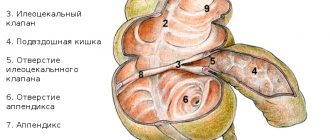
The intestinal valve is a tightly closed fold of natural origin formed at the junction of the small and large intestines. Its functional purpose is to ensure the movement of intestinal contents in the direction from the ileum to the cecum.
Insufficiency of the ileocecal valve (another name for this organ) causes the reflux of food masses in the opposite direction. The Bauginian valve, when its functionality is impaired, leads to congestion of the small intestine with the microflora of the large intestine and, as a consequence, its inflammation. Regular manifestation of this pathology causes a disease called chronic enteritis.
Causes of the disease
The Bauhinian valve, the shape of the opening of which can be open round, closed-lip-shaped, semi-open-slit-shaped, may stop performing its natural functions for the following reasons:
- congenital anatomical anomalies and defects;
- consequences of surgery;
- inflammatory processes in nearby organs, for example the ovaries;
- the presence in the body of pathogenic microbes that enter with food;
- neurological diseases.
Insufficiency due to psychosomatics
Separately, I would like to highlight the causes of a psychosomatic nature, which are the provocateurs of almost half of all diseases of the gastrointestinal tract. Psyche and somatics (soul and body) are an integral, unified system with a strong interconnection of components. Any deep emotional experience affects a person’s physical health, and, conversely, poor health directly affects thoughts, mood, and behavior. The Bauginian valve, the treatment of pathologies of which is successful in most cases, is also no exception and can become inflamed for psychosomatic reasons.
The importance of the ileocecal intestine in colon surgery
Modern ideas about the functional significance of the ileocecal part of the intestine, primarily the ileocecal valve (ICV) and the terminal part of the ileum, are quite contradictory. Suffice it to say that to this day there remains terminological confusion in the naming of the anatomical formations of this area (Sax F.F. et al. 1994)
One might assume that in surgical practice the question of the degree of participation of the ICC and the terminal ileum in the coordinated activity of the digestive tract should be resolved relatively simply, since functional results with their preservation or removal can be compared (quality of life). It turns out, however, that this simplicity is apparent; while studying the same phenomenon, authors often come to directly opposite conclusions. Both in domestic and foreign literature there is serious evidence confirming the functional significance of the ICC and the terminal part of the ileum both in the motor-evacuation activity of the entire gastrointestinal tract (gastrointestinal or bisphiicteric reflex), and in the absorption and metabolism of certain substances, primarily vitamin B12 , the deficiency of which in the body can cause B12 deficiency anemia; bile and fatty acids, considered as “endogenous laxatives”; fat-soluble vitamins - A, D, E, K. Even limited resection of the ileum, unlike the jejunum, accelerates the transit of chyme by 2-3 times (Booth S.S. et a1, 1959) The ileocecal section of the intestine ensures a portioned supply of chyme to the large intestine after completion of hydrolysis and absorption of essential nutrients, it prevents the penetration (reflux) of colonic microflora into the small intestine (similar to a mechanical barrier) and, based on the feedback principle, has an inhibitory effect (“ileal brake”) on the motility of the proximal digestive tract (Jackson I.M. , 1949; Dyskin E.A., 1960, Melman E.P., 1970, Vitsyn B.A. et al., 1977; Fedorov V.D., Nikitin A.M., 1985; Lebedev N.N., 1987; Baltaitis Yu .V., 1990, Frolkis A.V., 1991, Lundqvist N. et al., 1975, Nasmyth DG, Williams NS, 1985, Phillips SF et al., 1988, Soper NJ et al.. 1990, Faussone PMS et al. , 1995)
On the other hand, there are reports of the insignificant role of the ileocecal part of the intestine in the regulation of the activity of the gastrointestinal tract (Johansson N., Nylander G., 1969, Neal DE et al, 1984) and the limited influence of the ileocecal sphincter on the passage of intestinal contents in this area (Kruis W. et al., 1987, Nen M. et al., 1991). Recently, probably the most compelling argument regarding the influence of the ileocecal region on the motility of the digestive tract (stomach, small and large intestines) has been the work of M von Flue et al. by transposition of the ileocecal segment in an isoperistaltic position to the site of the removed rectum (von Flue M., Harder F., 1994, von Flue M.O. et al., 1996, Degen L..P. et al., 1997). However, the authors did not note any significant differences in the transit of contents throughout the digestive tract
The conclusions of some researchers regarding the physiological significance of the ICC and the terminal part of the ileum are contradictory. So, I.N. Siparov, N.G. Lud (1888) first draw attention to the fact that “if the ileocecal angle is removed and the terminal section of the ileum (7-15 cm) is resected, then, as a rule, the motor-evacuation function of the gastrointestinal tract is not disturbed,” and then they completely conclude the opposite: “... the motor-evacuation function of the stomach and the passage of the contrast agent through the small intestine depend on the ileocecal interoceptive zone and, mainly, on the terminal ileum.” The same uncertainty can be traced in the article by R.A. Melnikova et al (1966) in their opinion, in patients who underwent subtotal colectomy with ileorectal anastomosis, “the absence of ICC does not have a significant effect on the frequency of stool in the long-term postoperative period,” although (further) “of course, the two most important ones should be preserved whenever possible.” biologically, the sphincter is the ileocecal valve and the sphincter of the rectum.”
