Rotavirus infection is caused by rotavirus (lat. Rotavirus). This disease has other names. For example, RI, intestinal flu, rotavirus gastroenteritis, rotavirosis, stomach flu. The incubation period is short: from 1 to 5 days. The disease can affect people of any age, only adults suffer from it in a milder form.
A person infected with the virus is a source of infection, starting from the very first day of the disease. Until all symptoms go away, the person remains contagious. Recovery can be expected 5–7 days after the onset of the disease. After an infection, the body develops stable immunity. If the disease is suffered in adulthood and the body has produced a small amount of antibodies, another infection may occur.
Methods of transmission of rotavirus infection
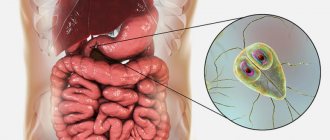
Rotavirus. This is what he looks like
In most cases, the gate through which rotavirus enters is the human mouth. Poorly washed fruits and eating with dirty hands inevitably lead to infection. Features of the production of dairy products can cause the spread of infection through this type of food.
Rotaviruses are generally very tenacious. They are kept in the refrigerator for several days, tolerate chlorination of water, even holy water does not stop them. Starting to visit child care institutions can provoke the appearance of this infection in a child.
After all, the body has to adapt when faced with unusual microbes and viruses. Rotavirus is also classified as a “dirty hand” disease. By causing inflammation of the respiratory tract, rotaviruses can spread in the same way as regular flu. For example, when coughing or sneezing. So the airborne method of spread is also inherent in them.
Rotavirus infection can spread in different ways, for example, as isolated cases of disease or as an epidemic.
The virus settles in the mucous membrane of the gastrointestinal tract. In first place is the mucous membrane of the small intestine. The virus causes enteritis here, that is, inflammation of the mucous membrane. Enteritis has its own symptoms, which are easily distinguished from others.
INTESTINAL INFECTIONS
Precaution is simple, but repentance is complex.
Goethe
Food and water consumed by humans are far from sterile. Billions of a wide variety of bacteria enter our bodies every day and hourly, and absolutely nothing bad happens from this - nature has invented too many ways to neutralize microbes. Saliva with bactericidal properties, poisonous gastric juice, a lot of our own, “good” bacteria in the intestines - all this does not give strangers the opportunity to take root and do their dirty deed.
Nevertheless, a person who has never had an intestinal infection simply does not exist. It does not exist, if only because there are many ways to neutralize all the numerous protective forces - swallow without chewing so that saliva does not have time to reach the microbes, overeat, neutralize acidic gastric juice with alkaline drinks, kill your own microbes with antibiotics, etc.
But the main cause of intestinal infections was, is and will be non-compliance with basic hygiene standards - improper storage of food, unwashed hands, flies scurrying between the dining table and the toilet. In the end, no matter what wonderful protective powers the human body possesses, there will always be a number of microbes that are simply impossible to neutralize.
The causative agents of intestinal infections can be bacteria (dysentery bacillus, salmonella, staphylococcus, typhoid bacillus, vibrio cholera) and some viruses.
The specific name of a specific pathogen of a specific intestinal infection is of interest, first of all, to medical workers. The volume, focus and intensity of anti-epidemic measures are largely determined by the type of pathogen.
Some bacteria spread through water, others through food, and these products are not just any, but very specific ones. In one case - vegetables, in another - eggs, in the third - dairy products, etc.
Some bacteria are very(!) contagious (for example, the causative agent of cholera), others are less so.
In one case, the disease develops rapidly and poses a real threat to human life, in the other, the symptoms develop slowly, and the disease itself is not particularly dangerous.
Microbes, causative agents of intestinal infections, can (as a rule, this is what happens) affect not the entire gastrointestinal tract, but certain parts of it. The inflammatory process in each such department has its own medical name: inflammation of the stomach - GASTRITIS, of the duodenum - DUODENITIS, of the small intestine - ENTERITIS, of the large intestine - COLITIS.
