For many people, the word "bacteria" connotes imminent evil. However, among these microscopic living forms there are different species. Some always bring only disease, so they are very dangerous. Others, on the contrary, do good, performing functions important for the life of people and animals. Representatives of the third group, which includes lactose-negative E. coli bacteria, can be both beneficial and dangerous, and therefore are called conditionally pathogenic. Some patients, seeing the presence of incomprehensible “E. coli" are very upset and rush to start treatment immediately. This is not advisable to do in all cases, since these bacteria must be present in the intestinal microflora, but their number should always be normal. Both its excess and its decrease cause a disease - dysbacteriosis.
What is E. coli
To make it clear what will be discussed in the article, we will explain the name of the microorganisms - E. coli lactose-negative. They are also called E. coli because they live in the intestines of humans and some species of mammals. In Latin it sounds like Escherichia coli. The name “Escherichia” is given to microorganisms in honor of the Austrian scientist Theodor Escherich, who was the first to discover them. The term “lactose” means that they reproduce well on lactose, that is, in milk media, and “negative” emphasizes their activity that is harmful to the human body. In the E. coli group, in addition to lactose-negative, enterohemorrhagic, enteroinvasive, enterotoxigenic and enteropathogenic Escherichia coli are distinguished. Any amount of them in the intestines is dangerous for health.
A microscope allows you to see what they look like. E. coli lactose-negative and other Escherichia actually look like short rods with rounded ends. They are up to 0.8 microns wide and up to 3 microns long. Sometimes these bacteria end up connected to each other, forming chains. On the outside, their shell is covered with pili - villi, which help the microbe to attach to the intestinal walls and be insensitive to many antibiotics. At the end, Escherichia has a flagellum, with the help of which they move quite quickly. Therefore, once they enter, for example, the genitals, they are able to move to the kidneys, prostate, and bladder.
Lactose-negative E. coli are facultative anaerobes, that is, they do not need oxygen for their life, but they tolerate its presence without difficulty.
These bacteria, like all Escherichia, have many strains that differ from each other in some external characteristics, reaction to antibiotics, secreted toxins and other characteristics.
Lactose-negative enterobacteria are typical representatives
Escherichia coli is a representative of the group of lactose-negative enterobacteria.
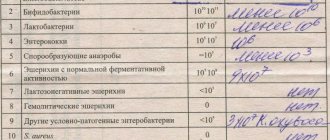
In the analysis form you will see the general indicators of this group and separately for each type of microorganism. The group of lactose-negative enterobacteria includes:
- hemolyzing Escherichia coli;
- Klebsiella;
- proteas;
- hafnia;
- serrations;
- enterobacters;
- Citrobakers.
Some of them are normal inhabitants of the intestine in small quantities, while others should not be present in the human microflora.
The benefits of E. coli
Some sources indicate that lactose-negative E. coli enter the fetal gastrointestinal tract in the mother’s womb, but most bacteriologists are inclined to believe that they colonize the baby’s intestines in the first two days after birth. E. coli do not stay in the stomach because the environment there is not suitable for them. Having penetrated the intestines, they attach to its walls, where they live as long as their carrier is alive. While there are 10*5 CFU/g of them (this is only 1% of all microorganisms in the intestines), they are doing useful things:
- produce B vitamins, lactate, succinic, formic, acetic and lactic acids, biotin, vitamin K;
- process oxygen, thereby promoting the vital activity of bifidobacteria, without which there can be no normal digestion of food;
- prevent many pathogenic bacteria from settling in the colon.
In other words, these bacteria are necessary in certain quantities. Some strains are even used as a probiotic and are purposefully introduced into the intestines for certain diseases. Therefore, if the analysis showed their presence is normal, then there is no pathology.
Enterobacter
Enterobacter - lives in the human large intestine. It is considered an opportunistic bacterium and is capable of causing various diseases of the gastrointestinal, urinary and respiratory systems.
In a urine test, this microorganism should contain no more than 10 * 5 pieces. per 1 ml of biological fluid. In stool analysis – no more than 10*4. If the level of leukocytes in the urine is increased, then the level of Enterobacter 10 * 4 units is critical. Signs of damage by Enterobacter:
- nausea;
- vomit;
- temperature increase;
- chills;
- feverish condition;
- pain in the lumbar region.
