Loose stools, or diarrhea in common parlance, is a digestive disorder that occurs quite often in both infants and schoolchildren - in children of any age. Many parents believe that the appearance of unnoticeable mucus in a small amount in the child’s stool is the norm. What can lead to diarrhea and when to sound the alarm, we will consider further. The main cause of this condition is the ingestion of substances from food that irritate the gastrointestinal tract or are intolerable to the child. There are few options for children under 12 months: such substances can get into breast milk, formula, drinks (water, baby tea, etc.) or complementary foods. In breastfed babies, diarrhea is a rare occurrence, but in formula-fed babies and children at the stage of introducing complementary foods, it is quite common.
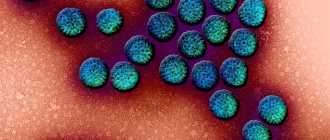
The second common cause of diarrhea is infection: viruses, bacteria and fungi can enter the child’s body with food, water, as well as through contact and household contact, through the dirty hands of the mother or baby, if basic hygiene rules are not followed.
Errors in nutrition are the third cause of diarrhea. Early introduction of complementary foods, overload of the digestive tract (especially the introduction of several new products at once), exceeding the frequency of meals - all this leads to the fact that the gastrointestinal tract cannot cope and dysfunction occurs, which is manifested by diarrhea.
Causes of loose stools with mucus in children
Many parents believe that the appearance of unnoticeable mucus in a small amount in the child’s stool is the norm. And even if a child has diarrhea with mucus (reasons), this is not yet a clear sign of the disease. However, mucus is always a sign of irritable bowel: normally there should be no mucus in the stool! In children under two years of age, this happens much more often than in older children, since the intestines of children are more sensitive to bacteria and microorganisms that enter the gastrointestinal tract.
Most often, loose stool in a child is caused by the following reasons:
- eating disorder
- high content of vegetables and fruits in the diet
- diarrhea in baby during teething
- colds
- taking antipyretics
- simple overexcitement
- climate change.
This is not dangerous and in most cases this disorder goes away on its own. With loose stools, the child’s general condition does not suffer greatly from these reasons.
Also, mucus in a baby’s stool may appear due to non-sterility of breast milk. Then it is better for the baby’s mother to take the appropriate test in a paid laboratory and reconsider her diet. More serious reasons include:
- overeating (see how to properly introduce complementary foods to children)
- enterocolitis
- intolerance to cow's milk, gluten (see is it possible to give cow's milk to children under one year old)
- gastroenteritis
- lactase deficiency
- helminthic infestation
- poisoning
- dysbiosis.
Prevention of loose stools in a newborn
To avoid this problem, it is worth carefully selecting the mother’s diet, feeding the baby in sufficient quantities - moderately, in accordance with its needs, introducing complementary foods in a timely manner (no earlier than 6 months), starting with “delicate” foods, massaging the belly clockwise to improve peristalsis and avoid dyspeptic symptoms.
Thus, it is fair to say that diarrhea with mucus in a child can be both a normal variant and a pathology. The accompanying symptoms are of decisive importance, by which you can understand whether your baby’s condition is physiological or whether it is worth seeing a doctor.
How to understand that loose stools are diarrhea (diarrhea)
First, let's talk about norms.
- In a breastfed baby, stool can accompany each feeding, up to 8 times a day.
- When bottle-fed, babies have stools less often, up to 4 times a day.
- After the introduction of complementary foods, the frequency of bowel movements approximately equalizes, both in children who are still fed breast milk and in babies receiving formula, more often - up to 3 times a day.
When breastfeeding, stool can be either liquid or mushy; the consistency and shade of stool depend on what is present in the nursing mother’s diet; the smell is somewhat similar to the smell of kefir.
Thus, watery stool with a greenish tint in a baby feeding at the breast, with lumps of undigested milk, is the norm, but only if the baby feels well, is gaining weight and behaves normally!
The stool of a child fed formula is denser, almost always the same color and characteristic smell.