We believe that for the correction of postcolectomy and postcoloproctectomy syndrome, the preservation of the ileocecal valve, and with it the terminal ileum, has a certain positive significance (Zhukov B.N. et al., 1993, Isaev V.R. et al., 1998) . It is likely that with right hemicolectomy, where a significant portion of the colon remains, the loss of FCI will be compensated over time. It is also possible that with transposition of the ileocecal section, this segment of the intestine loses its regulatory function, thereby becoming a kind of reservoir (although back in the 60s, V.M. Veldchenko established the existence of constant neuroreflex connections between the ileograft and other parts of the digestive system - intestines, stomach, salivary glands). During colectomy and coloproctectomy, the situation dictates a saving attitude towards everything that can be saved, because “the assumption that with the help of various techniques and the formation of intussusception anastomoses can actually be replaced by the Bauginian valve is hardly justified” (Vorobiev G.I., 1994).
The problem of using ICC is also becoming relevant because now during extended operations on the colon there is a tendency to preserve the direct line, especially in emergency surgery and in severe general condition of the patient (Vorobiev G.I. et al., 1999 a, b, Oleinikov P.N., 1999; Savchenko N.F. et al., 1999)
When performing a colectomy or subtotal colectomy, if there are no contraindications, it is possible not to mobilize the ileocecal region, but the continuity of the intestinal tube between the ICC and the rectum or sigmoid colon can be ensured by using an ileointestinal autograft in an isoperistaltic position. Our experimental studies on animals have proven the fundamental possibility of performing the same operation, but with a small intestinal autograft simultaneously in the iso- and antiperistaltic position (operation diagram. ICC - isoperistaltic intestinal insert - antiperistaltic intestinal insert - anastomosis with the rectum or sigmoid colon). Only with this type of surgical intervention is it possible to preserve the ICC and take advantage of the slowdown in the transit of intestinal contents (antiperistalsis).
It was only after completing our experimental studies using the isoantiperistaltic ileal insert that we learned that the idea of such an operation had been put forward and developed. G.-P. Schrader in 1972 for gastric replacement after total gastrectomy (Kieninger G. et al, 1979).
The surgical options we offer are not always feasible. They assume at least a satisfactory general condition of the patient, and this practically does not happen in emergency surgery. Performed in a planned manner, such operations must be well supported financially (formation of four interintestinal anastomoses, a lot of time). With a protracted recurrent course of nonspecific ulcerative colitis, the ileum (backwash ileatis) is also involved in the inflammatory process, and the ICC becomes sclerotic, deformed and ceases to function. Diffuse polyposis of the colon can be complicated by malignancy of polyps in the right half of the colon - and then it is necessary to remove both the ICC and at least 10-15 ohms of the terminal part of the ileum.
Here is one of the clinical observations:
Patient K.G.A., 49 years old (case history No. 16788/1355), disabled 2 gr. Hospitalized in October 1999. Clinical diagnosis: UC with total damage to the colon, continuously relapsing course, exacerbation stage. Chronic cholecysto-pancreatitis, Chronic gastraduodenitis, Chronic B12 and iron deficiency anemia. Clear signs of nutritional dystrophy (loss of body weight up to 30 kg: with a height of 167 cm, weighs 45 kg). Complaints of severe general weakness, loss of appetite, pain in the abdomen (mainly on the right), loose stools mixed with mucus and blood up to 5-10 times a day.
She has been ill since 1979. She was treated in various hospitals in the city and in outpatient clinics. In complex therapy - drugs such as sulfasalazine, glucocorticoids (prednisolone) began to be taken only before surgery.