Treatment is carried out using antibiotics, bacteriophages, and drugs that improve the body's microflora.
E. coli lactose-negative: proliferation. What it is?
In medicine, the term “proliferation” means the growth of tissue. In relation to bacteria, this is their excessive growth. Normally, E. coli colonizes the large intestine. When they proliferate, they migrate in large quantities into the thin tissue, causing dysbacteriosis in it. E. coli begin to ferment (ferment) carbohydrates, which leads to the formation of methane, hydrogen and CO2. Because of this, the patient experiences bloating. Fermentation also produces fatty acids, which stimulate the formation of water in the intestines. As a result, the person begins to experience diarrhea. Proliferation of microbes into the small intestine causes deconjugation and loss of fatty acids, which provokes cholelithiasis.
If overly multiplied bacteria manage to penetrate into the blood through ulcerations in the intestinal walls, they spread to many organs, causing various diseases, such as meningitis, gastroenteritis, peritonitis, and sepsis.
Serrations
Enterobacter - lives in the human large intestine.
Serrations are a widespread microorganism. It is a facultative anaerobe and produces a natural red dye.
Until the 60s of the last century, serration colonies were used as a dye to test air circulation.
It has been proven that 10% of nosocomial infections are caused by these microorganisms. The mortality rate when infected by this bacterium is 26%.
Dysbacteriosis in infants: causes and symptoms
In normal condition, babies must have beneficial bacteria in their intestines. If lactose-negative E. coli is elevated, the infant may develop dysbiosis. This occurs due to low immunity in newborn babies and the inability of their body to control the number of bacteria. Signs of the disease:
- bloating;
- flatulence;
- frequent regurgitation, sometimes vomiting;
- rumbling in the stomach;
- diarrhea (watery, foamy stool with a characteristic odor);
- allergic dermatitis;
- weight loss.
Undigested grains of food and mucus may be observed in the stool.
If your baby defecates too often, he or she may become dehydrated. Its symptoms:
- rare urination;
- weakness;
- dry lips, tongue.
In some cases, lactose-negative E. coli in the stool of an infant is elevated, but the child is active, eats well, and gains weight.
It depends on the characteristics of his immune system. In addition to the disturbance in the number of opportunistic E. coli, in the first days and weeks after birth, dysbiosis can begin due to the entry of enteropathogenic E. coli into the infant’s gastrointestinal tract. You can become infected with them through mother's milk, through a dirty pacifier, toys, medical instruments, poorly washed hands of the mother or medical staff, or an insufficiently treated bottle. In infants on artificial feeding, infection with pathogenic Escherichia occurs if milk formulas are prepared in violation of technology. In addition to the general symptoms of dysbacteriosis (diarrhea, vomiting, bloating), fever and bloody streaks in the stool are added.
Atopic dermatitis, adaptation disorders and intestinal dysbiosis
Atopic dermatitis (AD) is a chronic recurrent inflammatory skin disease manifested by intense itching, sympathetic skin reaction, papular rashes and severe lichenification in combination with other signs of atopy. AD usually occurs in early childhood, has age-related localization features, and is characterized by hypersensitivity to both allergens and nonspecific irritants. Blood pressure significantly affects the quality of life, can cause sleep disturbances, decreased activity, neurotic conditions and lead to the formation of bronchial asthma and, accordingly, disability [1, 9].
Among the etiological factors leading to the development of AD, sensitization to food allergens is indicated, especially in childhood. This is due to congenital and acquired dysfunctions of the digestive tract, improper feeding, early introduction of highly allergenic foods into the diet, intestinal dysbiosis, the presence of a high titer of opportunistic pathogenic flora (OPF), disruption of the cytoprotective barrier, etc., which contributes to the penetration of antigens from food gruel through the mucous membrane into the internal environment of the body and the formation of sensitization to food products [6, 7, 10].