What then is considered diarrhea? Defecation, the appearance, smell and quantity of which is not included in the usual number of bowel movements per day. But you need to remember that all children are different and you cannot compare them with each other - the loose stool that we see in a photo posted by some mom on the forum is not necessarily a model that we should emulate!
There are so-called diagnostic criteria that allow you to identify diarrhea from normal stool:
- bowel movements have increased significantly, at least twice as often;
- the stool has become watery;
- stool contains unusual impurities;
- the color of feces has changed with a normal diet, including discoloration;
- the child is restless, eats and sleeps poorly, knocks his legs;
- there is increased gas formation;
- an unpleasant odor emanates from stool;
- Irritation and redness appeared around the anus.
Attention! You need to inform your pediatrician about every case of increased stool frequency, the appearance of atypical or more frequent bowel movements than usual! For children under one year old, this is mandatory - you need to call a doctor at home!
Aggravating circumstances include:
- foamy or watery stools that have lost their fecal character (wet spots on a diaper or diaper)
- blood in loose stools
- copious mucus in the stool.
But the situation becomes more serious if the child’s diarrhea is caused by an intestinal infection or appears during or after taking antibiotics (dysbacteriosis). It is necessary to urgently call a doctor if your child develops:
- watery stools with mucus more than 6 times a day
- feces with a strong foul odor
- green diarrhea in infants or diarrhea in the form of orange flakes
- high fever combined with diarrhea
- stool in the form of raspberry jelly or blood in liquid stool,
- diarrhea combined with regurgitation (especially fountain),
- concomitant serious condition - the child is lethargic, refuses food and food, urination is rare or absent.
In addition, if a baby has loose stools combined with frequent regurgitation, the baby has poor weight gain - this indicates serious health problems. A doctor will help determine the cause of loose stools in a baby by sending him for the appropriate tests - coprogram, general blood test, stool test for dysbacteriosis. Diarrhea in children after antibiotics is almost always caused by intestinal dysbiosis. Therefore, any use of antibacterial agents is recommended to be accompanied by means to maintain the normal microflora of the baby according to age and the recommendations of the pediatrician (see).
| Feces with colienteritis | Putrid feces with one-sided protein feeding | Hungry stool | Meconium |
| Dysentery feces | Feces for nutritional dyspepsia | Acholic feces in biliary atresia | Mesose-like homogeneous feces (for breastfeeding) |
| Feces with intestinal infantilism | Feces for nutritional dyspepsia | Stool for neonatal melena | Feces of a baby fed cow's milk |
Treatment
It is necessary to understand that the liquid consistency of a baby’s stool in itself is not yet a pathology, because, basically, a child at this age drinks mother’s milk or diluted formula. The presence of mucus can also be physiological, so parents should carefully monitor the child’s well-being, his mood, the amount and frequency of urination, weight gain and appetite. If these indicators are normal, there is no need to worry. However, if you notice negative dynamics, it is worth starting treatment:
- Diarrhea with mucus in a child can lead to dehydration, so you need to give him plenty of liquid: still mineral water, unsweetened dried fruit compote (it contains substances that improve peristalsis), chamomile tea, which has anti-inflammatory, anti-allergenic and carminative effects;
- Use enterosorbents - drugs that adsorb toxins on their surface. These include: Polysorb, Smecta, White Coal (preferably in a suspension, which is prepared by adding boiled water to a 250 ml bottle of powder, and then vigorously shaking). Such drugs are prescribed for suspected acute intestinal infection;
- Electrolyte solutions will help avoid the loss of microelements and maintain water-salt balance. For infants with diarrhea of any etiology, it is recommended to use Humana Electrolyte - a hypoosmolar mixture that stimulates the replenishment of missing fluid and has a pleasant taste (fennel or banana), which is important when consumed by children, as well as Regidron, which is effective against increased acetone, rotavirus infection and dehydration of any origin;
- If diarrhea is caused by an allergic reaction, it is appropriate to stop the child’s contact with the likely irritant and take antihistamines, for example, Tavegil (available in suspension for children up to one year old) or Fenestil (drops for oral administration);
- In case of dysbiosis, it is important to give preference to adapted formulas (if the baby is bottle-fed) and not to forget about prebiotics that help maintain normal microflora in the large intestine: Linex, Bifiform-Malysh, Acipol, etc.;
A consultation with a pediatrician is required, before which the child must stop eating so that the doctor can adequately assess the quality of stool.
