Pain syndrome
The appearance of pain is typical for large cysts, as they compress the surrounding tissues, including the nerve plexuses. Small cysts do not exert such pressure, therefore, as a rule, there are no complaints of pain. This symptom is especially characteristic for the period of formation of false cysts during acute and exacerbation of chronic pancreatitis, and it is caused to a greater extent by destructive processes. Over time, the intensity of the pain decreases, it is characterized as “dull” or rather “discomfort”. A characteristic symptom is the “lucid interval” (temporary improvement and absence of pain after acute pancreatitis or injury). The most severe pain is caused by cysts located on the posterior surface of the gland and compressing the solar plexus area. Impact on this nerve plexus creates in patients a very intense, long-lasting burning pain that radiates to the back. Movement, compression by clothing, a belt, or a belt increase its intensity. The condition is somewhat alleviated when taking the knee-elbow position (“on all fours”). A pronounced increase in pain - “dagger” pain can indicate the occurrence of complications (for example, rupture of a cyst), gradual progression of pain along with an increase in body temperature and the appearance of intoxication - about its suppuration.
Dyspepsia
Other manifestations of pancreatic cysts may include dyspeptic disorders: nausea, vomiting (which may result in an attack of pain), and stool instability. As a result of the decrease in the amount of pancreatic juice entering the intestines, the digestion of food and the absorption of nutrients are disrupted. As a result, the patient loses weight, loses weight, and becomes weak.
Intestinal obstruction
Sometimes large pancreatic cysts cause compression of neighboring organs, impairing their patency. When a cyst is located in the head of the gland, obstructive jaundice may occur (yellowishness of the skin, sclera, and itchy skin appears); if the portal vein is compressed, swelling in the legs or ascites develops. Very rarely, large pancreatic cysts compress the intestinal lumen (duodenum), which interferes with the passage of food. In these cases, incomplete high intestinal obstruction may form.
General information
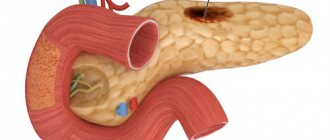
According to the definition of the World Gastroenterology Organization (2019), “a pancreatic cyst is a well-defined formation in the pancreas containing fluid.” They can be located both inside the pancreas and protrude beyond its borders. Despite the relative rarity of this pathology (about 0.2%), there is a negative tendency towards its increase, especially in young people, which is to a certain extent due to the increase in complicated/destructive forms of acute/chronic pancreatitis and the capabilities of modern imaging technologies used in the diagnosis of diseases abdominal organs.
There are two large groups of pancreatic cysts: true (congenital), the cavity of which is filled with mucous epithelium, and acquired (false) cysts, predominantly limited by a fibrous capsule, which are most often represented by postnecrotic cysts of the pancreas, which are the most common (up to 55% of cases) complication of pancreatitis. ICD 10 pancreatic cyst code: K86.2. Pancreatic cysts are most often benign, but some types have a high potential for malignancy. For example, mucinous cystic/intraductal papillary mucinous cysts have a high potential for malignancy, while pseudocysts, simple cysts and serous cystic neoplasms are almost always benign. According to the World Gastroenterological Organization, the risk of malignancy of true pseudotumor cysts on average for intraductal papillary cysts is 41%; mucinous cysts - 25.2%, intraductal pseudopapillary cysts - 18.3%, serous cysts - 15.2%, while the frequency of malignancy of false cysts does not exceed 0.3%.
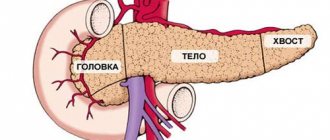
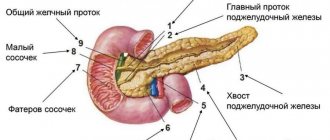
Additionally, malignant cysts ( adenocarcinomas / pancreatic cystic neuroendocrine tumors ) are included in a separate category. The cyst can have different localization: cyst of the head; body and tail of the pancreas. In approximately 85% of cases, cysts are localized in the body/tail of the gland and only in 15% of cases are localized in its head. Less commonly, two or multiple cysts form.
The occurrence of certain types of pancreatic cysts varies significantly. Thus, the share of true cysts accounts for 15-20%, and the share of acquired (false) cysts is almost 80%, while the cause of the formation of post-necrotic cysts in 50-60% are destructive forms of acute pancreatitis and in 15-30% - traumatic injuries PJ. Accordingly, the most common morphological form, postnecrotic cysts, will be considered below.
