive system, both upper and lower, is based primarily on imaging studies, laboratory tests are widely used in the diagnosis of diseases of the liver and pancreas. In addition to morphological tests, this is the main element of diagnosis.
Biochemical research
Laboratory tests in the diagnosis of diseases of the upper gastrointestinal tract play a supporting role in assessing the development of the disease.
- Morphology of peripheral blood.
Anemia indicates the intensity of bleeding. Anemia can also result from chronic malnutrition or cachexia, such as from cancer. Inflammation of the mucous membrane of the stomach and duodenum, as well as malabsorption syndromes, can cause iron deficiency anemia, folic acid or vitamin B 12 (often accompanied by low levels of cholesterol, calcium and albumin). - Violation of water and electrolyte balance.
Vomiting can lead to fluid and electrolyte imbalance, such as hypokalemia and alkalosis. Malnutrition is accompanied by hyponatremia. Vomiting and malnutrition with associated electrolyte disturbances often result from impaired gastric emptying or gastroparesis. This occurs due to disorders of the nervous and muscular systems of the digestive tract, metabolic diseases, or other pathologies not primarily related to the digestive system. - Gastrin concentration.
Gastrin concentration is determined when diagnosing Zollinger-Ellison syndrome (in healthy people it does not exceed 150 pg/ml). Values >150 pg/ml (or 10 times normal at gastric pH <2.1) are characteristic of Zollinger-Ellison syndrome—in some patients they can reach 100,000 pg/ml. If gastrin concentration cannot be assessed, increased basal gastric acid secretion (BAS) > 15 mmol/h is of great diagnostic value.
Instrumental research methods
They represent an important section of a comprehensive examination of patients with gastrointestinal problems. They include X-ray, endoscopic, ultrasound, electrographic and electrometric methods. Depending on the nature of the disease, the doctor prescribes a certain examination. Some of the most common methods are ultrasound, CT and MRI; you can check the prices for examinations during your appointment.
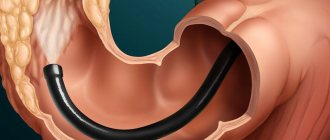
- Endoscopic examination of the gastrointestinal tract
Endoscopy is an examination consisting of direct examination of the internal surface of various parts of the abdominal or tubular organs of the abdominal cavity (esophagus, stomach, duodenum, colon) using special devices - endoscopes. Modern endoscopes are a flexible tube equipped with an optical system in the center. The technical perfection of the devices ensures absolute safety of diagnostic procedures for the patient during the appointment. Endoscopy in gastroenterology is used to study the esophagus (esophagoscopy), stomach (gastroscopy), duodenum (duodenoscopy), rectum and sigmoid colon (sigmoidoscopy), and the entire colon (colonoscopy). - Ultrasound examinations of the digestive organs
Ultrasound diagnostics (ultrasound) - (echography, echolocation, ultrasound scanning, sonography, etc.) is based on the ability of ultrasonic waves, focused and directed in a certain way, to be partially reflected or absorbed when passing through tissues or organs of the abdominal cavity with different densities . The doctor gives you a referral for an ultrasound so that you can determine the shape, size, position, structure of the liver, gallbladder, pancreas, identify tumors, cysts, stones (stones), vascular disorders, damage to the ducts and others. - X-ray examination of the gastrointestinal tract
X-ray examination of the gastrointestinal tract allows us to clarify the shape of the internal organs, their position, the state of the relief of the mucous membrane, tone, and peristalsis. Never ignore a referral for an x-ray, because this method plays an important role in the diagnosis of peptic ulcers, tumors of the gastrointestinal tract, anomalies in the development of cholelithiasis, enlarged pancreas, and more. X-rays are also important in identifying complications (gastric stenosis, penetration of ulcers, varicose veins of the esophagus, dolichosigma, megacolon, etc.), as well as assessing the nature of functional (motor-evacuation) disorders. X-rays are widely used in gastroenterology for the study of blood vessels.To study the state of the blood supply to the object being studied, a radiopaque substance is injected into the corresponding artery and a series of radiographs are taken. This makes it possible to highly effectively diagnose ischemia (circulatory failure) of the digestive system, tumor processes, consequences of injuries and other pathological conditions at the appointment.
