Symptoms of GERD: treatment
Treatment for GERD consists of medications or surgery.
Medicines
The NIDDK lists the following treatment options for GERD:
- Antacids : Doctors may recommend over-the-counter antacids to relieve mild symptoms of GERD. You should not take these medications for severe symptoms or use them for daily use without consulting your doctor.
- H2 blockers : These drugs reduce acid production in the stomach. They are available over the counter or with a prescription.
- Proton pump inhibitors (PPIs) : Doctors may recommend PPIs for long-term treatment of GERD. These drugs reduce stomach acid production more than H2 blockers.
Operation
Surgery is an option if lifestyle changes and medications do not relieve GERD symptoms. The NIDDK states that doctors may recommend one of the following procedures:
- Fundoplication : In most cases, fundoplication produces long-term improvement, which is why it is the most common type of surgery for GERD. It involves suturing the top of the stomach to the end of the esophagus. This increases pressure on the lower esophageal sphincter and reduces acid reflux.
- Bariatric surgery: An example of this procedure, also known as weight loss surgery, is gastric bypass surgery. Doctors may recommend this type of weight loss surgery for those with GERD and obesity.
- Endoscopy : This procedure is only suitable for a small number of cases. In this process, the doctor inserts a tube with an attached camera into the esophagus and then administers treatment.
Sometimes it is enough to change the diet and adjust the child’s lifestyle.
Perhaps this will be enough - the complaints will disappear or significantly decrease.
What can you recommend?
Avoid overeating and reduce portion sizes - this way they will not cause stomach fullness and increased intragastric pressure.
Limit fatty and fried foods - they slow down the natural passage of food
from stomach to intestines
Avoiding foods that relax the valve between the esophagus and stomach is the main defense against reflux.
Such products include chocolate, caffeine-containing drinks, mint, citrus fruits and tomatoes (also juices from the latter).
Remember that passive smoking increases reflux.
Tight clothing and belts that compress the abdominal area increase intra-abdominal pressure and can provoke reflux
For overweight children, set a goal to reduce body weight.
If reflux is provoked by certain physical activity - somersaults, bending forward, etc. - avoid these situations if possible.
Although I don’t really understand how to explain this to an active and active baby.
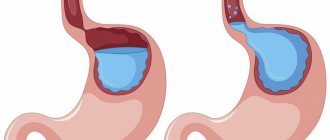
There are children (and adults, of course) whose complaints appear in a horizontal position. This is when gravity doesn't help keep food in the stomach and reflux worsens.
I recommend that such children do not lie down immediately after eating.
Implementing this advice in a kindergarten setting is not easy: it has long been accepted that soon after lunch (the largest meal of the day), children are put to sleep.
If possible, such children should have dinner 2.5-3 hours before bedtime.
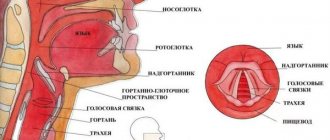
I also give similar advice to children with laryngopharyngeal reflux.
Many experts on this unusual variant of reflux, when aggressive stomach contents are refluxed into the respiratory tract, believe that it is at night that everything happens.
Perhaps this is why laryngopharyngeal reflux is often not accompanied by daytime complaints of heartburn, belching food, and so on.
A good option is also to change the horizontal position during sleep - you can put the baby with a slight tilt so that the head and throat are higher than the stomach.
Ways to create such a tilt have already been discussed, but new ways continue to appear - you can share your life hacks in the comments.
This way, it is possible to help some children with GERD without resorting to medication.