The particular significance of this type of cyst is determined by the frequent complications in the form of cyst suppuration (15.6%), bleeding (11.3%), perforation (6.7%), malignancy (5.6%), false aneurysm (3.1% ), fistulas (1.4%), obstructive jaundice (3.5%), duodenal stenosis (1.6%), acute intestinal obstruction (0.4%), which determines high mortality rates (from 9.2 to 53%).
Standard classification
To understand the diameter of the affected area, its location, and also to find out whether the inflammation has affected neighboring soft tissues, modern diagnostic methods are used. They are considered a mandatory item in the plan before prescribing a surgical intervention, which allows not only to study the problem in detail, but also to use the collected information during the operation itself.
Content:
- Standard classification
- Features of each type
- When is it time to see a doctor
- Radical approach
- Success forecast
The most productive versions of diagnostics are computed tomography and magnetic resonance imaging, as well as ERCP. In the first two cases, the stage of adding a contrast agent is not mandatory, but the last type of analysis is completely based on it.
Only after receiving the visualization in hand does the attending specialist make the final decision regarding whether the operation is possible and which format will be the most effective. Most often, classic internal or external drainage is used. A little less often, experts resort to resection of part of the pancreas along with the area that threatens the entire body.
According to statistics, pancreatic cysts have been diagnosed much more often in recent years, and mostly young people become its victims. Researchers explain the sharp rejuvenation of patients in the gastroenterology inpatient department by the fact that young people more often began to suffer from acute and chronic pancreatitis. Moreover, their etiology varies from classic traumatic to biliary or acquired alcoholic, which over the last ten years has become a real scourge among doctors.
According to the same statistical summary, a cyst is the most common consequence of complications of chronic pancreatitis. It accounts for about 80% of clinical cases of the total.
Difficulties are added by the fact that in the medical community there is no common understanding of what formations should be classified as pancreatic cysts. Because of this, one general set of rules regarding the classification of such pathology is not provided, as well as standards of pathogenesis with the provision of care.
Some adherents insist that the cyst must have pancreatic juice inside and also be limited to the walls. Others believe that the contents may even be necrotic parenchyma or:
- blood;
- pus;
- inflammatory exudate.
The only thing both camps agree on is the principles of anomaly formation. They provide the following conditions:
- parenchymal damage;
- problematic secretion outflow;
- local failure of microcirculation.
There is a separate classification of pathologies, which is divided according to the parameters of their formation. But even they have several divisions for the convenience of establishing a specific diagnosis. Basic sorting involves dividing diseases into the following types:
- congenital;
- inflammatory;
- traumatic;
- parasitic;
- neoplastic.
The first item includes several more subitems such as dermoid and teratoid, as well as fibrocystic degeneration, adenomas, and polycystic disease.
But frequently occurring pseudocysts are a representative of a number of inflammatory categories, which also include retention variants. Separately, there is a sorting for neoplastic versions, which affects the following subtypes:
- cystadenomas;
- cavernous hemangiomas;
- cystadenocarcinoma;
- epitheliomas.
They all differ in the course of the disease, cure measures, and approaches to rehabilitation therapy.
Pathogenesis
The development of pancreatic cysts occurs under the influence of provoking factors, resulting in discomplexation of pancreatocytes in the pancreas with the development of small diffuse necrosis of acinar (secreting) cells. As a consequence, there is a violation of secretion into the lumen of the ducts and parapedesis of secretory granules in the interstitium. Destroyed cells promote interstitial/intracellular activation of trypsin, which activates pancreatic hydrolytic/proteolytic enzymes, which in turn contribute to autoenzyme aggression and the development of foci of necrosis, which is manifested by regional rheological disorders and severe interstitial edema.
Resorption of pancreatic enzymes from the interstitium contributes to autolytic damage to blood vessels with the subsequent development of thrombohemorrhagic local syndrome.
The formation of fluid accumulations is based on the processes of lysis of foci of infiltration/necrosis. The formation of fluid accumulations is ensured mainly due to the exudative reaction of inflamed tissues and, to a lesser extent, due to pancreatic juice arriving due to a violation of the outflow of juice along the main pancreatic duct. As a result of a pronounced violation of capillary permeability, almost within 1–2 hours after the destruction of the acini, many mast cells/leukocytes appear in the tissues, actively secreting biologically active substances, which leads to the formation of a demarcation shaft around the focus of necrosis, consisting of leukocytes, fibrin, histeocytes, lymphoplasma cells components and nuclear detritus.
