- What causes appendicitis?
- How to prevent complications after appendicitis?
- Treatment of appendicitis Sutures after appendicitis
- What depends on the professionalism of the doctor?
- Diet after appendicitis
Appendicitis is a fairly common disease. If detected in time, it is quickly cured, but can only be eliminated surgically. At the same time, surgery to remove appendicitis is assessed by surgeons as the easiest. The development of appendicitis is justified by certain factors; it does not arise out of the blue.
| Prevention of appendicitis is not the least important in creating a healthy lifestyle. When the disease cannot be avoided, it makes sense to adjust your diet and daily routine. Rehabilitation after appendicitis does not require many restrictions, but in order to feel excellent, you must listen to your doctor’s recommendations. |
What causes appendicitis?
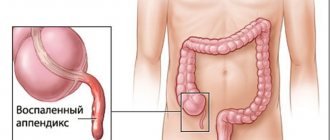
Appendicitis is an inflammation of the vermiform appendix of the cecum, the appendix. The function of the appendix in the body has not been fully established. It is rather a vestigial organ. It is assumed that in the course of human evolution it has lost its main digestive function and today plays a secondary role:
- contains a large number of lymphoid formations, which means it partially provides immunity;
- produces amylase and lipase, which means it performs a secretory function;
- produces hormones that provide peristalsis, and therefore is akin to hormonal glands.
The causes of appendicitis are described by several theories:
- the mechanical one states that the reason for the development of appendicitis is obstruction of the lumen of the appendix with fecal stones or lymphoid follicles against the background of activation of the intestinal flora; as a result, mucus accumulates in the lumen, microorganisms multiply, the mucous membrane of the appendix becomes inflamed, then vascular thrombosis and necrosis of the walls of the appendix directly occur;
- the infectious theory is based on the fact that inflammation of the appendix is caused by an aggressive effect on the appendix of infectious agents localized here; usually this is typhoid fever, yersiniosis, tuberculosis, parasitic infections, amebiasis, but specific flora has not yet been identified;
- the vascular theory explains the development of appendicitis by a disorder of the blood supply to this part of the digestive tract, which is possible, for example, against the background of systemic vasculitis;
- endocrine The basis for the occurrence of appendicitis is the effect of serotonin, a hormone produced by multiple cells of the diffuse endocrine system located in the appendix and acting as a mediator of inflammation.
Appendicitis often develops against the background of other disorders of the gastrointestinal tract. A high risk of appendicitis is assessed for those individuals who are diagnosed with:
- chronic forms: colitis,
- cholecystitis,
- enteritis,
- adnexitis
Appendicitis most often develops between the ages of 20 and 40; Women suffer from it more often than men. Appendicitis ranks first among surgical diseases of the abdominal organs.
Prevention of appendicitis consists of eliminating negative factors, treating chronic diseases of the abdominal organs, eliminating constipation and maintaining a healthy lifestyle. The diet should include a sufficient amount of plant fiber, since it is this that stimulates intestinal motility, has a laxative effect and reduces the passage time of intestinal contents.
How to prevent complications after appendicitis?
Inflammation of the appendix, if not diagnosed and eliminated in time, can result in serious pathologies. The latter include:
- appendiceal infiltrate - a conglomerate of inflamed tissues of the appendix and adjacent organs (omentum, small intestine, cecum) that develops 2-4 days after acute appendicitis;
- abdominal abscess and periappendiceal abscess - can develop around the appendix and in other places in the abdominal cavity due to sedimentation of an infected effusion, intra-abdominal hematomas or poor-quality sutures of the appendix stump;
- peritonitis (inflammation of the peritoneum);
- phlegmon of the retroperitoneal space is an acute purulent-inflammatory process that develops in the retroperitoneal tissue, not delimited from healthy tissues;
- thrombophlebitis of the pelvic veins and pylephlebitis (septic thrombophlebitis of the portal vein and its branches, usually developing after appendectomy);
- sepsis (blood poisoning).