In mid-November, an operation was performed - Colectomy. Abdominal-anal resection of the rectum. During the intervention, clear signs of an inflammatory process were found throughout the entire colon and 50 cm of the terminal ileum. In the mesentery adjacent to the ileum there are a large number of large lymph nodes and massive compactions that deform this segment of the intestine.
The ileocecal section is mobilized, the cecum is opened, its mucous membrane is sharply hyperemic, erosions, ulcerations, pseudopolyps are visible. The ICC is atonic, does not close, is cicatricially changed, does not function. Simultaneously with the colectomy, about 70-75 cm of the ileum was removed.
A permanent Brooke ileostomy was formed in the groin area on the right.
An examination of the abdominal organs revealed a large gallbladder that emptied poorly on palpation, but without external signs of inflammation. During its puncture, about 90 ml of bile was removed, in the last portion - white inclusions. There are no stones. The clinical diagnosis of the disease was confirmed histologically (ulcerative-necrotic changes in the mucous membrane, hemorrhages in it and growths like a glandular polyp).
The postoperative period was difficult, but without serious complications. She was discharged three weeks after surgery under the supervision of a surgeon and gastroenterologist at her place of residence. Periodically consults by telephone. Two months after the operation, body weight increased by 5 kg. Ileostomy. functions normally (the volume of chyme has decreased).
From the analysis of the presented Case History, it is clear that the choice of surgery in this situation was predetermined: it was impossible to save the ICC and a significant segment of the ileum, and due to the serious condition of the patient, it was decided to refrain from inversion of the terminal ileum and cholecystectomy. All this was the result of long-term (not fully) conservative treatment and a belated decision on the need for surgical treatment.
Different assessments of the clinical outcomes of extensive resections of the colon are also explained by the fact that when these operations are performed, the size of the simultaneously removed portion of the terminal ileum is not the same. This explains the desire of surgeons for its minimal resection. Thus, according to various authors, during colectomy for colon polyposis and ulcerative colitis, it is recommended to remove no more than 5-7 cm of the ileum (Brusilovsky M.I., 1977), 4-5 cm (Vasiliev A.A., 1967) , 2-4 cm (Fedorov V.D., Nikitin A.M., 1985), 1-2 cm (Mikhailyani G.S., 1994) Some researchers attach crucial importance to preserving several centimeters of the ileum in front of the ICC, believing that this department is like a border post, the purpose of which is to ensure the efficiency of hydrolysis and absorption of nutrients in the upper and lower areas of the intestine. If during surgical interventions more than 20 cm of the final section of the ileum is removed, this causes severe functional disorders of the gastrointestinal tract and other organs and systems.
The surgical interventions we offer are precisely aimed at preventing these possible complications.
Literature 1. Baltaitis Yu.V. Extensive resection of the colon. Kyiv: Health, 1990 2. Brusilovsky M.I. Consequences of colectomy. - Chisinau: Shtiintsa, 1977. 3. Vasiliev A.A. Clinic and surgical treatment of nonspecific ulcerative colitis. M.: Medicine, 1967. 4. Velichenko V.M. Replacement of defects of the colon and rectum with ileograft. Minsk: Belarus, 1967. 5. Vitsyn B.A., Blagitko E.M., Nimaev Yu.Ts. Long-term results of resection of the ileocecal intestine // Vesti, surgeon. them. Grekova, 1977, 12, 31-34 6. Vorobyov G.I., Mikhailova T.L. and others. Experience of the State Scientific Center of Coloproctology in the surgical treatment of nonspecific ulcerative colitis // Russian. magazine gastroznterol., hepatol., coloproctol., 1999a. 8, 3, 47-55. 7. Vorobyov G.I., Mikhailova T.L. and others. The choice of surgical tactics for complications of nonspecific ulcerative colitis // Relevant. problem coloproctol. IV All-Russian conf. with international participation. Irkutsk, 1999 b, 323-325. 8. Vorobyov G.I. Resection of the ileocecal intestine // Clinical operative coloproctology / Ed. acad. RAMS V D. Fedorova, corresponding member. RAMS G.I. Vorobyova and prof. VL. Rivkina. M., 1994, 113-114. 