Activation of fibroblasts promotes the intensive formation of elements of connective tissue structures/collagen, which serve as the basis for the formation of a barrier, which subsequently becomes the base of the postnecrotic cyst capsule.
Classification
It is customary to distinguish the following types of pancreatic cysts.
True cysts:
- Congenital (single/multiple cysts, localized in the pancreas itself; combined with cysts in the liver/kidneys and other organs; cystic fibrosis of the pancreas).
- Acquired (retention cysts caused by retention of pancreatic secretions; parasitic cysts (for example, hydatid cysts); primary tumor cysts - cystadenomas/cystadenocarcinomas and metastatic ones.
Pseudocysts (extrapancreatic/intrapancreatic):
- Being predominantly the outcome of pancreatic necrosis ;
- Post-traumatic cysts (open/closed injuries of the pancreas, operations on the pancreas and adjacent organs).
- Idiopathic.
- Cysts communicating/not communicating with the pancreatic ducts.
According to course/clinical signs
By degree of formation:
- The first stage is acute (the cyst is not formed, the time period is up to 1.5 months from the moment of occurrence).
- The second stage is subacute (a cyst wall has been formed, which consists of loose granulation tissue), over a time period of 2-3 months.
- The third stage - the cyst wall is closely connected with the surrounding tissues.
- The fourth stage - the cyst wall is finally formed and is represented by a dense fibrous capsule, over a period of more than a year.
By location (pancreatic head cyst, pancreatic body cyst, and pancreatic tail cyst).
According to the morphological characteristics of the cysts (intrapancreatic/extrapancreatic; single/multiple; single-chamber/multi-chamber).
According to the severity of the course : simple and complicated (malignancy, suppuration, bleeding, fistula formation, perforation, compression of surrounding organs).
Histological classification (table below).
Features of each type
After a pathology is discovered, the doctor must anticipate its type in order to then deal with a specific program of therapeutic measures. Some experts believe that a cyst after trauma is as complex as the identical development of events in acute or chronic pancreatitis. First, autolysis of the enzymatic format occurs in the affected area of the pancreatic parenchyma, followed by the formation of a loose infiltrate. It contains tissue breakdown products.
Over time, it turns into a kind of capsule, which provokes the formation of a false cyst, which does not have a layer of lined epithelium. A real cyst communicates with the duct, being inside the pancreas, or outside if the size of the formation is too large.
Scientists never name the average size of such inflammation, since they can vary from giants with several liters of accumulated fluid to tiny objects, which is characteristic of polycystic disease. During the observations, the researchers came to the conclusion that in women the most common reason for such a verdict is pancreatitis of any kind, and in men it is an abdominal injury.
Congenital abnormalities are often found in children, since they try to manifest themselves with unpleasant symptoms from the very beginning. It is believed that this option is the logical conclusion of dysontogenesis. They are found both singly and in colonies.
At a particularly advanced stage, they are combined with identical formations in neighboring organs:
- liver;
- kidneys;
- ovaries.
Even combinations with the brain have been recorded in clinical practice.
Traditional contents imply a granular mass, cavities with dermoid tissues. The primary source of the problem is the incorrect formation of embryonic anlages, such as individual glandular lobes, separated from the main mass of the gland. Sometimes they ectopize into the gastric walls.
If we consider a kind of popularity rating, then the inflammatory type of formations becomes the leader of the list, for which we should “thank” pancreatitis that is not fully cured or left to chance. When a person becomes a victim of its acute form, degenerative processes contribute to the formation of an infiltrate, to which a capsule and cavities are later added.
The result of chronic pancreatitis looks a little different, expressed in islands of connective tissue, as well as in a narrowing of the duct with periodic expansions. Because of this, already during the operation the surgeon can decide to get rid of stones that block the normal transfer of secretions. They are so small that ultrasound does not notice them.
When the duct narrows inside the glandular lobe, a regular cyst forms. But if there is a prestenotic expansion of the path, then a large spherical obstacle of a retention nature cannot be avoided. Its feature is called dense fibrous walls, a tight vascular sect, and lining with cubic epithelium. The contents of the lesion range from almost clear liquid to a thick brown consistency.