The cause of complications after appendicitis lies in unprofessional treatment or too late contact with a doctor. Under no circumstances should the symptoms of acute appendicitis be ignored and expect that everything will go away on its own. Tangible discomfort in the lower right side, combined with bowel movements, vomiting and fever, should be a reason for immediate contact with a professional physician.
If appendicitis develops, it is strictly forbidden to take laxatives and painkillers, or apply heat to the painful area. In the prehospital period, the patient requires rest and bed rest; on the contrary, cold can be applied to the side. Confirmation of suspicion of appendicitis is an indication for surgical intervention; conservative treatment methods do not demonstrate success.
Surgical intervention performed on the first day of appendicitis development is easy to perform and complications are unlikely. The prognosis is assessed favorably. Usually, on the second day after surgery, the patient can turn over in bed, sit down, and get up and walk on the 3-4th day.
In the next few weeks, the patient must adhere to a gentle regimen and reduced physical activity, otherwise the risk of improper healing of the suture after appendicitis , the development of adhesive disease, and an inguinal hernia increases. The likelihood of this is explained by the uneven fusion of muscle tissue, when the mesentery or intestinal loops can protrude through the unfused areas, and this will prevent the final fusion of the muscles. This usually happens in the background:
- improper nutrition of the patient in the postoperative period;
- ignoring the necessary wearing of a bandage;
- weakness of the muscular frame of the anterior abdominal wall;
- unacceptable physical activity and heavy lifting;
- inflammatory internal processes.
Forecast
A timely diagnosis of appendix perforation will save your life.
Fatal cases of appendicitis depend on the delay in diagnosis (perforation of the appendix) and the age of the patient. A rather interesting publication was presented by the English Royal College of Surgery, according to which the mortality rate was 0.24, and the incidence of various complications was 7.7 in 6596 patients who underwent open appendectomy from 1990 to 1992.
The prognosis of the development of tubal infertility and its frequency after appendectomy was also additionally considered. Even though reports indicate that after perforated appendicitis the increased risk of infertility is 4.8 for nulliparous patients and 3.2 for multiple parous patients, a modern historical cohort study has shown that there are no consequences for fertility.
This latter study provides a counterargument to the view that prefers performing an unnecessary appendectomy rather than risking delayed surgery with an increased risk of perforation during acute appendicitis. It has previously been noted that careful observation of the patient in the hospital and his examination is in no way associated with an increased risk of perforation, since both early and late complications when using traditional intervention are in the range of 13% to 17%.
Treatment of appendicitis
Today, medicine does not offer any other methods of treating appendicitis other than emergency surgery. Although the very act of surgery can be a major concern for many patients, there are minimal risks in this treatment strategy. If the operation is performed efficiently and immediately, then already on the second day the patient begins to recover progressively.
Access to the appendix is carried out using the McBurney method (or, as it is called in the domestic literature, Volkovich-Dyakonov); removal of the appendix can be typical or retrograde:
- the typical one is used when it is possible to remove the appendix through surgical dissection - the mesentery is ligated and then cut off, the stump is placed in the dome of the cecum;
- retrograde is appropriate if it is impossible to pass the appendix through the surgical wound, for example, in the presence of adhesions or an atypical location of the appendix - first, the appendix is cut off from the dome of the cecum, then the stump is placed in the dome, and only after that the appendix is isolated and the mesentery is ligated.
As a result of accessing the appendix using the McBurney method, a small, even scar remains, which is very undesirable for many patients. Advances in modern medicine offer minimally invasive surgical interventions to eliminate appendicitis. First of all, this is a laparoscopic method - through small punctures of the abdominal wall (usually three) with special instruments. Another minimally invasive progressive method of removing the appendix is transluminal - flexible instruments inserted into the lumen of the genital organ and through an incision in the wall of the internal organ (in the wall of the stomach or vagina). Transluminal intervention is characterized by a complete absence of visually noticeable defects and a reduction in postoperative rehabilitation time.