Remember - we already cited similar words when we wrote about damage to the respiratory system: rhinitis, pharyngitis, laryngitis, tracheitis, bronchitis... The situation with the gastrointestinal tract is similar, and the simultaneous defeat of several of its parts gives rise to the use of complex and scary words: gastroduodenitis, gastroenteritis, enterocolitis, gastroenterocolitis. It becomes clear that the medical term “enterocolitis” is not the name of the disease - it only characterizes damage to a certain area of the gastrointestinal tract. Doctors identify this very “specific area” quite easily - by the symptoms of the disease and by the appearance of the stool. But it is quite difficult to determine the exact name of the disease based on the symptoms. Although many intestinal infections have very characteristic symptoms. At least dysentery, typhoid fever, and cholera can often be diagnosed without additional tests.
Nevertheless, no matter how obvious the symptoms are, the final diagnosis is made only after a microbiological examination (stool, vomit, water collected after gastric lavage, blood, “suspicious” foods and drinks) are examined. They found a dysentery bacillus - that means it’s definitely dysentery. If they found salmonella, that means it’s definitely salmonellosis, etc.
But everything is not so simple. In order to make a diagnosis, one must do more than just detect the microbe. It is necessary that the detection of a microbe be accompanied by specific symptoms of an intestinal infection - vomiting, diarrhea, etc. During a wide variety of preventive examinations (before, for example, a child goes to kindergarten or school, before going to a sanatorium), it is often found in the stool something bad - dangerous E. coli, or salmonella, or dysentery bacillus. If the microbe is present, but there are no manifestations of intestinal infection, this situation indicates that this person (an adult or a child, it does not matter) - a “victim of bacteriological examination” - is a healthy carrier of a certain bacterium. That is, this person has immunity to this pathogen; in other words, he cannot get sick, but still poses a threat to society because he spreads the infection. And doctors will certainly take a close look at such a person.
***
After entering the human body, pathogens of intestinal infections begin to actively multiply, which leads, firstly, to disturbances in the digestive process and, secondly, to inflammation of the cells of the intestinal mucosa. The typical and most characteristic consequence of these two processes is the main symptom of any intestinal infection - diarrhea [1]. Other signs of the disease - nausea, vomiting, abdominal pain, fever, lack of appetite, general weakness - are common, but are not obligatory accompaniments of intestinal infection.
By the way, it should be noted that at the everyday and at the medical level, the concepts of intestinal infection are very different. For an ordinary person it is clear: if there is diarrhea, then there is an intestinal infection, but for a doctor the main thing is not the symptoms, but the route of infection. From a medical point of view, any disease transmitted through the mouth (with food, water, unwashed hands - the so-called fecal-oral route of infection) is a typical intestinal infection. The most significant example is viral hepatitis A (Botkin's disease). Infection with the virus always occurs when it enters the gastrointestinal tract, but the liver is affected, and in most cases there is no diarrhea.
The ways to prevent intestinal infections are quite obvious and come down to compliance with basic hygiene standards: washing hands, especially thoroughly after visiting the toilet, heat treatment of food and water, following the rules for storing food, isolating patients and, at a minimum, providing them with separate utensils.
You should always remember that the most terrible and dangerous consequence of any diarrhea is the loss of fluid and salts by the body . Without food, the human body can survive more or less safely for a couple of weeks, but without an adequate supply of water and salts of potassium, sodium, and calcium, a person cannot live: in this case, the clock counts.
The reserves of water and salts in the child’s body are especially small, and it is for children that intestinal infections pose a real threat to health and life.
Thus, the true severity of an intestinal infection is often determined not by the frequency of stool, not by the smell and color of stool, but by the degree of dehydration. Only a doctor can determine the severity of an intestinal infection, but the likelihood that people will seek medical help for every diarrhea is very low. Therefore, we emphasize that regardless of the name of a particular intestinal infection, there are very specific rules of behavior for the patient and his relatives.
- You should always think about what you ate or what you fed your child. It's not so bad if it's your personal culinary masterpiece, but if it's a cake from a nearby store, then you should be conscious and think about those who might follow in your footsteps. Finding out the phone number of the district sanitary station is not at all difficult.