Tests needed to determine the cause of diarrhea in children
A complete blood count will help determine the “severity” of the infection. That is, how strong the inflammatory process is in the baby’s body. Based on the test result, the doctor will prescribe treatment.
- Coprogram
The coprogram can establish the presence of disturbances in the functioning of enzymatic systems, shows the functioning of the pancreas and helps to recognize the location of dysfunction in the digestive system, the severity of the inflammatory process, and pathological processes in the gastrointestinal tract. In an acute situation with diarrhea, it is almost always useless.
- Bacteriological analysis of stool + test for dysbacteriosis
It will help determine which pathogenic microorganisms are causing the baby’s digestive upset. This way you can identify Staphylococcus aureus, Klebsiella, Enterococcus, Proteus. In the same analysis, colonies of bifidum and lactobacilli are considered, which, as a rule, are very few in diarrhea in children. The analysis also allows us to establish a quantitative indicator of beneficial bacteria in the baby’s intestines. The disadvantage of this analysis is that it is completed within 5-10 business days and most often it will have to be done for a fee.
- A stool test for worm eggs and protozoa is necessary, as some helminthic infestations can cause periodic diarrhea in a child.
- Stool culture for typhoid-paratyphoid and dysentery group allows us to freely identify or refute these variants of infection.
- In the direction of the pediatrician, stool can be cultured for a specific suspected pathogen: staphylococci, rotaviruses.
infant diarrhea with mucus
A runny nose is one of the problems that parents of young children often face. What do you need to know about this condition in order to effectively help your baby and not miss the development of serious complications?
The younger the child, the more discomfort he experiences when he has a runny nose. However, treating this disease is not easy. It is impossible not to treat a runny nose at all: it can be complicated by other diseases, for example, inflammation of the ear - otitis media. At the same time, too active and excessive treatment can lead to disruption of the nose and make it difficult for the child to breathe through the nose. Therefore, it is important to know how to help your baby correctly and quickly.
Important organ The nasal mucosa is lined with ciliated epithelium: the cilia make oscillatory movements and attach dust particles, viruses, and microbes to themselves. And the mucus secreted by the cells has a disinfecting effect. The nasal cavity has an abundant blood supply; the walls of the turbinates are intertwined with a network of vessels. This structure of the nose allows you to warm the inhaled air and clean it of dust and germs, so nasal breathing is very important for children. When breathing through the mouth, the defense weakens and the likelihood of getting sick increases. In addition, the nose is a powerful reflexogenic and perceptive zone; there are many sensitive, olfactory and nerve endings. It is closely connected with the work of many organs and systems, so it is important that the baby’s nose always works properly.
Features of a runny nose in infants
A runny nose, or rhinitis (from the Greek word rhinos - nose + itis - meaning inflammation) is an acute or chronic inflammation of the nasal mucosa, which occurs both as an independent disease and as a symptom of many colds and non-infectious diseases. If for adults a runny nose, although unpleasant, is most often not dangerous, then for children it is by no means a harmless problem. Rhinitis in children occurs differently than in older children or adults.