You can check the prices for examinations during your appointment.
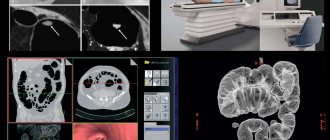
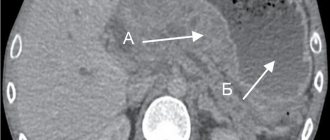
- Computed tomography
Computed tomography (CT) allows you to obtain x-ray images of tissues at any depth of their location, conduct layer-by-layer studies of tissue structures from the edges to the center, reproducing the size, density, structure and some other characteristics of the objects under study with great accuracy. But high quality X-ray equipment is important. The Neva Clinic uses only modern medical CT equipment, which allows obtaining highly informative images of good quality. - Radioisotope studies of the digestive organs
Radioisotopes are an important section in the diagnosis of diseases of the liver, biliary system, pancreas, etc. Scanning is used to study the condition of the liver in the diagnosis of hepatitis, cirrhosis, neoplasms, thyroid gland and kidneys involved in the development of gastrointestinal pathology.Radioactive isotopes are also used to study absorption in the small intestine, determine the nature of disorders and localization of damage to the biliary system, identify the characteristics of the pathological process in the pancreas, and circulatory disorders in the liver.
- Electrometric and electrographic studies in gastroenterology
In hospitals and clinics, a number of methods are used to study certain parameters of the functional activity of the gastrointestinal tract: stomach - electrogastrography, intestines - electrointestinography, rheography is used for mucous membranes, and phonogastrography and phonointestinography (recording of sounds in Gastrointestinal tract). - MRI
The magnetic resonance imaging (MRI) method is one of the modern non-invasive (does not require intervention in the human body) methods. MRI is based on the interaction of an external magnetic field with hydrogen atoms, one of the main elements of the human body.MRI provides an exceptional opportunity to visualize the internal structure of the body in comparison with ultrasound and CT. During an appointment, MRI allows you to construct both two-dimensional images of sections of the area under study up to tenths of a millimeter thick, and make a three-dimensional reconstruction of the tissues required for diagnosis. Compared to CT and ultrasound, MRI provides more opportunities to study the condition of diseased organs, but sometimes they are simply not needed. Then the attending physician at the appointment gives preference to CT or ultrasound.
You can check the prices for examinations during your appointment.
Take care of your health!
Gastrointestinal diseases can manifest as discomfort or pain, or they can be practically asymptomatic. But they don’t go away on their own, unfortunately. Without seeing a specialist and appropriate treatment, the pathology only worsens and can spread to other organs. Everything in the human body is closely interconnected. Therefore, for example, gastric disorders will sooner or later lead to problems with the liver and intestines.
Preventative screenings (such as CT, MRI and ultrasound - you can check the prices for screenings when you make an appointment), following your doctor's orders and getting regular tests can prevent the development of many serious complications (and surgery visits) and maintain a high quality of life for many years.
Department of Gastroenterology, Neva Clinic
At the Neva Clinic, doctors care not only about your health, but also about a comfortable stay and delicate solution to various problems of patients of any age. We do not have queues or referrals to hard-to-reach laboratories; you can make an appointment at a time convenient for you. You can undergo examination (CT, MRI and ultrasound; you can check the prices for examinations during the registration), receive treatment and receive a full package of medical services on an outpatient basis, without interrupting work or study.
In our gastroenterology center in Moscow, it is possible to undergo various laboratory and instrumental studies (CT, MRI and ultrasound) and always receive doctor’s services on time and in full. It is important that such unpleasant medical procedures, such as gastroscopy, take place without pain and discomfort, since modern technology of minimal size is used, and the areas of the body being examined are irrigated with special “freezing” (painkillers) substances during the procedure.
All doctors at the Neva Clinic constantly improve their skills by attending symposiums and seminars. Thus, we use the latest technical developments and modern safe drugs to achieve maximum accuracy in diagnosis and 100% effectiveness in treatment of even the most persistent and recurrent lesions. The use of disposable consumables from European manufacturers guarantees the safety of our services at all stages of admission, diagnosis and treatment.
And remember, the best treatment is preventative. Regular examinations and timely visits to a doctor for advice will help avoid many unpleasant consequences.
