Myths and truth about urticaria
Urticaria is a skin disease. It is characterized by rashes similar to nettle burns and itching of varying severity, often severe. If the rash lasts less than 6 weeks, it is acute urticaria. More than 6 weeks - chronic.
Myth .
Urticaria may be accompanied by poor health, fever, cough, headache, rashes in the mouth, swelling, joint pain, diarrhea, and vomiting. Is it true . Such symptoms may be a manifestation of a systemic allergic reaction (this may also include urticaria) or individual diseases.
Myth . Hives are an allergy.
Is it true . The disease is associated with the release of biologically active substances (transmitting signals from cell to cell) by immune (mast) cells of the skin under the influence of various reasons. One of the reasons may be allergies. In most cases, the manifestation of chronic urticaria occurs without an understandable external cause as a result of the action of autoantibodies (antibodies to the body's own proteins) on cell receptors.
Myth . Urticaria occurs due to the presence of chronic infection and bacterial allergies, worms, disturbances in the gastrointestinal tract, and the circulation of toxins in the body.
Is it true . The most common cause of acute urticaria is viral infections (ARVI).
Urticaria can occur when infected with worms, but there is no need to look for worms in all patients. Our region, according to WHO, is not endemic (infection with worms in central Russia occurs infrequently). Therefore, when urticaria manifests itself, it is logical to conduct an examination for worms after staying in regions with a high prevalence of helminthic infestations (Asia, Africa), in the presence of other symptoms and characteristic changes in a routine blood test.
It is assumed that infection of the gastrointestinal tract with H. pylori (a bacterium that causes stomach ulcers and erosions) may be important. The connection between urticaria and other diseases or functional disorders of the gastrointestinal tract has not been confirmed. Moreover, it makes no sense to search for and treat certain elusive and unmanifested conditions. The circulation of toxins in the body is a myth (there is no evidence), and accordingly, urticaria cannot occur for this reason. Chronic urticaria or so-called urticaria-like rashes (similar to hives) may indicate the occurrence of some serious common diseases.
Myth . If the patient has a high sensitivity of the body to allergens, then he may experience chronic recurrent urticaria. High sensitivity markers can be antibodies to Epstein-Barr viruses and cytomegalovirus.
Is it true . Allergic urticaria occurs acutely upon contact with a specific allergen. There are usually few such allergens for one patient. These can be foods (usually fish, nuts, eggs), insect bites. The detection of antibodies to viruses in the blood indicates that a person has had contact with the virus and has developed a protective reaction of the immune system. Antibodies to viruses are not related to allergies and do not affect the release of biologically active substances in urticaria.
Myth . If you have urticaria, it is necessary to conduct a comprehensive examination.
Is it true . In most cases, acute urticaria does not require examination. For chronic urticaria, specific studies are indicated, but not a complete examination of the body.
Myth . In acute cases of urticaria, it is necessary to go to the hospital, otherwise recovery will be delayed and complications will arise.
Is it true . Indications for hospitalization are severe urticaria, combination with edema, bronchospasm or other manifestations of anaphylaxis (severe allergic reaction), or a violation of the general condition.
Myth . If you have urticaria, you must follow a special hypoallergenic diet. In case of acute urticaria, it is forbidden to eat even food that was previously well accepted by the body. During an exacerbation, a person’s reaction to food is difficult to predict, so a gentle menu or even complete fasting is necessary.
Is it true . It is necessary to exclude only those foods to which a person has a proven allergy. The prescription of a diet for chronic urticaria is controversial. The benefit of a diet avoiding pseudoallergens or histamine-containing foods in the treatment of chronic urticaria has not been proven by research. Following such diets poses significant challenges and is not supported by most current clinical guidelines.
Myth . For urticaria, it is necessary to prescribe corticosteroid hormones in tablets or droppers.
Is it true . Indications for the use of corticosteroid hormones include severe urticaria, edema, bronchospasm, or other signs of anaphylaxis. This treatment will help relieve severe or life-threatening symptoms, but will not affect the further course of the hives.
Myth . It is necessary to cleanse the body with laxatives, enemas, sorbents, diuretics, hepatoprotectors and choleretic agents, use hyposensitizing drugs such as sodium thiosulfate and calcium gluconate, restore the microflora with probiotics and drink vitamins.
Is it true . All these drugs have no proven effectiveness; their effect is assumed to be through their influence on non-existent mechanisms. In accordance with modern recommendations, treatment should be aimed at reducing the release of biologically active substances, primarily histamine. The main group of drugs for the treatment of both acute and chronic urticaria are type I histamine receptor blockers (antihistamines), a combination of different drugs or an increase in dose is possible. If the effect of using antihistamines is insufficient, antileukotriene drugs and type II histamine receptor blockers are added to treatment. And in severe cases, antibodies to immunoglobulin E (omalizumab) or immunosuppressive therapy with cyclosporine.
All myths are quoted from the Russian-language Internet, although they are quoted from the international consensus document EAACI/GA2LEN/EDF/WAO and the Federal Clinical Guidelines of RODVK.