Risks
The NIDDK notes that the following factors may increase your chance of developing GERD:
- pregnancy
- overweight or obesity
- smoking, including passive smoking
- hiatal hernia
- certain medications such as: benzodiazepines, which are a class of sedatives
- calcium channel blockers, which are a class of drugs that lower blood pressure
Experience in the treatment of gastroesophageal reflux disease
Ensuring effective control of gastric secretion is one of the main conditions for successful treatment of so-called “acid-dependent” diseases of the upper gastrointestinal tract. In clinical and outpatient practice, currently, second-generation (ranitidine) and third-generation (famotidine) H2-receptor blockers of histamine are most often used to inhibit hydrochloric acid by parietal cells of the gastric mucosa, somewhat less frequently - proton pump inhibitors (omeprazole, rabeprazole), and for neutralization of hydrochloric acid already released into the stomach cavity - antacid drugs. Antacids are sometimes used in the treatment of patients suffering from so-called “acid-dependent” diseases, in combination with H2-blockers of histamine receptors; sometimes as on-demand therapy in combination with proton pump inhibitors. One or two chewed antacid tablets do not have a significant effect [10] on the pharmacokinetics and pharmacodynamics of famotidine used at a dose of 20 mg.
There are certain differences between these medications; we list the main ones: different mechanisms of action; speed of onset of therapeutic effect; duration of action; varying degrees of effectiveness of their therapeutic action depending on the time of taking the drug and eating; cost of medications [1]. The above factors are not always taken into account by doctors when treating patients.
In recent years, the literature has increasingly discussed the issues of pharmacoeconomic effectiveness of the use of various medications used according to one or another regimen in the treatment of “acid-dependent” diseases [2, 7]. The cost of examination and treatment of patients is especially important to consider in cases where patients, due to the characteristics of the disease, require long-term treatment [4, 6], for example, with gastroesophageal reflux disease (GERD). This is a very common disease, and the examination and treatment of such patients requires significant costs.
As is known, most patients with GERD do not have endoscopic signs of reflux esophagitis. However, as GERD progresses, pathological changes in the esophageal mucosa appear. The symptoms of this disease have the same impact on quality of life as the symptoms of other diseases, including coronary heart disease [5]. It has been observed [8] that GERD has a negative impact on quality of life, especially on pain scores, mental health and social function. Patients suffering from GERD are at high risk of developing Barrett's esophagus, and then adenocarcinoma of the esophagus. Therefore, at the very first clinical symptoms of GERD, especially when endoscopic signs of esophagitis occur, it is necessary to pay sufficient attention to timely examination and treatment of such patients.
Currently, patients with GERD are treated, in particular, with the drug famotidine (gastrosidine) in usual therapeutic dosages (20 mg or 40 mg per day). This drug has a number of advantages: ease of use (1-2 times a day), high efficiency in the treatment of “acid-dependent” diseases, including compared to antacid drugs [9], as well as greater safety compared to cimetidine. However, observations have shown [1] that in some cases, to increase the effectiveness of therapy, it is advisable to increase the daily dose of gastrosidine, which, according to some observations [1], reduces the likelihood of side effects compared to the use of histamine first H2 receptor blockers (cimetidine) in higher doses ) and second (ranitidine) generations. The advantage of famotidine [11] over cimetidine and ranitidine is its longer inhibitory effect on the secretion of hydrochloric acid by parietal cells of the gastric mucosa.
There are other advantages of histamine H2 receptor blockers (ranitidine or famotidine) over proton pump inhibitors; in particular, prescribing these drugs at night allows them to be used effectively in the treatment of patients due to the absence of the need to observe a certain “temporary” connection between the intake of these drugs and food. Prescribing some proton pump inhibitors at night does not allow them to be used to their full potential: the effectiveness of proton pump inhibitors is reduced, even if these drugs are taken by patients in the evening and an hour before meals. However, 24-hour pH monitoring carried out in patients treated with omez (20 mg) or famotidine (40 mg) indicates [3] that the duration of action of these drugs (10.5 hours and 9.4 hours, respectively) does not overlap the period of night secretion, and in the morning, a significant proportion of patients again experience “acidification” of the stomach. In this regard, it is necessary to take these drugs in the morning.
Of particular scientific and practical interest is the study of the effectiveness and safety of the use of famotidine and omeza (omeprazole) in higher dosages in the treatment of patients suffering from “acid-dependent” diseases of the upper gastrointestinal tract.