Therefore, do not delay your visit to the Neva clinic and hurry to make an appointment with a gastroenterologist!
- Make an appointment
Serological tests - testing for Helicobacter pylori infection
Helicobacter pylori infection is detected by the presence of IgG against Helicobacter pylori in the blood serum. The sensitivity of the test is 80-95%, specificity 75-95%.
Antibody titers usually decline within 6–12 months of infection but often remain elevated for a long time. Serological tests do not provide definitive information about the timeliness and activity of infection and are not recommended for assessing eradication effectiveness. The test for the detection of H. pylori antigens in feces has a sensitivity and specificity of >90%.
2.When is the composition of digestive secretions studied?
The study of the composition of digestive secretions is used for:
- Helicobacter pylori infection,
- peptic ulcers,
- gastroduodenitis,
- atrophic gastritis,
- dyspepsia,
- during the period of taking antisecretory drugs to assess their effectiveness.
Gastric juice is collected for analysis on an empty stomach
. Its study should be carried out immediately, since over time a number of substances disintegrate and some indicators of the secretory fluid change.
Laboratory diagnosis of diseases of the small intestine
- Diagnosis of neuroendocrine neoplasms and the concentration of 5-hydroxyindoleic acid in urine.
When diagnosing carcinoid tumors, cancers of the small intestine that produce serotonin, it is useful to measure the concentration of the serotonin breakdown product in the urine, 5-hydroxyindoleic acid (5-HIAA). In carcinoid syndrome, its concentration in a 24-hour urine sample increases, usually >30 mg. - Serum chromogranin A concentration.
Neuroendocrine cells produce, store, and release chromogranin A (CgA) into the blood. The concentration of this protein is increased in metastatic carcinoid tumors and in other hormonally active tumors of the gastrointestinal tract (GEP-NET - gastroenteropancreatic neuroendocrine tumors). The sensitivity of the test ranges from 10 to 100%, specificity from 68 to 100%. The most sensitive determination of chromogranin A is for gastrinoma, glucagonoma and carcinoid syndrome. It is also an important marker in disease monitoring and a prognostic factor in patients with carcinoid syndrome. - Infections.
When diagnosing and differentiating infectious diarrhea, stool culture is carried out for Campylobacter, Shigella, Salmonella and Yersinia.
Why is self-medication dangerous?
Often, the consequence of the disease becoming chronic is self-medication, which only aggravates the course of the disease, bringing only a temporary improvement in the patient’s condition. Do not forget that a disease of one organ of the digestive system, progressing uncontrollably, can provoke the spread of the pathological process to others, therefore a combination of gastritis and pancreatitis, cholecystitis and pancreatitis, etc. is often observed.
There are other reasons for the emergence and aggravation of any pathological process - determining the etiology of a particular case should be entrusted to a specialist.
Malabsorption syndromes
Biochemical research.
Laboratory diagnosis of diseases of the small intestine is based on laboratory tests of blood, stool, stress and provocative tests. They are performed primarily in the evaluation of disorders of digestion and absorption of carbohydrates, fats and protein-losing enteropathy (intestinal protein-losing syndrome).
Blood tests.
In blood serum it is determined (depending on the degree of deficiency of nutrients, minerals and vitamins):
- microcytic anemia due to iron deficiency;
- macrocytic anemia due to deficiency of vitamin B 12 or folic acid;
- hypocalcemia, hypophosphatemia, hypomagnesemia;
- metabolic acidosis;
- hypoalbuminemia;
- sometimes hyponatremia;
- deficiency of fat-soluble vitamins (A, D, E, less often K).
The abnormalities mentioned may also be the result of short bowel syndrome after a large portion of the small intestine has been removed.
Stool tests
- PH assessment. A stool pH test strip is useful in assessing digestion and carbohydrate absorption problems. Correct values are in the range of 7.0-7.5; PH <6.0 indicates impaired digestion and absorption of carbohydrates.