Stitches after appendicitis
With the classic version of surgery, a small (on average three-centimeter) suture remains in the lower side of the abdomen. The application and resorption of sutures after appendicitis requires professionalism from the doctor and responsibility from the patient in following his recommendations.
In the absence of complications after appendicitis, external sutures are removed on days 10-12, and internal sutures are absorbed within two months (performed with catgut threads). These are the necessary time frames for restoring a strong muscle frame, and the skin regenerates even faster. On average, about 6 weeks (at least) the patient will be recommended a special gentle regimen.
What depends on the professionalism of the doctor?
Cooperation with a qualified physician is important even at the stage of diagnosing appendicitis. In this case, it is important to thoroughly study the history of the disease, evaluate the existing symptoms and not ignore or ignore signs indicating the severity of the process.
If the diagnosis is confirmed, surgery is performed almost on the same day. Appendicitis does not relapse, it cannot be repeated, but its insidiousness lies in the likelihood of adhesive disease. It develops with infection of the abdominal cavity, disproportionate physical activity and excessive mobility in the postoperative period, against the background of fermentation processes due to non-compliance with the diet.
Possibly suppuration of the sutures. It occurs due to the negligence of medical staff and insufficient sanitary treatment of instruments. Another reason for suppuration of sutures is improper treatment of the wound surface and nosocomial infection. The risk of overstrain of the abdominal wall depends on the patient’s carelessness, which is often aggravated by weak immune defense.
The prevalence of postoperative complications in appendicitis has recently tended to decrease due to the fact that patients turn to doctors at an early stage of appendicitis, and modern medical advances make minimally invasive interventions possible.
Laparoscopic appendectomy
Recently, with the development of technical capabilities in medicine, minimally invasive techniques, also used in the surgery of abdominal diseases, are becoming increasingly popular. Laparoscopic appendectomy is a worthy alternative to classical surgery, but for a number of reasons it cannot be performed on every patient.
Laparoscopic removal of the appendix is considered a more gentle method of treatment, which has a number of advantages:
- Low morbidity compared to abdominal surgery;
- Possibility of local anesthesia in most patients;
- Shorter recovery period;
- The best result for severe diseases of internal organs, diabetes, obesity, etc.;
- Good cosmetic effect;
- Minimum complications.
However, laparoscopic appendectomy also has some disadvantages. For example, an operation requires the availability of appropriate expensive equipment and a trained surgeon at any time of the day, because the patient can be taken to the hospital at night. Laparoscopy does not allow a detailed examination of the entire volume of the abdominal cavity, adequate sanitation and removal of exudate in common forms of the inflammatory process. In severe cases, with peritonitis, it is impractical and even dangerous.
Through many years of discussions, doctors determined the indications and contraindications for laparoscopic removal of the appendix.
The following are considered indications:
- Doubts about the diagnosis requiring laparoscopy for diagnostic purposes. For example, in a woman with pain in the right iliac fossa, after several hours of observation, the diagnosis of appendicitis cannot be confirmed. The surgeon goes for laparoscopy and discovers inflammation of the uterine appendages, which can spread to the appendix, or it is already inflamed, in which case it is quite logical to remove it laparoscopically. The child may be diagnosed with catarrhal appendicitis, and the appendix is removed during laparoscopy. These operations are performed in the absence of contraindications (purulent process, peritonitis), in which, after laparoscopy, open abdominal surgery is performed.
- Severe concomitant pathology (severe obesity, diabetes mellitus, heart failure), in which major surgical trauma is undesirable, the risk of infectious complications is high, and abdominal surgery is inevitably accompanied by large incisions (in obese patients).
- The patient’s desire to perform the operation laparoscopically (of course, if this does not conflict with safety).
- Laparoscopic surgery for gynecological pathology, when in case of adhesions, purulent inflammation of the pelvic organs, leaving even an unchanged appendix is impractical and is fraught with secondary appendicitis.