We studied the results of clinical, laboratory and endoscopic examination and treatment of 30 patients (10 men and 20 women) suffering from GERD in the stage of reflux esophagitis. The age of patients is from 18 to 65 years. Upon admission to the TsNIIG, 30 patients showed the main clinical symptoms of GERD (heartburn, chest pain and/or epigastric pain, belching), 25 patients had clinical symptoms mainly associated with impaired motility of the upper gastrointestinal tract (feeling of rapid saturation, fullness and distension of the stomach, heaviness in the epigastric region), usually occurring during or after meals. The combination of certain clinical symptoms, the frequency and time of their occurrence, as well as the intensity and duration of different patients were different. No significant deviations in blood parameters (general and biochemical tests), urine and feces tests were noted before the start of therapy.
During esophagogastroduodenoscopy (EGDS), 21 patients were diagnosed with reflux esophagitis (in the absence of erosions), including 4 patients with cicatricial ulcerative deformation of the duodenal bulb and one patient with a slit-like ulcer of the duodenal bulb (5 patients suffered from duodenal ulcer intestines, combined with reflux esophagitis). In addition, one patient had a peptic ulcer of the esophagus against the background of reflux esophagitis, and 8 patients had erosive reflux esophagitis. In all patients, according to endoscopy, cardiac insufficiency was detected (in combination with or without axial hiatal hernia).
In the treatment of such patients, gastrosidine (famotidine) was used at a dosage of 40-80 mg per day for 4 weeks (the first 2-2.5 weeks of treatment were carried out in the TsNIIG hospital, in the next 2 weeks patients took gastrosidine in an outpatient setting). Gastrosidin therapy was always started and continued in the absence of significant side effects; patients were prescribed 40 mg 2 times a day for 4 weeks; only when diarrhea and urticaria appeared, the dosage of gastrosidine was reduced to 40 mg per day.
The study was carried out taking into account the criteria for inclusion and exclusion of patients from the study according to the rules of clinical practice.
During endoscopy, NR was determined using a rapid urease test (one fragment of the antrum of the stomach within 2-3 cm proximal to the pylorus) and histological examination of biopsy material (two fragments of the antrum within 2-3 cm proximal to the pylorus and one fragment of the body of the stomach within 4-5 cm proximal to the angle of the stomach). When examining patients, if necessary, ultrasound of the abdominal organs and X-ray examination of the gastrointestinal tract were performed. The data obtained, including identified side effects, were recorded in the medical history.
During the study period, patients did not additionally take proton pump inhibitors, histamine H2 receptor blockers, or other so-called “anti-ulcerogenic” drugs, including antacids and agents containing bismuth. 25 out of 30 patients (84%) due to the presence of clinical symptoms, most often associated with impaired motility of the upper digestive tract, additionally received prokinetics: domperidone (Motilium) for 4 weeks or metoclopramide (Cerucal) for 3-4 weeks.
Treatment of patients with GERD in the stage of reflux esophagitis always began with the administration of gastrosidin 40 mg 2 times a day (it was assumed that in the event of significant side effects, the dose of gastrosidin would be reduced to 40 mg per day). After 4 weeks from the start of treatment (taking into account the condition of the patients), in the presence of clinical signs of GERD and (or) endoscopic signs of esophagitis, therapy was continued for another 4 weeks. After 4-8 weeks, based on the results of clinical, laboratory and endoscopic examination, it was planned to summarize the results of treatment of patients with GERD.
When treating patients with gastrosidine (famotidine), the following factors were taken into account: the effectiveness of gastrosidin in suppressing both basal and nocturnal and food- and pentagastrin-stimulated hydrochloric acid secretion, no changes in the concentration of prolactin in the blood serum and antiandrogenic effects, no effect of the drug on the metabolism of other drugs in the liver funds.