It is especially difficult for infants and children of the first years of life. Firstly, they do not know how to blow their nose to remove mucus buildup and make breathing easier. Secondly, babies have very narrow nasal passages, and due to the abundant blood supply, any irritation causes severe swelling, which aggravates the difficulty breathing through the nose. Thirdly, the nasal cavity in an infant has a small volume, so it quickly becomes clogged with mucus, practically eliminating breathing through the nose, and this, in turn, does not make it possible to suck the breast or bottle normally, which leads to refusal to eat. Fourthly, disruption of the normal outflow of mucus leads to stagnation and proliferation of microbes, to inflammation and its spread to the ears or throat. In addition, the baby’s immunity is still incomplete, so the infection activates quite quickly, causing a general reaction of the body - fever, intoxication, lethargy.
However, in young children, unlike adults, there are also physiological, “dental” and false rhinitis , which develops with excessive salivation.
Physiological runny nose
Parents often notice a “squelching” sound in their baby’s nose during the first 2-3 months. Most often, it’s not a matter of a cold, but a matter of physiology. In babies, the nasal mucosa begins to adapt to a new regime, because before birth the baby’s habitat was water, and after birth it was air. By about 10-12 weeks of life, the mucous membranes of the nose and pharynx are adjusted to full function. Until this moment, the body tests the condition of the nasal mucosa - either dries it out, which may not be noticeable due to the child’s condition, or overly moisturizes it, which is manifested by nasal discharge. Usually, parents mistake these very phenomena for a cold and intensively treat them, although in fact this is a normal stage in the development of the baby’s nose. No intervention is required here: the body knows that excess moisture is being released, it adjusts the regulation mechanism. If you intervene and remove moisture, the body will increase its production, “deciding” that since the moisture is disappearing, then it is needed in an even greater volume. Thus, intervention can turn the physiological state of mucosal tuning into a problem.
If, apart from nasal discharge, there are no other symptoms, and the baby is under 2-3 months old, do not rush to drip drops - most likely, this is a physiological runny nose, it does not interfere with the baby’s life, mostly disturbing only the parents. In this case, it is optimal to maintain a cool temperature in the room - about 20-22 ° C - and a humidity of 50-70%, then the mucous membranes of the nose will not dry out, and its function will be restored by itself. You can instill salt solutions into your baby in the morning and at night, for example AQUAMARIS, AQUALOR, SALIN or pharmaceutical saline solution: they soften and moisturize the nasal mucous membranes. No additional procedures are required.
Also, infants have special conditions that do not occur in older children and adults. At about 3 months, with the beginning of the oral stage of exploring the world, when the baby puts everything in his mouth, increased salivation appears. In this case, episodes of “grunting” may occur, which is caused by the accumulation of mucus and saliva in the nasopharynx when the baby is lying down. This blockage of the posterior nasal passages causes nasal congestion. A slight leakage from the nose can occur when regurgitating: if part of the food gets into the nasal passages, in order to protect itself from aggressive stomach juices, mucus is intensely released, which neutralizes the acid, which is why a runny nose occurs. This is not dangerous to the baby's health.
Let us especially focus on the so-called “dental runny nose” . Sometimes, especially when the upper teeth erupt, due to irritation of the trigeminal nerve branch, excessive mucus secretion occurs and a runny nose occurs. However, it is not accompanied by any other symptoms. If there is a cough, fever, or stool problems, this is not a “runny nose,” but an infection that requires examination by a doctor.
Runny nose as a disease
Acute rhinitis, or runny nose, is the most common disease of children in the first years of life, including infants. Very often parents are interested: why, if breastfeeding protects the baby from diseases, does he still have a runny nose? In fact, breast milk does not ensure the complete absence of diseases, but their adequate and rapid progression. Therefore, a runny nose in a baby occurs much less frequently, is easier and goes away faster.
The urban environment and the presence of a large number of adults and children in the house provide frequent contact with viruses and germs and a greater likelihood of developing infection. However, an indicator of the active functioning of the immune system is a runny nose, which occurs without complications, fever and passes in 3-5 days: it trains the work of all levels of the body’s defense.