If there are no risks, the patient’s condition is stable, and the inflammation has not spread beyond the appendix, then laparoscopic appendectomy can be considered the method of choice.
Contraindications to minimally invasive treatment:
- More than a day from the onset of the disease, when the likelihood of complications is high (perforation of the appendix, abscess).
- Peritonitis and the transition of inflammation to the cecum.
- Contraindications for a number of other diseases - myocardial infarction, decompensated heart failure, bronchopulmonary pathology, etc.
In order for laparoscopic appendectomy to be a safe and effective treatment procedure, the surgeon will always weigh the pros and cons, and in the absence of contraindications to the procedure, it will be a low-traumatic treatment method with minimal risk of complications and a short postoperative period.
The course of laparoscopic appendectomy includes:
A small incision is made in the umbilical area through which carbon dioxide is injected into the abdomen for a good view. The laparoscope is also inserted through the same hole. The surgeon examines the abdomen from the inside, and if doubts arise about the safety of further manipulations, he proceeds to open surgery.- Instruments are inserted through incisions in the pubic area and right hypochondrium, with the help of which the appendix is captured, the vessels are ligated, the mesentery is cut off, then the appendix is cut and removed from the abdomen.
- Inspection and sanitation of the abdominal cavity, drainage if necessary, suturing the instrument insertion sites.
Laparoscopic surgery for appendicitis lasts up to one and a half hours, and the postoperative period takes only 3-4 days. Scars after such an intervention are barely noticeable, and after some time has passed for final healing, they can be difficult to find.
The suture after open surgery is removed after 7-10 days. A scar will remain at the site of the incision, which will thicken and fade over time. The scar formation process takes several weeks.
The cosmetic effect is largely determined by the efforts and skill of the surgeon. If the doctor treats the wound suturing conscientiously, the scar will be almost invisible. If complications develop, if it is necessary to increase the length of the incision, the surgeon will be forced to sacrifice the cosmetic side of the issue in favor of preserving the health and life of the patient.
What measures are recommended after appendicitis?
After appendicitis, the patient must adhere to relatively simple and feasible restrictions for 1-2 months. They are quite simple to implement, especially considering that ignoring them is fraught with quite unpleasant and undesirable consequences.
Diet after appendicitis
After appendicitis, independent consumption of food is allowed from the third day after surgery, but food during this period should be ground and mushy. Milk and milk jelly, liquid porridge (preferably with water), chicken and vegetable broth, and vegetable purees are allowed. Dietary nutrition begins on the sixth day. Some dietary features are prescribed to the patient in the first 2-3 months after surgery. Diet affects the composition of the intestinal microflora and the activity of its functions. The following principles must be followed:
- small and frequent meals; simultaneous consumption of large portions of food is contraindicated;
- food should not be hot or cold, but only slightly warmed up;
- nutritious nutrition that provides the body with the entire spectrum of nutrients, vitamins and minerals, since stimulation and strengthening of the immune system is required during the recovery period;
- exclusion of products that promote fermentation and gas formation in the digestive tract; The diet should not contain legumes, heavy animal fats, any varieties of cabbage, smoked meats, marinades and pickles, and the consumption of alcoholic and carbonated drinks is not recommended.
While the diet should be complete, with sufficient protein content and the exclusion of only heavy fats, after appendicitis the patient is strongly advised to monitor his weight. Since physical activity is significantly minimized in the postoperative period, it is easy to gain excess weight, which is extremely undesirable.
To restore normal microflora, the body benefits from dairy and fermented milk products and plenty of drinking water. Meat and fish should not be consumed in the first weeks after appendicitis, but broths and pureed minced meat/fish are acceptable. If consuming fiber serves as an excellent prevention of appendicitis, then in the first week after surgery it is, on the contrary, undesirable. It is better to give up bread and baked goods; an excellent alternative can be bread, which contains a minimum of fiber and carbohydrates. Vegetables (carrots, beets) and bananas are perceived favorably by the body; it is better to avoid citrus fruits. At the same time, for immunization the body needs vitamin C, which can be obtained from other foods or consumed in tablet form, as well as other vitamins and vitamin-mineral complexes.
