Amebiasis - symptoms and treatment
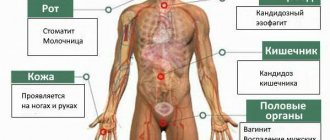
Amoebiasis (Amoebic Dysentery) is an acute and chronic disease that is caused by pathogenic strains of dysenteric amoeba. Penetrating into the body, they lead to ulcerative damage to the intestines, which is accompanied by moderate intoxication, stool disorders, weight loss and sometimes the appearance of abscesses in the liver, intestines, lungs and brain. The disease can last a long time, sometimes leading to death, especially in weakened patients and in the absence of medical care.
Pathogen
Taxonomy:
- domain - eukaryotes;
- branch - amoeba-like;
- type - Evosea;
- class - Archamoebae;
- family - Entamoebidae;
- genus - Entamoeba (entamoeba);
- species - dysentery amoeba (Entamoeba histolytica).
The Russian scientist F. A. Lesh was the first to describe the pathogen and prove its pathogenicity in 1875. At least 22 strains have now been isolated, of which 9 are pathogenic, and the remaining 13 are most likely not pathogenic for humans.
Changing during life, amoebas go through two stages of development:
- the vegetative, or active, stage in the form of a trophozoite ;
- a resting stage, or "dormant" stage, in the form of a cyst .
The vegetative stage divides amoebas according to function and structure into large vegetative, luminal and tissue. All of them, suddenly entering the external environment, die within 30 minutes.
Large vegetative trophozoites (forma magna) reach 20-60 microns. This form of amoebas moves due to forward thrusts. Contains the nucleus and cytoplasm - the main part of the cell. The cytoplasm is divided into a glassy transparent mass and an inner liquid layer with digestive vacuoles in which red blood cells captured by the amoeba are digested. In acute amoebiasis, large trophozoites are detected in fresh feces - “warm feces”. Capable of breaking down protein molecules. They have surface pectins, with the help of which amoebas attach to the intestinal mucosa.
The luminal vegetative trophozoites (forma minuta) are much smaller than the large form: they reach 15-20 microns. Such trophozoites are inactive. They have one core, which is not visible without coloring. Their cytoplasm contains small vacuoles, but without erytrophytes. Luminal trophozoites live in the upper part of the large intestine, feed on bacteria, reproduce, and do not cause obvious harm. They are detected in the feces of acute amoebiasis at the beginning of recovery, in chronic amoebiasis, as well as in amoeba carriers, but to identify them it is necessary to carry out deep intestinal lavages or examine the final portions of feces after taking a saline laxative. In the lower part of the large intestine, with a gradual deterioration of conditions, for example, lack of fluid, disruption of the bacterial flora, taking medications or changes in the pH of the environment, they usually transform into a cyst form, which is gradually released into the environment. If the body's defenses are weakened, luminal trophozoites can transform into a larger vegetative form and become aggressive.
Tissue vegetative trophozoites are formed from the luminal form, but are similar in appearance to the vegetative one. They reach 20-25 microns, are mobile, parasitize, penetrating the mucous membrane of the colon, and infect the intestines. They are detected only in acute amoebiasis in the affected organs; they are found extremely rarely in liquid feces - during the disintegration of intestinal ulcers.
Cysts form from the luminal form in the lower parts of the colon. They have a round shape and reach 8-15 microns. They are immobile, covered with a dense shell of chitin, and contain chromatoid bodies (RNA with protein) and glycogen. Depending on the maturity of the cysts, they contain from 1 to 4 nuclei. They are more often detected in patients with chronic amoebiasis and parasite carriers. They are very stable in the external environment: they remain in feces at room temperature for up to 2 weeks or longer, when frozen to −21°C - no more than 3 months, in water - up to 8 months. When heated to 100°C and boiled, they quickly die. Standard household disinfectants with chlorine have almost no effect on cysts. Soap-cresol preparations, a solution of sublimate 1:1000 and a 3% solution of carbolic acid can affect them [1][3][7][10].
Epidemiology
Amoebiasis is a widespread disease, mainly found in the countries of Southern and Western Africa, Central and South America, as well as in India, China and Korea. In Russia, isolated cases are mainly recorded, mainly in the southern regions, the Caucasus and the Far East. Although recently the incidence in our country has been increasing. This may be due to the influx of migrants from border regions and the development of tourism.