Much less common are situations where the cause of formation is parasitic influence. In fact, this only means the onset of the vesicular stage of echinococcus development. Due to the effects of the latter, the head is often affected. But if cysticercosis was detected, then the body with the tail was hit.
Physiologically, the wall of the parasitic variant consists of a fibrous capsule together with a chitinous membrane created by the body itself. The only good thing here is that cystadenomas are among the rarest medical diagnoses in the gastroenterological part.
Based on the presented schematic classification, doctors develop a further strategy for providing care, selecting the optimal surgical intervention.
Causes
The development of pancreatic pseudocyst is based on polyetiological factors, the main of which are:
- Acute/chronic destructive pancreatitis .
- Traumatic injuries of the pancreas.
- Blockage of the bile ducts (congenital or caused by the presence of stones (cholelithiasis), tumors, strictures, scars, persistent narrowing of the walls (stenosis).
- Parasitic infestations ( echinococcosis , opisthorchiasis , cysticercosis ).
Risk factors include:
- Abuse of alcoholic beverages.
- Obesity with lipid metabolism disorders, accompanied by increased cholesterol .
- Cholelithiasis (stones in the bile duct/gallbladder).
- Diabetes.
- Surgeries on the pancreas or adjacent organs.
Symptoms
The symptoms of a pancreatic cyst are extremely ambiguous, since it is largely determined by the size, type, shape, and localization of the cystic neoplasm. Cysts of small diameter on the pancreas (up to 3 cm) in most cases are asymptomatic, since they do not compress the adjacent nerve plexuses/vessels and are diagnosed accidentally. Most often, a pancreatic cyst manifests itself with weakness, a feeling of discomfort in the abdominal cavity, loss of appetite, moderate/occasionally acute pain, less often nausea and vomiting, and fever.
The enzymatic deficiency syndrome is characterized by progressive loss of body weight, the appearance of symptoms of steatorrhea , dehydration, and anemia , which is caused by a disruption in the breakdown of proteins/fats with the development of protein-energy deficiency. During an objective examination, asymmetry of the abdomen may be noted; upon palpation, tension in the upper/middle part of the abdomen may be noted.
As the size of the cyst increases, compression syndrome of adjacent organs is characteristic: when the cyst is localized in the head of the gland, the development of obstructive jaundice, which is manifested by skin itching and icterus of the sclera/skin; with pressure on the portal veins - swelling in the lower extremities; If the cyst is large and interferes with the flow of urine, urinary retention is typical. When the nerve plexuses are compressed, a burning, burning pain occurs. When the cyst suppurates, intoxication syndrome appears.
Tests and diagnostics
The diagnosis of pancreatic cyst is made on the basis of:
- patient complaints;
- anamnesis data (presence of provoking factors);
- results of an objective study (asymmetry of the abdomen, the presence of a volumetric protrusion on the anterior abdominal wall in the area of gland projection);
- laboratory data ( leukocytosis , increased bilirubin / alkaline phosphatase , increased ESR);
- data from instrumental studies - ultrasound, EUS (endoscopic ultrasound), CT, MRI/MRCP (magnetic resonance cholangiopancreatography), which visualizes a cyst-like neoplasm, as well as the location of the cyst, its size, changes in the gland, the presence of partitions/chambers in its cavity, wall thickness and nature of the contents.
Differential diagnosis of pancreatic cysts is carried out with pancreatic cancer, liver cysts, stomach tumors, kidney tumors, colon cancer, aortic (abdominal) aneurysm.
Postoperative period
After the operation, the patient is monitored in the intensive care unit for several days. From the first day it is important to mobilize the patient and breathing exercises to prevent pneumonia. Particular attention is paid to blood sugar levels in order to promptly recognize possible diabetes mellitus caused by such operations. Gradual restoration of nutrition, therapeutic exercises, and respiratory therapy are carried out. When a large part of the pancreas is removed, replacement therapy for enzymes produced by the pancreas is started. As a rule, the patient is discharged 10-14 days after surgery.