- An intestinal infection in any family member is an alarm for everyone else. The patient needs separate dishes, everyone else needs to ensure perfect cleanliness, wash their hands thoroughly, put suspicious products away from harm, boil all the dishes, and do not skimp on disinfectants.
- Both diarrhea and vomiting are ways of protecting the body. In a simplified version, it looks like this: something wrong has entered the gastrointestinal tract, and the body is trying in every possible way to remove this nasty thing. Therefore, in the first hours of an intestinal infection, we are not at all interested in stopping the diarrhea and vomiting. On the contrary, the body should be helped in both directions - drink and vomit (and if you don’t want to, deliberately induce vomiting, thereby washing the stomach), cleanse the large intestine with an enema. For the enema, ordinary boiled water is used, in no case warm (the optimal temperature is about 20 ° C), be sure to ensure that all the injected liquid comes out.
- The main principle of assistance is to replenish fluid and salt losses. Medicines available in any pharmacy and representing a pre-prepared mixture of various salts, which are diluted with boiled water before use, are ideal for this purpose. If the pharmacy is far away, mineral waters, decoctions of raisins, herbs, rose hips, dried fruit compote, or tea, better green than black, are quite suitable. After all, it's better to drink what you have on hand than to drink nothing.
- The temperature of the drinks should be approximately equal to body temperature - in this case, the absorption of liquid from the stomach into the blood will be as fast as possible.
- If vomiting persists, remember that you need to drink more often, but in small portions , so as not to stretch the stomach, and always coordinate the use of any antiemetic drugs with your doctor.
- By and large, there are only two absolutely safe ways to self-treat intestinal infections - fasting and drinking plenty of fluids. Any medications can lead to the most unexpected consequences, except that intestinal sorbents[2] are advisable and almost always indicated.
- The intensity of your worries should be closely related to the general condition of the child, and not to how many times he soiled the diapers (asked to use the potty, ran to the toilet). Monitor the color of your urine: if it is light, there is no fluid deficiency.
- Seeing a doctor is mandatory for diarrhea in children of the first year of life and, regardless of age, in the absence of a tendency to improve within 24 hours.
10. Seek medical attention immediately if:
- the most worrying symptom of an intestinal infection is abdominal pain;
- due to persistent vomiting, you cannot give your child something to drink;
- no urine for more than 6 hours;
- dry tongue, sunken eyes, skin has acquired a grayish tint;
- there is an admixture of blood in the stool;
- the diarrhea stopped, but the vomiting increased, and (or) the body temperature rose sharply, and (or) abdominal pain appeared.
11. When the condition improves, do not rush to feed the baby everything. Tea with low-fat cottage cheese, rice and oatmeal - let him be patient and fast for a day or two, he will be healthier.
***
It should be noted: modern therapy for intestinal infections does not at all involve swallowing everyone’s favorite phthalazole and chloramphenicol, if only because every second diarrhea is caused by viruses [3], on which the mentioned antibacterial drugs do not act at all. But even if it is a bacteria, the attitude towards the use of antibacterial drugs is ambiguous. Thus, for dysentery, antibiotics are almost always used, and for salmonellosis - much less often.
The paradox of treating intestinal infections lies primarily in the fact that a strict diet, replenishment of fluid and salt losses, plus time and patience are almost always sufficient conditions for recovery (compliance with hygiene rules is implied).
What's so paradoxical here? - you ask. First of all, in the opinion of our compatriots, drinking and starving is extremely insufficient for “full” treatment, you need more pills, and more...
The need for the above-mentioned “full” treatment is being successfully tried to be met by medical science, which is actively developing new methods of helping intestinal victims.
Thus, as an alternative to antibiotics, it is proposed to use so-called eubiotics - beneficial intestinal bacteria, which should be “released” into the intestines, hoping that they themselves will “drive out” the uninvited guest.
Another proposed method of treating intestinal infections is based on the fact that almost all bacteria have natural enemies - special viruses that infect bacteria. Such viruses are called bacteriophages , or simply phages. Preparations containing certain phages have already been developed, actively produced and used: “salmonella bacteriophage” - for the treatment of salmonellosis, “dysentery bacteriophage” for the treatment of dysentery, etc.