On average, about 50 million cases of amoebiasis are registered annually in the world, of which about 100 thousand end in death. In terms of the number of deaths, this disease ranks third among parasitic diseases. Approximately 90% of cases of the disease are intestinal amoebiasis, the remaining forms are extraintestinal.
The source of infection is a person (patient or carrier). With its feces, amoebas in the form of cysts enter the environment.
The transmission mechanism is fecal-oral. Includes water, food, household contact and sexual (oral-anal) transmission routes. Infection can occur when any substance (water, food, dirt, fingers) that comes into contact with the feces of an infected person or contains some part of it enters the mouth. Mechanical spreaders and carriers can be cockroaches and flies. In extremely rare cases, homosexuals and patients with secondary immunodeficiency may become infected when amoebas enter directly into the wound.
A person with amoebiasis runs the risk of transmitting the infection to family members, but this risk is low, especially if the person follows the rules of personal hygiene: thoroughly washes his hands after using the restroom and before preparing food.
Situations that increase the risk of infection:
- visiting tropical countries with low levels of sanitation;
- interaction with immigrants from tropical countries with poor sanitary conditions;
- neglect of personal hygiene rules;
- consumption of raw, undisinfected water from open sources and the water supply system;
- homosexual contacts;
- presence of mental disorders.
Immunity after an illness is unstable and weakly expressed, repeated infections are possible. Even a large number of antibodies formed, for example in amoebic liver abscesses, do not protect against the progression of amebiasis [1][2][5][6].
General information
Amebiasis belongs to the group of protozoa (anthroponotic protozoal diseases), the causative agents of which are protozoa.
It is characterized by a wide range of symptoms - from asymptomatic carriage to severe intestinal (intestinal amebiasis) and extraintestinal lesions - skin, liver, lungs, brain, pleura (extraintestinal amebiasis). A widespread disease, mainly in countries with a tropical/subtropical climate - India, countries of central/south America, Africa (Ghana, Benin, Nigeria, Ivory Coast), Asia (China, Korea), where the infection rate of the population with dysenteric amoeba can reach 25 -40%. It should be noted that in almost 85-90% of infected individuals non-invasive amebiasis occurs (carriers of amoebas without any clinical manifestations) and only 10-15% of infected individuals develop invasive (with clinical manifestations) amebiasis. The spread of the disease is due to the low economic, sanitary and hygienic standard of living, and high population migration. Among parasitic infections in terms of mortality in the world, it ranks third after malaria and schistosomiasis . In Russia, amebiasis in adults and children is registered as a sporadic disease, in the form of imported cases among foreign tourists; epidemic outbreaks are extremely rare. However, according to experts, amebiasis is underdiagnosed and about 50% of cases are not recognized in a timely manner, and patients are treated with erroneous diagnoses of shigellosis , banal colitis , dyspepsia , dysbacteriosis , and in some cases, patients with amebiasis are regarded as “healthy” cysto/amoebiasis carriers and are not treated at all.
In the CIS countries, regions endemic for amoebiasis include Transcaucasia (Armenia, Georgia) and Central Asia (Turkmenistan, Kyrgyzstan). The most common form of amoebiasis is amoebic dysentery (amebic dysenteric colitis). Currently, with early diagnosis and adequate treatment, intestinal amebiasis is an almost completely curable disease, with the exception of fulminant amoebic colitis .
Diet
In the acute period, with severe intestinal disorders, Diet No. 4 for the entire acute period. In the acute period, it is necessary to exclude coarse fiber from the diet and limit the amount of carbohydrates. The calorie content of the diet should be 2500-3000 kcal/day. When intestinal dysfunction decreases and the general condition improves, the patient is transferred to Diet No. 2 . And immediately before discharge from the hospital (3-4 days before), the patient can be transferred to the general Diet No. 15 .
In cases of prolonged acute and chronic amoebiasis with a severe course, taking into account the frequency of loose stools, vomiting, lack of appetite and loss of body weight, the patient should be prescribed additional enteral/parenteral nutrition at the rate of 3500-4000 kcal/day, intravenous administration of amino acid mixtures in combination with polyionic glucose solutions (in a volume of 500–1000 ml) with insulin . If it is impossible/refusal to eat, liquid nutritional mixtures are administered through a tube.