Diet
Diet 5th table
- Efficacy: therapeutic effect after 14 days
- Duration: from 3 months or more
- Cost of products: 1200 - 1350 rubles per week
It is the most important component of the treatment process both during conservative therapy and after surgical intervention. The main one is Table No. 5 (pancreatic) for the entire period of treatment and No. 5, which is prescribed if necessary for up to 1 year. Most patients with this pathology (forum “pancreatic diseases”) believe that it is dietary nutrition that helps minimize the risk of complications.
Treatment of pancreatic cyst - surgery
The clear answer is surgery only! Modern technologies make it possible in many cases to avoid major surgery and limit ourselves to minimally invasive endoscopic or endovideosurgical intervention.
The following methods of treating cysts are possible:
- Removal of the cyst itself or a cystic part of the pancreas.
- Internal drainage of the cyst.
- External drainage of the cyst.
With the first method, as a rule, the cyst is removed along with a section of the pancreas. The volume of intervention depends on the size of the formation, on the location where the cyst is located, on the condition of the tissues adjacent to it. Distal resection, distal or pancreatoduodenal resection, are quite complex and require appropriate technical and medical support. Currently, these operations are included in the list of types of high-tech medical care performed under quotas from the Ministry of Health of the Russian Federation or under compulsory medical insurance policies. These operations can be performed in our Clinic both traditionally and laparoscopically.
Drainage operations are considered the most physiological and less traumatic, which are aimed at creating an outflow from the cyst into the stomach, duodenum or small intestine using internal drainage. An anastomosis is created, which ensures the delivery of gland juice to food, which relieves the pain reaction and rarely leads to relapses. Currently, it is also possible to perform these operations using endoscopic techniques, which are performed endovideosurgically or endoscopically with ultrasound guidance.
External drainage of cysts in planned surgery has recently been rarely used. The choice of this type of intervention is most often forced in emergency situations. Indications for this method:
- if the process of cyst formation has not completed;
- serious condition of the patient;
- suppuration of the cyst.
Such interventions are called palliative, they do not solve the problem, but can lead to relapse, to fistulas. They are used as one of the stages of patient treatment. Drainage operations can be carried out only after confirmation of a non-tumor cause of the formation.
Conservative treatment of the underlying disease is mandatory. For pancreatitis, it is imperative to follow a diet, the purpose of which is to reduce the secretion of pancreatic juice as much as possible.
Enzyme replacement drugs and analgesics are used; secretion suppressants. It is imperative to monitor the level of glycemia and, if necessary, correct it.
Consequences and complications
Why is a cyst in the pancreas dangerous? The danger lies in the high risk of complications. The most common complications of unresolved false cysts are severe pain and extrahepatic cholestasis / duodenal obstruction caused by external pressure, rupture into the abdominal cavity, pseudoaneurysm , bleeding and formation of a pancreatic abscess .
Diagnosis of a cyst
Ultrasound examination can diagnose cysts in all parts of the pancreas - head, body and tail. Endoscopic ultrasound additionally allows you to determine the benignity or malignancy of the formation.
Diagnostic methods are quite varied. On a plain radiograph of the abdominal cavity, a shadow can be identified, the position of which corresponds to the boundaries of the cyst. If this study reveals deformed borders of the stomach, a cyst is also suspected.
Duodenography reveals the contours of the cyst with great reliability. During irrigoscopy, large, downward-sloping cysts and polycystic pancreas can be detected; with angiography of the branches of the celiac artery, the contours of cysts of any size are clearly visible.
Forecast
The prognosis for pancreatic cysts depends on many factors (risk of malignancy , development of complications, timeliness/adequacy of treatment). In general, with timely and adequate treatment of pancreatic false cysts with a low risk of malignancy, the prognosis is favorable. At the same time, with the development of complications, the prognosis significantly worsens. The most dangerous complication of a false cyst is its rupture, accompanied by shock , the mortality rate of which in the absence of bleeding is 14%, and with accompanying bleeding reaches 60% and is the leading cause of death.
Mineral water for treatment
It can completely replace teas and plain water or drink along with them. Mineral water contains vitamins and minerals: calcium, magnesium, sodium, boric acid.
Since it stimulates the production of insulin, drinking mineral water for several weeks will have a beneficial effect on the condition of the pancreas.
Before treatment with folk remedies, you need to undergo a full examination and consult a doctor to rule out allergic reactions and intolerance to components.
These remedies will help relieve inflammation and stop the growth of the cyst, but will not get rid of the cyst itself, so you need to go to the hospital to remove it.