9. Jackson I.M. On the physiology of the ileocecal region. Message 1 Reflex influences from the ileocecal region of the intestine to the pyloric part of the stomach // Bulletin. exp. biol., 1949, 27, 2, 81-84. 10. Dyskin E.L. Short-term and long-term results, resection of the ileocecal intestine // Vesti, surgeon. them. Grekova, 1960, 7, 73-81. 11. Zhukov B.N., Isaev V.R., Katorkin E.N. Colon polyposis and metabolic disorders. Samara, 1993. 12. Isaev V.R., Zhukov B.N., Savinkov A.I. Surgical treatment of postcolectomy and postcoloproctectomy syndrome // Problems of coloproctology. Issue 16. / Ed. Corresponding member RAMS prof. G.I. Vorobyova, dmm. I.L. Khalifa. M., 1998, 380-388. 13. Lebedev N.N. Biorhythms of the digestive system. M.: Medicine, 1987. 14. Melman E.P. Functional morphology of the innervation of the digestive organs. M.: Medicine, 1970. 15. Melnikov P.A., Pravosudov I.V., Gulyaev A.V., Kovalev V.K. and others. Rational surgical tactics for diffuse polyposis and primary multiple cancer against the background of colon polyps // Vesti, surgeon. them. Grekova, 1996, 1, 34-37. 16. Mikhailyants G.S. Colectomy // Clinical operative coloproctology. Guide for doctors / Ed. Academician of the Russian Academy of Medical Sciences VD. Fedorova, corresponding member. RAMS G.I. Vorobyov and Professor VL. Rivkina. M., 1994, 135-139. 17. Oleynikov P.N. 30 years of experience in the treatment of nonspecific ulcerative colitis // Current. problem coloproctol. IV All-Russian conf. with international participation. Irkutsk, 1999, 336-339. 18. Savchenko N.F., Kuzmin S.N., Rebrova E.L. and others. Experience in the treatment of severe forms of ulcerative colitis // Actual. problem coloproctol. IV All-Russian conf. with international participation. Irkutsk, 1999, 316-318. 19. Saks F.F., Aksenenko A.V., Usynin A.Yu. Neuromuscular apparatus of the ileocecal part of the human intestine // Sphincters of digestion. tract / Ed. Professor V.F. Baitinger. Tomsk, 1994, 152-162. 20. Siparov I.N., Lud N.G. Clinic and treatment of short bowel syndrome. Minsk: Belarus, 1988. 21. Fedorov V.D., Nikitin A.M. Diffuse polyposis of the colon. M.: Medicine, 1991. 22. Frolkis A.V. Functional diseases of the gastrointestinal tract. L.: Medicine, 1991. 23. Booth CC, Evans KT et al. Intestinal hypertrophy following partial resection of the bow smallel in the rat//Br.J. Surg., 1959, 46, 403-410. 24. Degen LP, von Flue MO, Collet A., Hamel Ch. et al. Ileocecal segment transposition does not alter whole gut transit in humans // Ann. Surg., 1997, 226, 6, 746-752. 25. Faussone PMS, Ibba MI, Manneschi L. The caecolonic junction in humans has a sphincteric anatomy and function // Gut, 1995, 37, 493-498. 26. Von Flue M., Harder F. New technique for pouch-anal reconstruction after total mesorectal exicision//Dis. colon. Rectum, 1994,37, 1160-1162. 27. Von Flue M.0., Degen L.P. et al. The ileocecal reservoir for rectal replacement in complicated radiation proctitis//Am.J. Surg., 1996, 172, 4, 335-340. 28. Johansson H., Nylander G. Ileocolic transit in rats subject to ileocecal resection//Acta chir. scand., 1969, 135, 455-458. 29. Kieninger G., Koslowski L., Durst], et al. Clinical experience with a new method of gastric replacement following total gastrectomy // World J. Surg., 1979, 3, 6, 737-743. 30. Kruis W., Phillips SF, Zinsmeister A. Flow across the canine ileocolonic junction: role of the ileocolonic sphincter// Am.J. Physiol., 1987, 252, G13-G18. 31. Lundqvist H., Jung V., Gustavsson S. et al. Analyzes of small bowel propulsion, ileocecal passage and serum gastrin after truncal vagotomy // Acta chir. scand., 1975. 141, 298-303. 32. Nasmyth DG, Willians NS Pressure characteristics of the human ileocecal region - A Key to its function // Gastroenterology, 1985, 89, 345-351. 33. Neal DE, Williams NS et al. The effect of resection of the distal ileum on gastric emptying, small bowel transit and absorption after proctocolectomy // Br.J. Surg, 1984, 71, 66-670, 34. Neri M, Phillips SF et al. Canine ileocolonic sphincter flow, transit, and motility before and after sphincterotomy//Am.J. Physiol., 1991, 260, G284-G289. 35. Phillips SF, Qyigley EMM et al. Motility of the ileocolonic junction // Gut, 1988, 29, 390-406. 36. Schrader S.-P. Tierversuche zur Aniage ernes Ersatzmagens nach Gastrectomie. Tubingen, Habilitationsschrift, 1972 (cited no: G. Kieninger et al., 1979). 37. Soper NJ, Chapman NJ, Kelly KA. et al. The “ileal brake” after ileal pouch-anal anastomosis // Gastroenterology, 1990.98, 111-116.