The causes of a runny nose can be infectious agents, i.e. viruses or microbes. The first place in frequency is occupied by viruses that cause various types of acute respiratory viral infections, the second place is occupied by microbes. Normally, the cilia of the nasal epithelium vibrate, capturing foreign particles, dust and microbes, neutralizing them and removing them from the body. When an infectious agent enters the nasal mucosa with inhaled air, it settles on the ciliated epithelial cells, paralyzing their work. There it begins to reproduce. This period, depending on the type of disease, lasts from 12 hours to 2-3 days. Infectious particles damage the epithelium, and it becomes swollen, and the walls of blood vessels become more permeable, hence the appearance of mucus. This condition is favorable for the addition of a bacterial infection, i.e. inflammation caused by microbes, which complicates the course of the disease.
Most often, a runny nose occurs during sudden changes in temperature: this changes both the infectivity of microbes and the body’s resistance. The risk of the disease increases when the baby’s legs are cooled, since the legs have direct reflex connections with the nasal cavity: when they are cooled, the active protection in the nose decreases.
Stages of a runny nose
During acute rhinitis, three sequential stages are distinguished. At the first stage, when the inflammatory agent penetrates the mucous membranes, dryness and tension in the nose, congestion and a feeling of swelling, and itching are observed. In babies, this is usually characterized by frequent sneezing. Then this stage smoothly passes into the second - wet. The nose becomes very stuffy, nasal breathing becomes difficult, copious transparent watery discharge appears - the nose “runs”. Swelling of the mucous membranes of all three nasal conchas occurs, mucus accumulates in the nasal passages - then, due to difficulty in nasal breathing, the baby begins to breathe through the mouth. For a baby at this stage, sucking on a breast or bottle becomes almost impossible; the child often stops sucking, gets tired, and breathes through his mouth. After 1-2 days, the process enters the stage of suppuration: the mucus becomes yellowish or greenish in color due to the accumulation of killed microbes and viruses absorbed by immune cells; in fact it is the same pus. Swelling of the mucous membranes decreases, nasal breathing improves, nasal discharge becomes viscous, mucopurulent in nature, as they usually say, “with greens.” Gradually the volume of discharge decreases. The whole process proceeds sequentially and is completed within about 7-10 days, sometimes some stages may be short or absent.
Special situations
If a child is weakened and has frequent runny noses, this indicates chronic rhinitis, which occurs in several forms. With constant discharge of mucous or mucopurulent nature, difficulty in nasal breathing, half or the entire nose is congested, they speak of chronic catarrhal, or simple, rhinitis.
The hypertrophic form of rhinitis is characterized by a decrease in the sense of smell, hearing, and nasal sound of pronounced sounds. This usually happens with an allergic cause of a runny nose. In addition, smoking in the family, especially with a child, and allergens at home - animals, birds, fish food, feather pillows, mold, dust or carpet mites - contribute to a runny nose.
The causes of a runny nose in children can also be injuries to the mucous membrane; foreign bodies, such as balls, beads, berry seeds, that are stuck in the nasal cavity; exposure to strong odors, environmental factors - dust, smoke, varnishes, paints, poplar fluff. Irritation of the mucous membrane by these factors is a favorable environment for the attachment of microbes and inflammation.
Why is a runny nose dangerous?
A runny nose is most dangerous for children in the first year of life, since it rarely occurs in isolation; it is usually accompanied by inflammation of the pharynx - pharyngitis, inflammation of the ear - otitis media, inflammation of the sinuses - sinusitis, inflammation of the tonsils - tonsillitis or other diseases. This occurs due to the addition of a secondary infection or activation of one’s own opportunistic microflora in the oral and nasal cavity. In addition, in babies, a runny nose disrupts normal sucking, which leads to impaired weight gain or even weight loss due to refusal to eat. Significant discomfort is caused to children by irritation and ulceration of the area around the nose due to the constant flow of mucus: children rub their faces, causing infection. The crusts itch or sting, causing discomfort to the child; in this case, the baby refuses to wipe or clean his nose.
When should you see a doctor?