List of sources
- Grishakov S.A., Kubyshkin V.A., Karmazanovsky G.G. Cystic tumors of the pancreas. // Surgery. - 2006. - No. 11. - P. 65-70.
- Bayramalova L.A., Valeeva F.A., Shamsiev R.E., Zhuravlev I.A. DIAGNOSIS AND TREATMENT OF PANCREAS CYSTS // Advances in modern natural science. – 2014. – No. 6. – P. 23-25;
- Grishin I.N., Grits V.N., Lagodich S.N. Cysts, fistulas of the pancreas and their complications. – Minsk, 2009. – 272 p.
- Korolev M.P., Fedotov L.E., Avanesyan R.G., Turyanchik M.M., Fadeeva Yu.V. Combined minimally invasive technologies in the treatment of post-necrotic pancreatic cysts and their complications // Annals of Surgical Hepatology. – 2012. – T.17, No. 4. – P.57–65.
- Treatment and tactical approaches in patients with pancreatic pseudocysts/V.V. Boyko, I.A. Krivoruchko, A.M. Tishchenko [and others] // Clinical surgery. - 2004. - No. 6. - P. 16-19.
Surgical treatment of pancreatic cysts as a complication of acute pancreatitis
Introduction. Acute pancreatitis is one of the most common emergency surgical diseases and the main cause of the development of pancreatic cysts, especially after destructive pancreatitis, but the formation of cysts in the chronic form of pancreatitis and after trauma to the pancreas cannot be ruled out [2,6,16]. Previously, the diagnosis of cysts was complex and was based mainly on data from objective and x-ray studies, but in recent years, with the advent of new diagnostic equipment (ultrasound, computed tomography, magnetic resonance imaging), the frequency of identifying patients with pancreatic cysts has increased [3,7, 8.13], which may subsequently be complicated by suppuration, perforation, diagnosis and treatment become more complex. Formed pancreatic cysts are an absolute indication for surgical treatment due to the possibility of developing a large number of complications (suppuration, bleeding, perforation, formation of internal fistulas, etc.). Considering this circumstance, the treatment of cysts is only surgical, since the use of medications does not lead to the resorption of cysts [1,4,15]. The proposed methods for treating pancreatic cysts belong to the category of complex interventions, since the cysts initially represent a “decay cavity” in the omental bursa, the boundaries of which are the inflamed walls of the surrounding organs.
In this case, methods of external or internal drainage of the cyst can be used (imposition of cystogastroanastomosis, cystoduodeno-, or cystoenteroanastomosis); combined external-internal drainage, radical operations (enucleation of a cyst, resection of the pancreas with a cyst); endoscopic, laparoscopic and other minimally invasive puncture-catheterization interventions aimed at external and (or) internal drainage of cysts under the control of topical imaging methods [5,9,10,11,14]. But when using them, it is not always possible to achieve obliteration of the cavity, relapse and complications cannot be ruled out, which require longer hospital treatment and additional costs of medications, and sometimes require repeated surgical treatment, and therefore there is a search for the most effective treatment measures that allowed to achieve clinical recovery. In addition, with internal drainage, nasocystic drainage is always used, which is poorly tolerated by patients due to the occurrence of an inflammatory process in the nasal passages, oropharynx, and esophagus, and early removal of the probe does not ensure sanitation and obliteration of the cyst cavity.
Taking into account the shortcomings of existing methods of surgical treatment, we have improved the method of simultaneous double internal and external drainage of pancreatic cysts.
Purpose of the work: to evaluate the effectiveness of an improved method of simultaneous double internal drainage with external drainage in the treatment of pancreatic cysts.
Material and research methods. From 2014 to 2015, 11 patients with cystic lesions of the pancreas, the size of which exceeded 10 cm, were under observation at the city clinical hospital No. 1 of Bishkek from 2014 to 2015. There were 4 women aged from 30 to 72 years, 7 men aged from 36 to 76 years old. In most patients, inflammatory pancreatic cysts were detected - 10; a post-traumatic pancreatic cyst was found in one patient due to blunt abdominal trauma. A detailed examination revealed concomitant diseases in 8 patients: hypertension in 4, bronchopulmonary diseases in 3, coronary heart disease in one patient.