Folk remedies
Photo: stojak.ru
Treatment of a disease such as amoebiasis must be prescribed exclusively by an experienced specialist. But there are often cases when patients doubt modern medicine and want to try their luck and get rid of the disease using folk remedies. You can also try to eliminate this disease with some herbs and other plants. Namely, folk remedies for amoebiasis include:
- Garlic. They say that garlic tincture is very helpful in the case of amoebiasis. You need to mix forty grams of garlic and one hundred grams of vodka, and then take this mixture about ten drops three times a day and thirty minutes before you sit down to eat.
- Bird cherry. You should use about ten grams of bird cherry berries, poured with 200 ml of ordinary boiled water. The mixture must be infused for three to four hours. Half a glass is taken orally half an hour before meals.
- Caraway. This plant is considered the most effective in folk medicine for the treatment of amoebiasis. Take 200 milliliters of boiling water and add cumin, and then infuse for fifteen minutes. After this, the mixture should cool slightly. The tincture is filtered and stored in the refrigerator for two days. She drinks half a glass twice a day after meals.
- Hawthorn and sea buckthorn. Many people are familiar with these remedies first-hand, because many ailments can be treated with their help. You need to boil one hundred grams of fruit in two different glasses. After this, the drink is cooled, filtered and taken in small portions over several days.
Treatment of amoebiasis with herbs
Amoebiasis can also be treated with the help of certain herbs:
- Eucalyptus leaves can slow down or even suppress the progression of amoebiasis. In order to make a tincture, you need to mix 30 milliliters of water with 5 milliliters of an alcohol solution (one percent) and take three times a day half an hour before meals.
- Mix forty drops of tincture of alcohol and black poplar with warm water and drink an hour before meals.
Thus, treatment of amebiasis with folk remedies is, of course, possible. But not in the later stages. That is why you need to remember that common sense should prevail over your doubts in modern medicine, if any. And the first thing to do is to immediately seek help from a doctor, since only an experienced specialist is able to make a truly truthful diagnosis and prescribe proper treatment for the patient.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
Epidemiology
The source of the pathogen is a sick person in remission, a convalescent, a carrier of the pathogen, releasing cysts with feces. The process of releasing cysts by carriers can be extremely lengthy (over many years). A typical fecal-oral mechanism of transmission of the pathogen occurs when consuming contaminated food and water, through contaminated hands or household items. Much less often, cysts are transferred by insects (cockroaches/flies). The natural susceptibility of people to amoebiasis is quite high (the contagiousness index is 20%). After an illness, the patient develops relative and short-term immunity .
Classification
In accordance with pathomorphological changes and symptoms, “invasive” and “non-invasive” amebiasis are distinguished. Invasive amoebiasis (pathological changes develop) is characterized by:
- Clinical manifestation of the disease.
- trophozoites in feces .
- The appearance of characteristic changes in the intestinal mucosa during endoscopic studies.
- The presence of specific antibodies during a serological test.
“Non-invasive” intestinal amebiasis (carriage) is characterized by:
- No clinical symptoms.
- Absence of trophozoites .
- Endoscopic examination revealed the absence of pathological changes in the colon mucosa.
- Lack of specific antibodies.
The clinical classification of amebiasis includes asymptomatic carriage, amoebic dysentery , gastroenteritis , amoeboma , complicated intestinal amebiasis , postamoebic colitis .
Based on the severity of symptoms, they are divided into manifest and subclinical forms.
By duration: acute (up to 3 months); subacute (up to 6 months); chronic (more than 6 months).
According to the nature of the course: continuously progressive and recurrent amoebiasis.
List of sources
- Bronstein A.M. Amoebiasis: clinical picture, diagnosis, treatment. Methodological manual, M., 2002
- Eremushkina M. A., Burchik M. A., Popova L. S. Amebiasis in Moscow // New technologies in the diagnosis and treatment of infectious diseases: Collection. abstract VII Ross. Congress of Infectious Diseases. - N. Novgorod, 2006. - P. 211.
- Yushchuk N. D., Vengerov Yu. Ya. Lectures on infectious diseases. 3rd ed., revised. and additional M.: OJSC "Publishing House Medicine", 2007. 1032 p.
- Alikeeva G.K., Kukhtevich, E.V., Safiullina N.H. Amebiasis // Attending physician. - 2011; No. 3.
- Shamov Yu. A. Some aspects of amoebiasis at the present stage of its study // Pathogenesis, immunology, clinic and diagnosis of infectious diseases. — M., 1992.— P. 92–99.