- Test for the presence of reducing substances (Clinitest). The presence of reducing substances in the stool: glucose, lactose, fructose, galactose and pentose indicates disturbances in the digestion and absorption of carbohydrates. The test (reduction of copper cations) consists of mixing 0.5 ml of feces with twice the amount of distilled water. Then copper salts and sodium hydroxide are added and the color of the resulting suspension is compared with the standard. Under normal conditions, the amount of reducing substances in the stool does not exceed 0.25%, 0.25-0.5% is a questionable result, and > 0.5% is clearly an incorrect result. The study is used, in particular, to distinguish between infectious diarrhea and diarrhea caused by disorders of digestion and absorption of carbohydrates. In a patient with glycosuria, if the stool sample is contaminated with urine, the test may give a false-positive result.
- Osmotic gap. The concentration of electrolytes and osmolarity of the stool make it possible to calculate the osmotic gap - on the basis of this, osmotic (fermentation) and secretory diarrhea are distinguished. The osmotic gap is calculated by the formula: osmotic gap = expressed osmolarity - calculated osmolarity, or, osmotic gap = 280 - calculated osmolarity. Formula for calculated osmolarity: Calculated osmolarity = 2 × . An osmotic gap of >125 mOsm/kg indicates osmotic diarrhea, and <50 mOsm/kg indicates secretory diarrhea.
Why do digestive problems occur?
Diseases of the digestive system are often caused by poisoning, for example, in the case of consuming low-quality or expired products, alcoholic beverages, which cause irritation of internal organs and lead to their dysfunction.
A frequent cause of serious disturbances in the functioning of the digestive system are diets and fasting that have become fashionable, used without the advice of a specialist, which is absolutely unacceptable.
Any independent restriction in normal nutrition affects the state of health, leading to such disorders as gastritis, cholecystitis, pancreatitis, etc. We must not forget that diet is an exclusively therapeutic measure, carried out, if necessary, as prescribed by a professional doctor.
Microscopic evaluation
Microscopic Evaluation
Microscopic evaluation of smears of a fresh stool sample ground with 0.9% NaCl on a glass slide is useful in the diagnosis of digestive and fat absorption disorders. Undigested food remains, starch grains or muscle fibers are detected. After adding 1% Sudan III, red neutral fat globules become visible. Actually, their number is <60-80 in the field of view at 400x magnification.
- Estimation of fat excretion from 72-hour fecal collections.
Correct result: <6 g/24 h. Increased fecal fat excretion (15-35% of ingested fat and >6 g/24 h) is observed with disorders of digestion and fat absorption. - Evaluation of α 1-antiproteinase excretion.
When diagnosing protein malabsorption disorders (intestinal protein loss syndrome), a quantitative assessment of the excretion of α 1 -antiproteinase in feces or (more often) its concentration in feces is determined. α 1 -antiproteinase is an endogenous protein that is not sensitive to the action of proteolytic enzymes. Its normal concentration in feces does not exceed 0.62 mg/g.
Lactose tolerance test
The lactose tolerance test is based on determining serum glucose levels in the fasting state (baseline) and after oral administration of 100 g of lactose dissolved in 300 ml of water every 30 minutes for 2 hours.
Typically, there is an increase in glucose levels of 1.11–1.67 mmol/L (20–30 mg/dL) from baseline in the first 90 minutes. The absence of an increase in blood glucose levels 20-30 mg/dl above the baseline value and clinical signs of hypolactasia indicate lactose deficiency.
The specificity of this test is estimated at 80%, sensitivity - 75%. However, according to some authors, such an amount of lactose is unphysiological and can cause intolerance even in healthy people.
Hydrogen breath test
This is not a typical laboratory test. Its essence is to determine the amount of hydrogen in the exhaled air every 30 minutes for 2 hours after consuming 50 g of lactose (or 25 g of glucose, galactose or fructose).
The patient should not eat 8 hours before the examination. Normal values do not exceed 20 ppm. In people with lactase deficiency, unabsorbed lactose reaches the colon unchanged. There it is broken down by bacteria, producing large amounts of free hydrogen. In people with lactase deficiency, after oral administration of lactose, an increased concentration of hydrogen in the exhaled air persists for several hours.
For carbohydrate malabsorption, there is an increase of 20 ppm (parts per million) from the lowest value recorded during the test. With excessive growth of bacterial flora in the small intestine, an increase of 20 ppm occurs within the first hour of the test. Because of its high sensitivity, this test is preferred for diagnosing lactose intolerance syndrome. Contraindications: galactosemia and hereditary fructose intolerance. People taking antibacterial drugs may have false negative results.