The duration of the disease ranged from 4.5 months to 4 years. Inflammatory pancreatic cysts were considered as a complication of acute or chronic pancreatitis. The leading etiological factor of pancreatitis in the patients we observed was the systematic consumption of alcohol in 8 people; in 2 patients who had not previously consumed alcohol, acute pancreatitis developed after eating large fatty and spicy foods, and in one patient a pancreatic cyst developed after an abdominal injury.
The localization of pancreatic cysts, taking into account their location relative to the parenchyma, was different. Thus, in 2 patients the cyst was located in the head of the gland, in 8 in the body and in one in the tail area.
In establishing the diagnosis of pancreatic cysts, the following set of diagnostic methods was used, including general laboratory data, determination of specific indicators of the excretory and endocrine functions of the pancreas (complete blood count, urinalysis, bilirubin, aspartate aminotransferase, alanine aminotransferase, total protein, C-reactive protein, glucose blood, blood amylase, urine diastasis according to generally accepted methods), as well as instrumental research methods: ultrasound, and in unclear cases, computed tomography and magnetic resonance imaging were performed.
Results and its discussion. Clinical manifestations of patients with pancreatic cysts consisted of several groups of symptoms. The pain syndrome, which manifested itself as constant dull, aching pain in the epigastric region or in the left hypochondrium, was paroxysmal in nature with irradiation to the back and left shoulder; they were most likely caused by both the pathology of the pancreas itself and the pressure of the cyst on nearby organs. Such manifestations were typical for all patients.
Another group of symptoms was associated with the exocrine and endocrine function of the organ (nausea, periodic vomiting, loose stools, weight loss), which we noted in 6 patients.
The third group of symptoms is explained by compression of the antrum of the stomach, hepatoduodenal ligament and duodenum by the cyst, which manifested signs of gastrostasis in 3 patients, and in one case the pancreatic cyst was complicated by jaundice (total bilirubin was 156 µmol/l).
To determine the degree of maturity of a pancreatic cyst, we used ultrasound indicators, which are described in detail in the work of Achkasova E.E. et al. [1].
The first degree of maturity is characterized by the presence of formations of various shapes and sizes with unclear contours and reduced echogenicity.
For the second, cysts appear as an echo-negative formation of various sizes, round in shape and with clear contours and a capsule 1-3 mm thick, and the capsule runs along the entire circumference. The pancreatic duct is often unchanged.
In the third degree of maturity, echograms also reveal a rounded formation, but the capsule is thicker (4 mm or more) and in some cases inclusions are found in the lumen of the cyst. The degree of maturity of the cyst should be taken into account when choosing a treatment method. The authors argue that in the first stage of cyst maturity it is advisable to use a puncture method of treatment or external drainage, and in the second stage it is advisable to apply cystodigistial anastomoses, which we took into account in the treatment of pancreatic cysts. In the third degree of maturity, it is necessary to remove the cyst.
In all patients we operated on, pancreatic cysts had the second degree of maturity. During ultrasound examination, echograms are presented in the form of an echo-negative formation, round in shape with clear contours and a capsule 1-3 mm thick, which can be traced over the entire surface. The main pancreatic duct was not dilated in all cases (Fig. 1).
Rice. 1. Cyst of the second degree of maturity.
Preoperative preparation included infusion therapy (saline sodium chloride solution with a complex of vitamins B and C, reopolyglucin, infuzol, refortan, etc.) aimed at reducing intoxication.
Before the operation, 15-20 minutes intravenously, after the test, 1.0 cefazalin or ceftriaxone was administered, and after completion of the operation, antibiotics were administered intravenously again. After the operation, intravenous administration of the same antibiotics was continued 2 times a day for 4-5 days.
In addition, on the day of surgery, an ultrasound examination was performed again and the contours of the localization of the pancreatic cyst were applied to the skin, which was the basis for us to choose an approach in order to go directly to the cyst and carry out all stages of the operation without difficulty.
After examination, all patients were operated on under general endotracheal anesthesia using muscle relaxants. The choice of access was made based on the location of the pancreatic cyst: if the cyst was localized in the head and body - upper-median laparotomy, if in the caudal region - left hypochondrium laparotomy.
The operation on these patients was performed according to our improved method: one-stage double internal drainage with external drainage, for pancreatic cysts with pancreatic cystojejunostomy on a switched-off loop according to Roux (Patent No. 1667 dated 08/29/2014 issued by Kyrgyzpatent), in all those operated by us the size of the cysts exceeded 10 cm.