Isaev V.R., Zhukov B.N., Savinkov A.I., Lysoe N.A. Samara State Medical University, Department of Hospital Surgery, Samara
Symptoms of the disease
Insufficiency of the Bauginian valve is a little-studied disease, as it is characterized by rather nonspecific symptoms:
- flatulence (excessive accumulation of gases),
- bowel dysfunction: diarrhea and constipation;
- seething in the abdomen, which is especially well heard when pressing on the abdomen, namely in the area of the right hypochondrium;
- bad breath, presence of bitterness in the mouth;
- heartburn, nausea, belching;
- pain in the right side. The pain is mild, intermittent, and often occurs some time after eating;
- dizziness;
- cardiopalmus;
- increased fatigue;
- weight loss.
In most cases, insufficiency of the bauhinium valve is detected completely by accident (during an examination of the body or during screening) and can be mistaken for another disease.
Features of treatment
After diagnosing insufficiency of the bauhinium valve, the doctor prescribes comprehensive treatment. Its features depend on the degree of violations that occurred and the reasons that caused the process. The patient must switch to the correct daily routine and diet.
Correction of ileocecal valve insufficiency can be performed surgically or using drug therapy.
We recommend finding out whether you can eat bananas with chronic pancreatitis.
Read: what is melena stool and why does it occur.
Find out how phlebectasia of the esophagus is treated.
What does the new way of life involve?
The doctor’s first requirement is that the patient immediately switch to a new diet, which should not include heavy, “junk” food. It includes animal fats, salted, smoked, fried, spicy foods, and any type of alcohol. Coffee, soda, and strong tea are prohibited. Diet is important. You should eat 4 or more times a day, the average serving weight should not exceed 300 grams.
It is recommended to exclude stressful situations from the patient’s life and carry out psychotherapeutic measures to normalize his condition.
To restore the health of patients diagnosed with “bauhinium valve insufficiency,” treatment with folk remedies is possible. The use of any of them is permitted only after consultation with a doctor.
Use of medications
To eliminate dysfunction of the bauhinium valve, a specialist may prescribe the following drugs:
- magnesium orotate, its composition combines the components - magnesium and orotic acid (non-steroidal anabolic), they are necessary to restore the valve to lost muscle qualities;
- drugs to stimulate intestinal motility, increase the tone of its muscles (Coordinax, Proserin);
- probiotics for restoration and regulation of microflora;
- antiemetics (Cerucal);
- vitamins (C, group B).
Bauhin's valve: diagnostic methods
You can see the Bauhinian valve and accurately determine its functionality by performing a colonoscopy, which allows you to examine in detail the ileum, the mucous membrane of the small intestine, and also identify inflammatory processes present in the body.
The pathology of the ileocecal valve can be diagnosed using several methods, one of which is irrigoscopy, which involves injecting a barium-containing contrast agent into the rectum and then taking x-rays. The manipulations performed allow us to see the distribution of the contrast agent and make a presumptive diagnosis based on what we see, which can be confirmed by endoscopic examination.
A fairly effective and expensive diagnostic method is capsule endoscopy, during which the patient is required to swallow a miniature video camera equipped with a power source. To date, this method is the most reliable and the only one that allows you to completely examine the inside of the small intestine.
Location and structure
The Bauhinian valve is located between the ileum and large intestine. In this case, the upper part of the valve faces the cavity of the ascending colon, and the lower part faces the cavity of the cecum. The ileocecal valve is formed by the sphincter - a muscle ring on which there is a slight thickening. The formation protruding into the intestinal cavity forms a dome-shaped nipple, which, when the muscles contract, covers the intestinal cavity.