You need to know that a runny nose is a protective mechanism against the development of infection, since when mucus drains, harmful microbes and viruses are removed. Therefore, a short and uncomplicated runny nose does not require intensive treatment - you can cope with it on your own. However, a prolonged runny nose or complications can be dangerous for the baby, so you need to know when to seek help from a doctor, especially if we are talking about a baby in the first year of life.
Consultation with a doctor is required in the following situations:
• with a runny nose, the temperature rises to 38°C and above, the disease is accompanied by pallor, regurgitation, diarrhea;
• along with a runny nose, redness of the throat and shortness of breath appear;
• for a baby under 2-3 months of age, a runny nose prevents him from sucking,
• sleep; • the baby abandons or does not take the breast;
• runny nose lasts more than 2 weeks;
• the disease is accompanied by pain in the face and headache (when pressure is applied to the eyebrows, the child screams sharply under the eyes), the baby is lethargic or excited, blue discoloration is visible around the mouth;
• there is abundant purulent discharge from the nose with an unpleasant odor;
• nosebleeds occurred due to a runny nose;
• a runny nose appears after contact with animals, pollen, or contact with chemicals.
Treatment
First of all, before starting any therapeutic measures, it is necessary to alleviate the baby’s condition using available non-drug means. Sometimes this is enough, and the runny nose quickly goes away on its own. To sleep, raise the head of the child's bed to about 40-45°, thanks to this the mucus that accumulates in the nose will be easier for the baby to secrete or swallow.
Ventilate the apartment often, do wet cleaning, humidify the air: it’s easier to breathe with cool, moist air. Offer your child to drink little by little and feed him according to his appetite. If the baby refuses to suck or cannot do so because of mucus in the nose, it is necessary to toilet the nasal passages. To do this, prepare wicks rolled from cotton wool; There is no need to use chopsticks, as the child may jerk sharply and get injured. Drop 2-3 drops of saline solution into each nasal passage: AQUAMARIS drops, AQUALOR, SALIN, physiological is required if the temperature rises to 38°C or higher during a runny nose. Pharmaceutical solution - or chamomile decoction. Then, using a twisting motion, clean the baby’s nose with a twisted wick, removing mucus and soggy crusts. You can remove mucus with a small rubber bulb by carefully inserting its tip into the nasal passage, pressing the second wing of the nose against the septum. In addition, there are special pharmacy systems for cleaning the nose of infants - aspirators. This is usually a thin tube connected to a soft rubber or plastic balloon.
You should not use oil to soften crusts: it disrupts the normal functioning of the epithelial cilia and can cause swelling and allergies. If there is swelling in the nose or mucus is released very abundantly, disturbing the child, you can use vasoconstrictors, but these should be special children's drops with reduced dosages of medications.
The main ones in childhood are CHILDREN'S NAZIVIN, VIBROCIL, OTRIVIN BABY, CHILDREN'S NAZOL. For children under 3 years of age, it is allowed to use only drops, since sprays can provoke laryngeal spasms; from 3 years of age, the use of nasal sprays is permissible. Do not overuse drops or sprays, exceed the dosage or use them for more than 3-4 days. Before the doctor arrives, you can use regular saline or baby drops so that the child can eat. In addition, you must remember that vasoconstrictor drops act on the mucous membrane, which means they will help if they are used only after thoroughly cleansing the nose, otherwise, due to the abundance of mucus, they simply will not reach the site of their action. To use the drops, you need to warm them up a little in a water bath or in your palms. Place the baby on a flat surface, tilt his head up a little, drop 1-2 drops of the solution into the nasal passage and immediately tilt his head down, pressing the nostril to the nasal septum. Then the drops will not be swallowed and will be evenly distributed throughout the mucous membrane. Repeat the same with the other half of the nose.
When bacterial inflammation occurs, antibacterial drops are used as prescribed by a doctor, for example SODIUM SULFACYL, or ointments - BACTROBAN. DERINAT drops can be used to stimulate local immunity; when used in the first hours of illness, a runny nose can be prevented or its course halved. Homeopathic remedies such as EUPHORBIUM COMPOSITUM and OCARIZALIA are also successfully used to treat the runny nose.