Modern ultrasound options
In certain clinical situations, more modern techniques are especially useful:
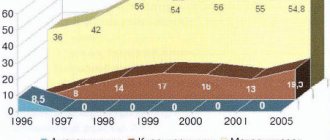
- Endoscopic ultrasound. (EUS - endoscopic ultrasound) allows you to identify small focal lesions of the pancreas, diagnose chronic pancreatitis and evaluate the local spread of esophageal cancer.
- Laparoscopic ultrasound examination. Allows recognition of neoplastic metastases in the peritoneum and small tumor metastases elsewhere.
- Contrast enhanced ultrasound (CEUS). Allows dynamic assessment of the vascularization of focal lesions. The 2nd generation contrast agents used today consist of microbubbles of gas (sulfur hexafluoride) in a phospholipid shell. They are classified as blood pool compounds, which means they do not enter the extravascular space. Providing only contrast enhancement to a degree dependent on the vascularity of the lesion being examined.
A contrast agent administered intravenously allows real-time assessment of all phases of liver vascularization (arterial, portal, late).
Observation of contrast enhancement in certain phases of the vessels makes it possible to more effectively detect focal lesions in the liver and differentiate them than in the case of classical ultrasound (the use of a contrast agent increases the sensitivity of ultrasound in the diagnosis of focal liver lesions by 30-40%).
D-xylose test
After oral administration, D-xylose is absorbed in the proximal small intestine and, due to slow metabolism, is almost completely filtered through the kidneys. After oral administration of 5 g of xylose, depending on the method used, the following is determined:
- Serum D-xylose concentration (normal >20 mg/dL);
- Urinary excretion of D-xylose (> 25%, i.e. 1.25 g, should be excreted in urine within 5 hours, half of this in the first two hours).
Decreased excretion of D-xylose is characteristic of malabsorption syndromes. The study has some limitations:
- Xylose is absorbed in the proximal small intestine, so the result may be normal despite significant damage to the distal small intestine, such as in Crohn's disease;
- Renal impairment may (due to decreased xylose excretion) produce false-positive results;
- Edema is also a cause of a false-positive test result, since the concentration of xylose in serum and its excretion in urine depend in part on the size of the aqueous space.
Despite its great utility, the D-xylose test is used less and less due to the availability of more accurate diagnostic methods.
Types of ultrasound
It is impossible to make a diagnosis based on ultrasound results alone.
There are several types of diagnostics of the esophagus. For each patient, the doctor determines the type that is suitable for him, based on the anatomical characteristics of the patient and his test results.
The doctor chooses a suitable research method from among the following types:
- Percutaneous ultrasound. This type is most common when examining children. A special sensor is located on an area of the patient’s skin pre-lubricated with gel in the neck, epigastrium and upper abdominal cavity. This makes it possible to visualize different parts of the organ. To better visualize the esophagus, the doctor may ask the patient to tilt their head back slightly.
- Intraesophageal ultrasound. A special small sensor is inserted directly into the lumen of the esophagus. This allows you to diagnose all layers of the walls of the esophagus and determine whether there are structural changes in them. In children, this method is practically not used due to the likelihood of mechanical damage to the esophagus. This method is also used to study the functioning of the heart muscle.
- Ultrasound with water-siphon test. This method is used to study the motility of the esophagus and stomach. During this type of diagnosis, the patient drinks a certain amount of water, which contrasts the organ cavity.
- Endosonography (endoultrasound). This examination for the patient is similar to gastroscopy and is performed with a special ultrasound sensor, which, together with an optical device, is attached to the end of the endoscope. It allows you to examine in detail areas that are inaccessible to conventional ultrasound examination, and detect changes up to 1 mm in size. This type allows not only to diagnose a neoplasm, but also to determine which layers of the organ it has affected, and what area of the organ it has affected.
Serological tests in the diagnosis of celiac disease
The enzyme immunoassay (ELISA) method determines:
- IgA antiendomism (EmA), characterized by high sensitivity (87-100%) and specificity (98-100%);
- IgG antiendomism (sensitivity 85-98%, specificity about 98%);
- IgA anti-tissue transglutaminase (tTG) (sensitivity 90-98%, specificity 95-98%);
- IgG against tissue transglutaminase (sensitivity 21-98%, specificity 98%);
- Anti-gliadin antibodies (AGA) with much lower specificity than previously mentioned (often found in other gastrointestinal diseases, such as Crohn's disease);
- Antireticulin antibodies (ARA) (sensitivity 76-87%, specificity 96-100%).