Most allergic problems are related to the gastrointestinal (GI) tract to one degree or another. This especially applies to allergic dermatoses, including AD. More than 90% of all antigens with which a person comes into contact are constantly present or in transit in the intestine - this is where the main elements of antiallergic protection are located, and the intestinal wall contains a huge number of immunocompetent cells, which allows some researchers to consider the intestine one of the key organs of the immune system. If any disturbances occur in the barrier function of the gastrointestinal tract, various toxins and antigens that become allergens begin to enter the blood from the intestines.
Allergens can be waste products of opportunistic flora [4] and parasites living in the intestinal lumen, as well as food that has not undergone sufficient breakdown. They sensitize the patient’s body, promote the production of specific IgE antibodies and the subsequent release of histamine from mast cells, which determines the clinical picture of food allergy. As you know, the environment is abundantly populated by microorganisms. Many of them are not capable of coexistence with a macroorganism, others are saprophytes, and others are symbionts, i.e., organisms capable of coexisting with other biological species in an interconnected and mutually beneficial interaction. Symbionts are necessary for the normal functioning of the host organism.
Under normal physiological conditions, the human body contains hundreds of different types of microorganisms. The term “normal microflora” unites microorganisms isolated from the body of a healthy person: from the skin, mucous membranes of the upper respiratory tract, gastrointestinal tract and genitourinary system. The lower sections of the small and especially large intestines represent a reservoir of bacteria throughout the body.
Normal flora is considered to be a set of microorganism associations typical for a certain biological species, the natural life activity of which occurs in those organs and tissues of the macroorganism that communicate with the external environment. Normoflora performs the most important physiological and immunological functions in the macroorganism and forms a single whole with it.
The total number of intestinal bacteria reaches 1014 cells, which is almost an order of magnitude greater than the number of cells of all organs and tissues of the macroorganism. It has been shown that the natural form of existence of any microorganisms in nature is an immobilized state, i.e. 99.9% of bacteria in nature live in the form of microcolonies fixed to various surfaces [12].
Attachment of microbial cells to solid surfaces occurs in three stages: in the first stage, reversible adhesion occurs due to weak interactions; the second stage consists of nonspecific adhesion with the help of fimbriae and pili, including the formation of hydrogen and ionic bonds; at the third stage, the formation of adhesion-enhancing extracellular material (polysaccharides) occurs. Thus, a biofilm is formed, through which contact is made between the intestinal lumen and the mucous membrane.
The biofilm covering the intestinal mucosa, in addition to polysaccharides of microbial origin, consists of colonies of microorganisms, as well as mucin produced by goblet cells. Microorganisms in a biofilm are tens and hundreds of times more resistant to adverse factors compared to when they are in a free-floating state [12]. Unlike free-living bacteria, representatives of normal flora in the animal body are able to attach only to certain receptors of the skin and mucous membranes. The most numerous and diverse group of bacteria is the thick mucosal layer covering the inner surface of the digestive tract. The normal flora of the gastrointestinal tract for humans are bifidobacteria, lactobacilli and Escherichia coli with normal enzymatic activity. As part of a biofilm, these types of bacteria should normally constitute up to 99% of all intestinal microflora.
In addition to normal flora, saprophytic and opportunistic flora may be present in the human intestine. Saprophytic flora is represented by epidermal and saprophytic staphylococci, enterococci, yeast, neisseria and other types of bacteria. Intestinal UPF can be represented by hemolytic streptococci, Staphylococcus aureus, spore-forming anaerobes, lactose-negative enterobacteria, hemolyzing Escherichia coli, and Candida fungi. Normally, the amount of UPF should not exceed 103–106 CFU per 1 g of feces, or 10% of the total number of microbes [5].
The normal flora of the intestine is involved in many vital processes of the macroorganism, which, in turn, is its habitat.
Diagnosis and treatment of dysbiosis in infants
If an intestinal disorder is suspected in children, stool tests are taken for dysbacteriosis and coprogram. It is better to collect material for analysis from a diaper, rather than from a diaper.
If tests show that lactose-negative E. coli is elevated in an infant, but his condition is normal, treatment is not carried out. In some cases, the doctor prescribes probiotics, such as Bifidumbacterin, and prebiotics, such as Hilak-Forte, Duphalac.
If the condition of a child under one year of age is serious, he must be hospitalized. The hospital provides complex therapy aimed at preventing dehydration (young children are given IVs with rehydration solutions) and reducing E. coli levels.