Nevertheless, we have to sadly admit that, despite the theoretical logic and attractiveness, the practical use of both eubiotics and bacteriophages does not lead to recovery faster than the same diet and drink.
It is not surprising that in the vast majority of countries in the world these drugs are not used (and are not produced or registered), since medical science is not yet able to prove their effectiveness[4].
***
In a hospital, the main method of providing emergency care for intestinal infections is infusion therapy , i.e. intravenous administration of fluids and salts to quickly compensate for losses.
For the most dangerous intestinal infection - cholera - infusion therapy is generally the most important. The causative agent of cholera produces an exotoxin (called cholerogens), which is located in the intestinal lumen, and therefore cannot be neutralized by serum. Under the influence of cholerogens, the cells of the intestinal mucosa seem to shrink and lose fluid in liters! So you have to administer drugs intravenously in large quantities and carry out very active treatment until antibodies to the toxin appear in the body.
[1] Diarrhea (synonymous with diarrhea) is frequent bowel movements in which the stool has a liquid consistency (definition from the Encyclopedic Dictionary of Medical Terms, M.: Soviet Encyclopedia, 1983).
[2] Intestinal sorbents are a large group of drugs that can bind (sorb) and neutralize poisons (toxins) located in the intestinal lumen. The most famous intestinal sorbent is the famous activated carbon, although there are other drugs that are tens and hundreds of times more active.
[3] The most famous virus that causes severe intestinal infections in children is the so-called rotavirus, which most often affects children in the first two years of life. It is not surprising in this regard that vaccination against rotavirus infection is present in the vaccination calendar of many countries around the world.
[4] At the same time, both bacteriophages and eubiotics are clearly safe drugs. Safety, combined with theoretical feasibility, plus the ability to satisfy parents’ needs for “full” treatment - all these are factors that determine the massive use of these drugs in our country.
author Komarovsky E.O. book Child's health and the common sense of his relatives published 02/24/2010 18:19
Symptoms of rotavirosis in pediatric patients
The disease has several stages:
- Incubation stage. From 1 to 5 days.
- Acute stage. From 3 to 7 days. If the course is severe, it may last more than 7 days.
- Recovery stage. From 4 to 5 days.
Rotavirus infection manifests itself very sharply. Vomiting begins and the temperature rises greatly. Diarrhea often begins. The chair has its own specific properties. At first it is liquid, yellow in color, then becomes gray-yellow in color, similar to clay. In addition to the symptoms of enteritis, there are symptoms characteristic of ARVI. A runny nose begins, it hurts to swallow (redness in the throat). Weakness is clearly manifested, there is no appetite. If you analyze the characteristics of both feces and urine, you can find many similarities with the symptoms of hepatitis A.
Signs in adults
Rotavirus often affects adults. But the disease is mild. People think that they have a normal digestive disorder, so they don’t pay much attention to it. In adults, nausea and vomiting are rare. Usually everything is limited to diarrhea, a slight increase in temperature and weakness. Sometimes the symptoms are smoothed out to such an extent that the person does not pay attention to them at all.
And at this time, it still remains very contagious and can infect not only others in public places, but also children at home. The insignificant manifestation of signs of this disease can be explained by a more resistant organism and a higher degree of adaptability of the gastrointestinal tract to irritants of this kind. Therefore, if one person in a team or in a house gets sick, everyone else will experience the same thing, but not everyone will experience it to the same degree.
Treatment of the disease in children
Treatment is symptomatic.
Since it is impossible to kill rotavirus, treatment is carried out in such a way as to reduce symptoms. Firstly, it is necessary to normalize water-salt metabolism. It is disrupted due to vomiting, diarrhea, and causes weakness and serious condition. Secondly, we must try to prevent the development of a secondary infection, which can greatly prolong the disease.
In order not to artificially create a favorable environment for the growth of bacteria, it is necessary to exclude all lactic acid products from the menu of a sick child. Since the baby has no appetite, there is no need to force him to eat. You can offer him jelly or chicken broth. You have to prepare these dishes yourself so that all the ingredients are fresh and natural.