The end of the diet after appendicitis should not be abrupt. It is recommended to gradually expand the diet. Under no circumstances should you suddenly lash out at foods that were previously excluded from your diet. In general, the postoperative diet is not strict, and therefore it will be useful to follow the rules that have already been familiar for several months in the future. This will only benefit the body.
Physical activity after appendicitis
The patient is allowed minimal physical mobility the next day after surgery, but it is recommended to get out of bed only on the third day.
Over the next 6 weeks, muscle fusion occurs, against which the risk of adhesions and even hernias remains. Heavy lifting and active physical activity are strictly prohibited. At the same time, it is noted that daily walking at a leisurely pace of 2-3 kilometers in the afternoon helps prevent adhesions. Therapeutic gymnastics is prescribed. It is noteworthy that the best restoration of muscle tissue occurs in those individuals who, before developing appendicitis, led an active lifestyle and kept their body in good shape.
As with diet, the increase in physical activity after appendicitis should not be sudden. After a few months, you can return to moderate exercise, gradually supplementing therapeutic exercises with general exercises.
Consequences of appendix removal for the body
As already noted, the appendix is considered an atavism. For modern humans, this is a rudimentary organ, the absence of which does not significantly affect the functioning of the body and the digestive system in particular. At the same time, the appendix produces some secretions and hormones, and lymphoid formations are located here.
Removal of the appendix means a temporary weakening of the immune system both due to the elimination of lymphoid cells and due to external intervention, the risk of infection entering the body. This risk can be overcome through artificial stimulation of the immune system, good nutrition, minimizing stress and active physical activity, and creating generally favorable conditions for rehabilitation.
Indications and preparation for surgery
Appendectomy is one of the interventions that in most cases is performed as an emergency. Indication: acute appendicitis. A planned operation to remove the appendix is performed with appendiceal infiltrate after the inflammatory process has subsided, approximately 2-3 months from the onset of the disease. In case of increasing symptoms of intoxication, rupture of an abscess with peritonitis, the patient needs emergency surgical treatment.
There are no contraindications to appendectomy, except in cases of the patient's agonal state, when the operation is no longer advisable. If doctors have adopted a wait-and-see approach due to appendiceal infiltration, then severe decompensated diseases of the internal organs may be contraindications to surgery, but during conservative treatment the patient’s condition can be stabilized to such an extent that he can undergo the intervention.
The operation usually lasts about an hour, both general anesthesia and local anesthesia are possible. The choice of pain relief is determined by the patient’s condition, his age, and concomitant pathology. Thus, in children, people with excess body weight, which involves greater trauma when entering the abdominal cavity, with nervous overexcitation and mental illness, general anesthesia is preferable, and in thin young people, in some cases, it is possible to remove the appendix with local anesthesia. Pregnant women, due to the negative impact of general anesthesia on the fetus, are also operated on under local anesthesia.
The urgency of the intervention does not require sufficient time to prepare the patient, so the necessary minimum examinations are usually performed (general blood test, urine test, coagulogram, consultations with specialists, ultrasound, x-rays). To exclude acute pathology of the uterine appendages, women need to be examined by a gynecologist, possibly with an ultrasound examination. If there is a high risk of thrombosis of the veins of the extremities, the latter are bandaged before surgery with elastic bandages.
Before the operation, the bladder is catheterized, the contents are removed from the stomach if the patient ate later than 6 hours before the operation, and an enema is indicated for constipation. The preparatory stage should last no more than two hours.
When the diagnosis is beyond doubt, the patient is taken to the operating room, anesthesia is administered, and the surgical field is prepared (hair shaving, iodine treatment).