Biochemical research
In the diagnosis of diseases of the colon, biochemical tests are only of auxiliary value.
Basic blood tests
In severe forms of ulcerative colitis and Crohn's disease, the following are observed:
- decrease in hemoglobin;
- leukocytosis;
- deficiency of iron, vitamin B 12 and folic acid;
- electrolyte disturbances (hypokalemia, metabolic alkalosis);
- hypoalbuminemia (due to malnutrition or protein-losing enteropathy);
- increased ESR and CRP.
These abnormalities correlate well with the severity of the disease. Abnormal values of parameters characteristic of hepatocyte damage and biliary stasis may indicate coexisting primary sclerosing cholangitis.
Sequence of ultrasound
The patient lies on the couch, on his back, then the doctor applies a special gel to his neck and abdomen. By moving the sensor over these areas, the doctor examines the patient’s organs on the monitor. During the procedure, the patient is asked to drink a little water to study the characteristics of its flow from the esophagus to the stomach.
For better visualization of certain organs or parts thereof, the diagnostic physician may ask the patient to lie on his side. The whole procedure takes up to half an hour. When preparing the results, the doctor describes the echogram, indicates the presence or absence of pathologies and summarizes the general condition of the organs being tested.
Carcinofetal antigen
For colorectal cancer, determination of carcinoembryonic antigen (CEA) in serum has little diagnostic value, but is important in the following cases:
- assessment of prognosis for colorectal cancer;
- monitoring the course of colon cancer after surgery and detecting relapse.
Normal values in healthy and non-smoking people should not exceed 5.0 ng/ml, and in smokers - 10 ng/ml. In patients with elevated preoperative CEA levels, it should return to normal values after radical surgery; regrowth indicates relapse (local or distant metastasis).
The absence of a decrease in CEA concentration after the procedure proves its non-radical nature. Conversely, an increase in concentration is >90% likely to indicate tumor recurrence.
In other clinical situations, CEA synthesis is also enhanced:
- For cancer of the pancreas, stomach, breast, lungs, reproductive organ, bladder;
- For non-epithelial neoplasms (neuroblastoma, sarcoma, lymphoma).
For non-malignant diseases:
- hepatitis;
- cirrhosis of the liver;
- chronic pancreatitis;
- ulcers of the stomach and duodenum;
- ulcerative colitis;
- during pregnancy.
Features of ultrasound in the diagnosis of gastrointestinal pathologies
The content of the article
Ultrasound in view B allows you to evaluate:
- size;
- echogenicity;
- echostructure;
- surface of parenchymal organs;
- and also detect focal changes.
Under ultrasound control the following is carried out:
- diagnostic biopsy;
- control of healing after surgery;
- alcoholization and thermal ablation of liver tumors;
- drainage;
- other procedures.
Disadvantages of the examination:
- Dependence of the result on the experience of the attending physician;
- Difficulty in examination if the patient is unprepared;
- Difficulty in assessing due to obesity, distended intestinal loops, fresh wounds.
Most lesions diagnosed by ultrasound require further imaging to determine their nature and extent.
Serological studies
Serological tests are performed to differentiate inflammatory bowel diseases:
- Antineutrophil cytoplasmic antibodies (ANCA) occur in 60% of patients with ulcerative colitis and 10% of patients with Crohn's disease;
- Anti-Saccharomyces cerevisiae (ASCA - antibodies against Saccharomyces cerevisiae) are present in 60% of patients with Crohn's disease and only 10% of patients with ulcerative colitis.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
Registration of research results
It should be said that ultrasound is not a complete replacement for such types of diagnostics as radiography or endoscopy. However, it allows you to assess the condition of tissues, organ contours, and identify the presence of pathologies.
The diagnostic protocol contains information regarding the thickness of the stomach walls, the presence of foci of inflammation, tumors, tissue structure and blood flow characteristics. This method makes it possible to identify most diseases of the digestive tract.