Based on the results of an analysis of the examination and treatment of patients with GERD in the stage of reflux esophagitis, in most cases the therapy was found to be effective. During treatment in patients with GERD with reflux esophagitis (in the absence of erosions and peptic ulcers of the esophagus), the main clinical symptoms disappeared within 4-12 days; in patients with erosive reflux esophagitis, chest pain gradually decreased and disappeared on the 4-5th day from the start of taking gastrosidin; in a patient with a peptic ulcer of the esophagus against the background of reflux esophagitis - on the 8th day.
Two out of 30 patients (6.6%) refused to take gastrosidin 2-3 days after the start of treatment, in their words, due to increased pain in the epigastric region and the appearance of dull pain in the left hypochondrium, although objectively their condition was quite satisfactory . These patients were excluded from the study.
According to endoscopy, after 4 weeks of treatment, endoscopic signs of reflux esophagitis disappeared in 17 out of 28 patients (60.7%), and positive dynamics were noted in 11 patients - a decrease in the severity of esophagitis. Therefore, these patients were subsequently treated with gastrosidin in an outpatient setting for another 4 weeks, 40 mg 2 times a day (7 patients) and 40 mg 1 time a day (4 patients in whom the dosage of gastrosidin had previously been reduced).
The question remains very controversial: should we consider reflux esophagitis, often observed with peptic ulcer disease (most often with duodenal ulcer disease), as a complication of this disease, or should we consider it an independent disease concomitant with peptic ulcer disease? Our long-term observational experience shows that, despite some connection between GERD and peptic ulcer (their relatively frequent combination and even the appearance or exacerbation of reflux esophagitis as a result of anti-Helicobacter therapy), still peptic ulcer and GERD (including in the reflux stage -esophagitis) should be considered independent diseases. We have repeatedly observed patients with frequent exacerbations of GERD in the stage of reflux esophagitis (if they had cicatricial and ulcerative deformation of the duodenal bulb). The last exacerbation of peptic ulcer (with the formation of an ulcer in the duodenal bulb) in these patients was observed 6-7 or more years ago (much less often than relapses of GERD in the stage of reflux esophagitis), however, with the next exacerbation of peptic ulcer with the formation of an ulcer in the duodenal bulb Reflux esophagitis was always detected during endoscopic examination of the intestines. We are confident that with the availability of modern medications, it is much easier to treat uncomplicated peptic ulcer disease than GERD: the period of therapy for exacerbation of duodenal ulcer disease takes significantly less time compared to therapy for GERD; and during the period of remission of these diseases, patients with duodenal ulcer feel more comfortable, while patients with GERD are forced to refuse to take significantly more foods and drinks to improve their quality of life.
Upon examination (after 8 weeks of treatment), three of 11 patients still had complaints associated with impaired motility of the upper gastrointestinal tract. Three patients, although feeling well, refused to undergo a control endoscopy after 8 weeks. According to endoscopy, in 7 out of 8 patients there was a disappearance of endoscopic signs of esophagitis (including healing of a peptic ulcer of the esophagus in one patient).
Determination of NR was carried out in all 30 patients: in 11 cases, NR contamination of the gastric mucosa was revealed (according to the rapid urease test and histological examination of targeted gastrobiopsy materials). Anti-Helicobacter therapy was not administered to patients with GERD in the stage of reflux esophagitis during treatment.
When assessing the safety of the treatment, no significant deviations in laboratory parameters of blood, urine and feces were noted. In 4 patients (13.3%), who previously had “normal” (regular) stools, on the 3rd day of treatment with gastrosidin (at a dose of 40 mg 2 times a day), in their words, “loose” stools were noted (mushy, without pathological impurities), and therefore the dose of gastrosidin was reduced to 40 mg per day. 10-12 days after reducing the dose, the stool returned to normal without any additional therapy. It is interesting to note that in another 4 patients who previously suffered from constipation, during treatment, stool returned to normal on the 7th day. In 3 out of 30 patients (10%), on the 3-4th day of taking gastrosidin, rashes appeared on the skin of the torso and limbs (urticaria). After reducing the dosage of gastrosidin to 40 mg per day and additional treatment with diazolin (0.1 g 3 times a day), the skin rashes disappeared.