What not to do when you have a runny nose
There are activities that should not be carried out during a runny nose, especially in children in the first three years of life.
• Do not rinse your child's nose with a syringe or rubber bulb: this can cause otitis media. The fact is that the nasopharynx cavity connects to the Eustachian tube of the ear, and the tube itself is wide and short. When fluid is forced into the nose under pressure, infected fluid will be thrown into the ear cavity and inflammation will develop. However, this does not happen when instilled - then the liquid only enters the nose.
• It is unacceptable to drip antibiotic solutions into a child’s nose on your own.
• It is forbidden to use vasoconstrictor drops constantly - their use is permissible only in case of severe congestion, before bedtime and for no more than 3-4 days. In addition, children under 3 years of age are prohibited from putting plant oils, aloe juice, Kalanchoe or vegetables, such as beets or carrots, into the nose, especially undiluted. The components they contain cause severe burns to the nasal mucosa.
• You should not put breast milk in your baby's nose, as it is a favorable environment for the growth of bacteria.
Prevention
A runny nose can be prevented by following hygiene measures: visit crowded places less during the cold season, wash your hands and face, irrigate the nasal mucosa with saline solutions after visiting crowded places - this washes away germs and viruses from the mucous membrane.
It is necessary to dress your child according to the weather and ensure that his feet are always warm and dry. The baby benefits from hardening activities, frequent walks in any weather, and proper nutrition.
How to treat diarrhea in an infant
Prolonged diarrhea in an infant is very dangerous; it leads to dehydration of the child's body in a very short time. What to give a child for diarrhea? First of all, it is necessary to restore the water-salt deficiency caused by diarrhea.
- The child should remain breastfed or bottle-fed. Give the breast as often as the baby asks, do not maintain the usual intervals!
- For formula-fed babies, it makes sense to slightly reduce the portions and feed the baby a little more often.
- If diarrhea in an infant is combined with frequent regurgitation (vomiting), there is no need to engage in amateur activities and treat it yourself. It is urgent to take the child to the hospital, where he will be given an IV, since infants become dehydrated much faster than adults.
- If it's just about diarrhea. You can try to fight dehydration on your own. In addition to the usual food (milk or formula), a child under one year old should drink the same amount per day that he approximately lost with the previous loose stool. Plus the volume of one feeding plus approximately 200 ml for each subsequent loose stool. They should be given special saline solutions (Regidron, Acesol, Oralit); pure baby water or sweet tea for children over one year of age are also suitable. If your baby drinks normally between feedings, give him water from a bottle, spoon, cup or syringe. If things get tough, give 1 teaspoon every 5 minutes.
- If nothing works out, don’t wait for complications and go to the hospital. Criteria for dehydration are drowsiness, dry lips, palms and soles, dull eyes, a poorly straightened fold on the tummy caught in the fingers, lethargy, and lack of urination.
The doctor may also prescribe treatment with Enterofuril, Stop-Diar in suspension, Furazolidone in tablets according to the instructions and dosage according to the child’s age (see symptoms of food poisoning, treatment of food poisoning, causes of diarrhea and vomiting in a child without fever, a complete list of all remedies for diarrhea) . Often, specific Klebsiella or staphylococcal diarrhea is treated with bacteriophages (intestibacteriophage, Staphylococcal, Klebsiella).
Diet for diarrhea in children
If an infant who is breastfed has diarrhea, the child recovers faster and they are less likely to have complications. It is necessary to combine breastfeeding with rehydration, breastfeed the baby more often and exclude vegetable complementary foods, juices, leaving cereals and meat.
For older children, a strict diet is necessary; indigestible foods, sweets, fatty foods, dairy products, salty foods, and foods rich in fiber are excluded from the diet. You can give crackers, tea, potatoes, bananas.
Author:
Selezneva Valentina Anatolyevna physician-therapist