The total width of the valve muscles is approximately 4 cm. The opening of the ileocecal valve looks like a horizontal slit or oval opening. Its total length is on average 25-27 mm. On the side of the ileum there is a special area - the upper lip. It is a free medial wall of the ileum overhanging the valve fissure. The lower lip is formed by the medial portion of the ileum, which is localized under the fissure.
Features of the anatomical structure of the area of the transition of the small intestine to the small intestine can be variable. Thus, in some people, slight intussusception (pressure) of the ileum into the cavity of the cecum is possible (no more than 5 mm). The wall of the organ in the area of invagination is large, so this area is called the ileocecal eminence.
Be sure to read:
Preparation and performance of anorectal manometry
Insufficiency of the Bauhinium valve: treatment
Identified pathology of the ileocecal valve is treated exclusively in a hospital setting and only using an integrated approach. If the development of inflammation occurs due to the presence of an infection in the body, doctors prescribe antiviral drugs and antibacterial agents. If the disease is anatomical, treatment is carried out not only with drugs (containing magnesium), but also with surgical intervention, which consists of narrowing the bauhinium valve. Such manipulations can reduce the volume of contents returning back to the small intestine.
What diagnostic methods are needed to confirm the disease?
If there is a suspicion of dysfunction of the ileocecal valve, the patient may receive a referral for instrumental diagnostics. He is invited to undergo tests (their choice is determined by the availability of certain equipment in the medical institution, as well as the patient’s ability to carry out diagnostics for a fee):
- colonoscopy (total);
- endoscopic examination (capsule);
- irrigoscopy (involves administering contrast through the rectum, then using a radiograph).
The key to health is the correct daily routine
Therapy is aimed both at eliminating symptoms and at relieving inflammation and swelling. The problem of the pathological condition of the ileocecal valve is almost always solved by normalizing lifestyle, provided that the causes of the disease are due to functional reasons. Therefore, first of all, you need to establish a daily routine and normalize your own diet. You need to eat in small portions, about 6-7 times a day. This will normalize the functioning of the valve system of the gastrointestinal tract and regulate the mechanism of unilateral movement of food masses. The menu should be diversified with mechanically gentle food: slimy soups, steamed fish and meat cutlets, meatballs. It is recommended to consume fruits in the form of purees, juices, and compotes. Baked apples are very useful. It is important to give up fried and spicy foods, black bread, beets, cabbage, limit coffee consumption, and also give up bad habits: alcohol and smoking. Patients are under medical supervision for six months.
Since the Bauhinian valve can often become inflamed due to psychosomatic disturbances, it is necessary to prevent stress factors from entering your life. For help in this matter, you can contact a psychologist or psychotherapist.
Its pathology in each specific case requires an individual therapeutic approach, which is determined only by the attending physician, taking into account the diagnosis and assessment of risk factors.
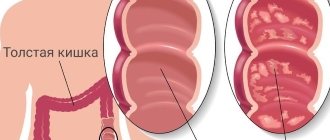
Assessment of the condition of the mucous membrane.
The description of the unchanged mucous membrane should be made taking into account the endoscopic signs given below.
- Color: depending on the light characteristics of the light source, the mucous membrane can be either pale yellow, white with a pearly tint, or slightly pink. Changes in the color of the mucous membrane occur due to its infiltration or hyperemia.
- Shine: normal smooth mucous membrane reflects light well and shines. This shine is due to light mucus, an even layer covering the intestinal wall. Due to the fine wavy circular striations of the colon mucosa, the absence of this lubricant makes the mucous membrane dull.
- Character of the surface. Normally, the surface is slightly striated but smooth. The slightest tubercles, ulcerations, and bulges indicate pathological changes.
- Vascular drawing. When the colon is inflated, a vascular pattern formed by submucosal arterial branches is clearly visible (the accompanying veins are not visible, since they are compressed by the injected air). Changes in the vascular pattern can be varied. It can be intensified and then small branches of the arteries become visible (it must be remembered that similar changes can be caused by overstretching). The absence of a submucosal vascular pattern indicates thickening of the mucous membrane or submucosal edema. Atrophic changes are characterized by rearrangement of the vascular pattern like angiomas, asterisks or choroid plexuses, and the severity of the venous pattern.
- Overlays As a rule, mucus can accumulate on the normal mucous membrane of the colon, either in the form of lakes or in the form of light lumps. The compaction of these deposits, the admixture of pus, fibrin, and necrotic masses indicate pathological changes in the intestinal mucosa.
An important feature of a normal mucous membrane is its good mobility relative to the submucosal layer.