Studies have shown the feasibility and effectiveness of therapy for GERD in the stage of reflux esophagitis with gastrosidine 40 mg 2 times a day, especially in the treatment of patients with severe pain and heartburn. Such treatment can be successfully carried out in inpatient and outpatient settings. Studying the long-term results of the treatment will make it possible to determine the duration of the period of remission of this disease and the advisability of treatment with gastrosidin as “maintenance” therapy or “on-demand” therapy.
For questions about literature, please contact the editor
Complications
Without treatment, GERD can lead to serious complications. According to the NIDDK, these may include:
- Esophagitis : This condition results from inflammation of the esophagus, which can cause ulcers and bleeding.
- Barrett's esophagus : This condition involves the replacement of the tissue lining the esophagus with tissue similar to the intestinal lining. In a small number of patients this leads to esophageal cancer.
- Esophageal stricture : This condition occurs due to narrowing of the esophagus.
In addition to problems in the esophagus, GERD can cause complications in other parts of the body. Complications include:
- chronic cough
- asthma
- inflammation of the vocal apparatus
- hoarseness
- caries
Myth: GERD is a hiatal hernia
In fact. Not always.
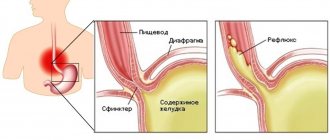
Most often, the reflux of hydrochloric acid from the stomach or bile into the esophagus (if a person suffers from cholelithiasis) occurs due to the weakness of the lower esophageal sphincter (valve), through which hydrochloric acid and/or bile from the stomach and/or aggressive for the esophagus enters. or gallbladder. With low reflux (reflux) - in the lower third of the esophagus, with high - in the middle and upper, up to the oral cavity. GERD occurs for many reasons. The provoking factors of gastroesophageal reflux disease are smoking; alcohol; carbonated drinks; work associated with a constant inclined position of the body and lifting heavy objects; stress; overeating (especially at night). All this relaxes the lower esophageal sphincter, disrupting the natural barrier necessary to protect the esophageal mucosa.
Conclusion
A person with GERD can try several home remedies to relieve symptoms. These include split meals and avoiding eating before bed.
Also, if you are interested in home remedies for GERD, you can try ginger supplements. However, you should first seek advice from your doctor.
Lifestyle changes may also help. These include quitting smoking, achieving or maintaining a moderate weight, and remaining upright after meals.
When home remedies and lifestyle changes do not relieve symptoms, doctors may prescribe medications or recommend surgery.
Myth: GERD is heartburn
In fact. Not only. Although heartburn, which torments those who suffer from gastroesophageal reflux disease (and regardless of food intake), is one of the most common and most characteristic manifestations of this disease. However, GERD also has other, at first glance, unrelated symptoms - chest pain, long dry cough, shortness of breath, hoarseness, sore throat, inflammation of the gums and tooth enamel, which some doctors, without understanding, attribute cardiovascular, dental or ENT diseases. And only after examination and treatment by a gastroenetrologist, such patients receive relief from their suffering.
Myth: GERD occurs only in people with high acidity
In fact. And that's not true. Gastroesophageal reflux disease can occur with increased, decreased, or normal acidity of gastric juice. The situation is similar with the Helicobacter pylori bacterium, which is considered not only the main provocateur of gastric ulcers, but also causes GERD. However, doctors did not come to a clear opinion on this matter. But it is known that treatment of Helicobacter with strong antibiotics disrupts the motility of both the esophagus itself and the lower esophageal sphincter, and thus stimulates the disease. Some cardiac medications, as well as non-steroidal anti-inflammatory and painkillers (especially if they contain caffeine) have the same relaxing effect on the sphincter.