Surgery technique: upper-middle or left hypochondrium, depending on the location of the pancreatic cyst, laparotomy, which allows for a full inspection of all parts of the pancreas, bile ducts and neighboring organs. After isolating the cyst wall, a puncture was performed, the contents of the cyst were sent for bacteriological, cytological and biochemical examination, and a section of the cyst wall was sent for histological examination to exclude malignant growth.
After removing the contents of the cyst, the cavity was opened and examined; if there were sequestration and necrotic tissue, then a necrosequestrectomy was performed. A thin silicone drainage tube was passed through the upper lateral wall into the cystic cavity, fixed with catgut, and the drainage was removed through a separate contraperture in the left hypochondrium. Such drainage is necessary for complete and timely evacuation of the contents of the cyst, sanitization of its cavity in the postoperative period and to prevent stagnation and infection, as well as for further dynamic monitoring of the functional viability of the anastomosis. Next, pancreatocystojejunostomy was formed.
To apply it, it is advisable to use a loop of jejunum at least 40 cm away from the ligament of Treitz, connected by a Y-shaped anastomosis according to Roux, which prevents or reduces the possibility of cystodigistial reflux. The formation of an anastomosis with the “disconnected” jejunum significantly reduces the likelihood of infection of the cyst cavity and the progression of pancreatitis. The operation diagram is shown in Fig. 2.
Rice. 2. Method of one-stage double internal with external drainage of a pancreatic cyst.
In the postoperative period, the cyst cavity was washed daily through a drainage tube twice a day with a 0.02% antiseptic solution of decamethoxin or an ozonated physiological solution of sodium chloride with an ozone concentration of 8-10 μg/ml.
We settled on these solutions, since ozone has a powerful bactericidal, antiviral and antioxidant effect, and decamethoxin is a modern antiseptic that belongs to the group of detergents, which is a surfactant that concentrates on the cytoplasmic membrane of the microbial cell, disrupting the permeability of the cytoplasmic membrane of microorganisms. During treatment with decamethoxin, the sensitivity of antibiotic-resistant microorganisms to antibiotics increases [12]. It has been established that the use of decamethoxin does not cause toxic effects. After the operation, the nature and volume of discharge from the cyst cavity was monitored daily with mandatory biochemical testing, and if the level of pancreatic enzymes (amylase, lipase, trypsin) increased, protease inhibitors (Gordox, Cantrical, Sandostatin) were included in the treatment complex. In addition, in the postoperative period they included infusion, symptomatic therapy and intravenous antibiotics, painkillers according to indications, and an ultrasound examination was performed every other day or two for the timely detection of complications from the pleural and abdominal cavities (pleurisy, fluid accumulation in the abdominal cavity, pelvis and etc.), and on days 5-6 after surgery - an x-ray examination to determine the size of the cyst cavity with a water-soluble contrast agent. When confirming a decrease in the volume of the cyst cavity, satisfactory evacuation of contrast and the absence of discharge from the cavity, the drainage tube was removed, this was usually on the 8-9th day, and if the cavity decreased slightly, then the drainage was delayed for another 4-5 days, this was observed in 2 patients and their drainage was removed on days 13-14 after surgery.
In the postoperative period, we did not observe any complications in any patient. The hospital stay was 12.0±1.32 bed days. In all patients, a control ultrasound examination did not reveal any cystic formations of the pancreas; the anastomosis was consistent and functioning satisfactorily.
Control examination after 6 months, which was performed in 8 patients. All of them were in satisfactory condition, one patient noted periodic epigastric pain, but it quickly passed and did not require additional treatment. Ultrasound and X-ray examination confirmed the integrity of the anastomosis and the absence of pathological changes.
Thus, our studies have shown that cure of pancreatic cysts can be achieved through their timely identification, the use of assessing the degree of maturity of the cyst during ultrasound examination before the development of complications and the use of the technique we developed, including simultaneous double internal with external drainage of patients with pancreatic cysts.
Conclusions:
- Many factors contribute to the occurrence of pancreatic cysts: inflammation (acute and chronic) of the pancreas, trauma.
- The use of one-stage double drainage of a pancreatic cyst with external drainage prevents the occurrence of anastomositis, cystodigistous reflux, ensures faster obliteration of the cyst cavity and leads to a reduction in hospital treatment time.