If there is excessive proliferation of E. coli and the child develops meningitis or other severe complications, treatment is carried out with antibiotics.
In cases where pathogenic E. coli are detected in the feces of a baby, treatment is mandatory. It is carried out with antibiotics, rehydration solutions, probiotics and prebiotics.
Dysbacteriosis in children over one year old
It is believed that in children over 1 year of age, intestinal dysfunction occurs for the same reasons as in adults. E. coli lactose-negative levels are elevated in a child in the following cases:
- very weak immunity;
- long-term use of antibiotics, especially if treatment with these drugs is carried out on the initiative of the parents, and not as prescribed by the doctor.
Symptoms of dysbiosis in children older than one year are the same as in infants:
- stomach ache;
- loose stools more than 2 times a day;
- rumbling in the intestinal area;
- flatulence;
- vomit;
- general malaise.
In rare cases, dysbiosis is accompanied by constipation or alternating constipation and diarrhea.
The same instability of defecation is observed if E. coli lactose-negative is reduced. If the analysis reveals the number of these bacteria is below normal, this may indicate the presence of worms.
In addition, children over one year old may be infected with dangerous E. coli: enterotoxigenic (attaches to the intestinal walls and releases toxins that cause diarrhea), enteroinvasive (causes symptoms similar to shingellosis and dysentery), enterohemorrhagic (diarrhea with blood streaks, pain in the abdomen have a sharp cramping character).
Infection with these species of E. coli leads to:
- eating unwashed or contaminated foods, especially fermented milk;
- any physical contact with a sick child or adult (for example, playing together, which is why outbreaks of dysbacteriosis are often recorded in kindergartens and nurseries);
- use of objects contaminated with E. coli (toys, dishes).
The causes of this pathology
The causes of elevated lactose-negative bacteria manifest themselves in almost the same way. Bacteriosis forms after the use of antibiotics that destroy harmful microorganisms and intestinal flora.
Failure to comply with personal hygiene measures leads to infection of a healthy person with pathogenic organisms through the oral route. Personal contact between a sick and healthy person is not necessary. An infected individual leaves bacteria on door handles, dishes, and railings.
Pathogenic microflora enters the body with unprocessed meat, dirty fruits, milk, eggs, and vegetables.
Diagnosis and treatment of dysbiosis in children
If a child has diarrhea and other symptoms of gastrointestinal dysfunction, it is necessary to undergo tests:
- coprogram;
- feces for dysbacteriosis.
Sometimes culture of urine and vomit is performed to check for the presence of E. coli in the material.
Enterohemorrhagic bacilli should be absent from the test results. E. coli lactose-negative in the feces of children over one year old and adults should remain within 10*5 CFU/g. In this case, in general, all opportunistic E. coli should be from 10*7 to 10*8 CFU/g. If this indicator is reduced to 10*6 CFU/g, grade I dysbiosis is diagnosed, and if it is increased to 10*9 CFU/g and higher, grade II dysbiosis is diagnosed.
Treatment for elevated lactose-negative E. coli is based on a strict diet. It includes porridges cooked in water without oil, slimy soups (rice, oatmeal), boiled fish, vegetables, meat, as well as crackers, bagels, and black bread. To avoid dehydration, the child is given frequent drinks (clean water, teas with chamomile, yarrow), jelly made from apples, black currants, and dried fruit compotes. For very frequent diarrhea, give solutions of “Regidron”, “Glucosolan” to drink, or prepare your own solutions from clean water to which sugar, salt and soda are added in proportions of 2:1:1. The therapy complex also includes enterosorbents “Polysorb” and “Smecta”.
If dysbacteriosis is accompanied by a temperature of 38 °C or more, antipyretic drugs are prescribed.
If treatment does not bring results on the 4th day, the patient is prescribed antibiotics. Ciprofloxacin and Amoxicillin are considered effective.
After recovery, patients must take a course of probiotics “Bifidumbacterin”, “Linex”, “Bifikol” and others.
E. coli in women
If in women E. coli lactose-negative is increased in the feces, dysbacteriosis of the second degree is diagnosed. They can call him:
- severe diseases of any etiology, leading to decreased immunity;
- uncontrolled or prolonged use of antibiotics.