Author:
Vera Removna Voronina , dermatologist
Diagnosis of urticaria
Urticaria is diagnosed by a specialist (for example, a dermatologist): this is usually done during an examination based on the characteristic appearance of the rash. If the urticaria is acute, the patient, as a rule, does not need additional research: this type of disease usually goes away quickly on its own and does not subsequently return. If urticaria is chronic, it is important to determine its immediate cause in order to select the correct treatment. Laboratory diagnostics are used for this.
Laboratory tests necessary to diagnose urticaria:
- Clinical blood test;
- ESR;
- General urine analysis
- Fecal analysis for the presence of helminth eggs;
- Circulating immune complexes (CIC);
- Antibodies to double-stranded DNA;
- Antinuclear factor;
- C3 and C4 complement components;
- Culture of flora to determine sensitivity to antibiotics (various locations);
- Intestinal dysbiosis;
- AST;
- ALT;
- Serum urea and creatinine;
- Total bilirubin;
- T3 free;
- T4 free;
- AT-TG;
- AT- TPO;
- Total immunoglobulins E in serum.
Additional tests needed to diagnose urticaria:
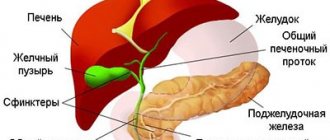
- Ultrasound of the thyroid gland (code 21331 and code 21344 for children) and ultrasound of the abdominal organs (code 21313 or code 21314);
- Skin biopsy;
In some cases, diagnosing urticaria may require consultation with a dermatovenerologist, gynecologist and other specialists.
Anamnesis
Given the ephemeral nature of urticaria rashes, it is extremely important to properly collect anamnesis. The doctor must understand whether it is urticaria, what provokes it and what mechanisms support it. Therefore, you should pay attention to the following points:
- description of the elements and associated sensations (itching, burning, pain);
- life expectancy of elements and the presence of secondary changes - hyperpigmentation, erosions, crusts, etc.;
- the cyclicity of the appearance of elements, the duration and frequency of the disease. For women, it is worth paying attention to the connection with the phases of the menstrual cycle;
- triggers, including medications, food intake, insect bites/stings, as well as physical factors and stress;
- previous therapy and its effectiveness;
- presence of allergic diseases in personal and family history;
- the presence of concomitant somatic pathology, including those associated with chronic urticaria, infectious diseases, autoimmune diseases, non-infectious chronic inflammatory diseases, especially involving the gastrointestinal tract, paraneoplasia;
- professional activity/hobby.
New trends
The effectiveness of treating urticaria with alternative groups of drugs is currently being studied. Among them: antidepressants, androgens, slow calcium channel blockers (nifedipine), M-anticholinergic blockers, sulfasalazine, methotrexate, colchicine.
The use of plasmapheresis and phototherapy in patients with solar urticaria is actively discussed. Separately, it is worth dwelling on the issue of the use of biological agents. The idea of binding and inactivating molecules involved in immune responses has always seemed extremely attractive in the search for a cure for hives. The appearance in practice of monoclonal antibodies (MAbs), which make it possible to solve this problem with high specificity and selectivity for target molecules, gave rise to a number of biomedical studies that studied the possibility of using MAbs for the treatment of immune-mediated diseases, including allergological diseases.
Currently, mAbs against immunoglobulin E, the drug omalizumab, are registered in Russia. The drug binds to IgE, blocks its interaction with receptors on mast cells, which prevents their subsequent degranulation; there is also a decrease in the number of IgE receptors on the surface of basophils. Omalizumab, originally used to treat severe atopic asthma, later showed its effectiveness in the treatment of chronic urticaria. However, scientists do not rest on this and continue to search for new biological agents to treat different types of urticaria.
Inspection
If a patient comes to an appointment with a rash, then it is necessary to understand how similar what he sees is to a urticarial rash. The presence of elements other than a blister, as well as atypical secondary elements - crusting, erosion, persistent hyperpigmentation - casts doubt on the diagnosis.
Also, during the examination, you should pay attention to the signs of atopic diseases and other somatic pathologies. If you suspect a connection between physical factors and the development of urticaria, provocative tests are informative. The doctor can apply streak stimulation with a spatula, apply heated or cooled objects, apply vibration sources, irradiate with light of different wavelengths, offer physical exercises and hang weights from the patient’s limbs, followed by assessment of the skin.
Treatment of urticaria
Typically, acute urticaria goes away on its own within a day and does not require treatment. You can reduce itching by taking antihistamines and using cold showers. Antihistamines can block the effect of histamine, the main substance that triggers the symptoms of hives. If it is determined that the nature of the urticaria is allergic, it is necessary to eliminate the effect of the allergen on the body as soon as possible.
Treatment of chronic urticaria is a much more difficult task. If the cause of the chronic rash has been established, it is necessary to treat the underlying disease. In many cases, a positive result can be achieved using individually formulated combinations of drugs. To treat chronic urticaria, specialists may use antihistamines, steroids (synthetic analogues of adrenal hormones), as well as certain types of antidepressants.