Entry into the intestines of other pathogenic E. coli is possible in the following situations:
- consumption of poor quality water and food;
- physical contact (for example, shaking hands) with a carrier of the bacteria;
- lack of hygiene;
- using household items that contain E. coli (it should be noted that they are very tenacious in the external environment and can exist for a long time in the soil, in food and in water).
In most cases, the disease goes away without taking antibiotics. Treatment methods:
- strict diet;
- drinking plenty of water;
- taking enterosorbents.
It is much more dangerous if lactose-negative E. coli is found in the urine or vagina, because normally they should not be there. Bacteria enter an unusual environment due to improper hygiene or lack thereof (without regular washing, E. coli that come out of the colon with feces remain on the body and penetrate the vagina), when wearing tight underwear, especially thongs, during unprotected sexual intercourse with a carrier bacteria.
If lactose-negative E. coli is found in the vagina, how to treat such a disease? And is it necessary to do this if the woman does not feel discomfort? E. coli, once in the genitals, can move from there to the urethra, bladder, ovaries, and uterus. They are not washed out by a stream of urine and almost always cause inflammation, which without proper treatment becomes chronic. That is, the woman becomes a carrier of E. coli. In this case, there may be no obvious symptoms, only vaginal discharge with a characteristic unpleasant odor and some discomfort during sexual intercourse are observed. Hypothermia, stress, poor nutrition, or any disease can trigger the transition from a chronic to an acute form, so if the analysis shows the presence of lactose-negative E. coli in the vagina, treatment is mandatory. The course of therapy includes taking antibiotics and restoratives. In a month you need to repeat the analysis. If the rod is again detected in the smear or urine, a second course is prescribed, but with other antibiotics.
E. coli in pregnant women
As noted above, lactose-negative E. coli (Escherichia coli) is present in the gastrointestinal tract of all people, without causing any problems. In women during pregnancy, the immune system is weakened, which often leads to the number of Escherichia being outside the normal range. At the same time, the woman herself may not feel any discomfort, and changes in the microflora of her intestines are detected only by test results.
It is much worse when a pregnant woman experiences the following symptoms of dysbiosis:
- diarrhea;
- vomit;
- constipation;
- heartburn;
- flatulence.
Frequent bowel movements and vomiting lead to dehydration, which negatively affects the development of the baby in the womb. In addition, if there are too many bacteria, the pregnant woman’s body becomes intoxicated with their waste products. Also, diarrhea is fraught with increased uterine tone, which threatens premature birth. Constipation is unfavorable for all people (and especially for pregnant women) because unnecessary substances found in the stool are not eliminated from the body, but enter back into the blood.
Treatment of lactose-negative E. coli in pregnant women is carried out according to the general scheme:
- strict diet;
- taking rehydrants;
- drinking teas, jelly, dried fruit decoctions;
- taking enterosorbents.
If E. coli is found in the urine or in a smear taken from the vagina of a pregnant woman, it is necessary to take immediate action, as this is fraught with the development of colpitis, as well as infection of the baby during childbirth. Therefore, a pregnant woman must be prescribed a course of antibiotic treatment. "Amoxiclav" can be used at any period, "Cefotaxime" - only after the 27th week, "Cefipime" and "Ceftriaxone" - only after the 13th week, "Furagin" - only until the 38th week.
E. coli in men
Are lactose-negative E coli elevated in the stool of an adult male? If the indicators differ from the norm, this indicates dysbacteriosis. The causes of its occurrence, symptoms and treatment methods are the same as for women. The entry of intestinal bacteria into the urethra of the male genital organ causes urethritis, which can occur in an acute form (with severe pain when urinating) for only one or two days, and then become chronic without treatment.
Bacteria from the urethra migrate to the genitals and provoke diseases such as prostatitis, orchitis (inflammation of the testicles), epididymitis (inflammation of the testicular appendages). The disease will transition from chronic to acute due to hypothermia, stress, or any situations that lead to a decrease in immunity. Therefore, treatment (there should not be lactose-negative E. coli in the genitourinary organs of a man!) is mandatory. It is carried out according to the same scheme as for women.