If the appetite is partially preserved, then you can offer the child liquid rice porridge, which must be prepared in water. No oil should be added. But a little sugar won't hurt. The main thing is not to use large portions. They will definitely provoke a gag reflex. Take short breaks between taking individual portions of food.
Principles of treatment
Treatment of rotavirus gastroenteritis is symptomatic and comprehensive. The need for hospitalization is rare and depends on the severity of the sick person’s condition. For mild forms of the disease, outpatient treatment is indicated. In this case, family members must carefully observe the rules of personal hygiene and disinfect the premises to prevent infection.
- following a gentle diet with the exclusion of dairy products and limiting carbohydrates, with split meals;
- measures to replenish the volume of lost fluid, for which saline, colloid and crystalloid solutions are prescribed for drinking or intravenous administration;
- detoxification using enterosorbents;
- immunoglobulins, antiviral agents (not always);
- multienzyme drugs to correct emerging digestive insufficiency;
- normalization of intestinal microbiocenosis with the help of probiotics.
It is usually recommended to continue the use of probiotic preparations even after the relief of the main symptoms of the disease. This will help restore disturbed intestinal microflora and form local immunity. The composition of the well-known probiotic "Acipol" includes lyophilisate of live lactobacilli acidophilus and polysaccharides obtained from kefir grains, which also help strengthen the immune system and increase the overall resistance of the body. It is important to remember that the prescription of certain drugs should be done by a doctor who makes a decision on the choice of drugs based on the results patient examinations.
Ways to combat high fever that occurs during illness
Rotavirus under a microscope
It is customary to lower the temperature only when the thermometer shows numbers above 38º. If the indicators are lower, then the temperature is brought down when it is difficult to bear, the patient complains of feeling unwell, and experiences discomfort. If the temperature rises above 38º, you need to put in Cefekon suppositories. They are relevant for children under 3 years of age.
But for older children, paracetamol is needed. The convenience of suppositories lies in the possibility of administering the drug to a sleeping child. When the temperature cannot be brought down in the usual way, you can combine paracetamol with a quarter of an analgin tablet. If a child is given medications containing paracetamol, take at least two hours between doses.
Excellently reduces the high temperature of rubbing. To do this, you can mix vodka and warm water or water with vinegar. Wipe the entire body with a moistened napkin, trying not to make the temperature of individual areas different. After wiping, you should put socks on your feet. They begin wiping if taking the tablets does not reduce the temperature after 30 minutes. It is necessary to ensure that a baby with a high temperature does not overheat. For this purpose, they do not put warm clothes on him or cover him with a warm blanket. Everything should be as usual.
If other compositions are used, the interval between doses is increased to 4 hours or longer, depending on the instructions.
If symptoms indicating an intestinal disorder appear, Enterofuril is introduced into the course of treatment. The dosage is prescribed according to the patient's age. Take it twice a day. Drink it for 5 days or more. This remedy will prevent prolonged diarrhea. Enterol successfully replaces Enterofuril.
Painkillers are started only when the diagnosis is confirmed. If it is definitely established that it is a rotavirus infection, you can give no-shpa. It is better to take the solution in an ampoule. Its contents are poured into the baby’s mouth, and can be washed down with water or tea.
As soon as the appetite appears, the baby should be given bactisubtil. It restores intestinal microflora and fights diarrhea. It should be given twice a day. Open the capsule, dissolve the powder in water, and give it before meals. Duration – 5 days.
How to treat rotavirus infection in a child
Any suspicion of an intestinal infection in a child is a reason to contact a pediatrician or infectious disease specialist. After the examination, the doctor prescribes the necessary tests and therapy.
In mild cases, rotavirus infection in a child can be treated at home1. If you follow the recommendations given by the doctor, recovery occurs on the 4th-5th day of the disease6.
In case of moderate to severe disease (high fever, lethargy and deterioration of the baby’s condition, repeated vomiting, watery stools more than 8 times a day)6, as well as the appearance of blood in the stool1, hospitalization is necessary1.
Treatment for rotavirus infection includes
3:
- Rehydration.
With a viral intestinal infection, the child’s body loses a large amount of water and salts3. To restore and maintain the water-salt balance, the pediatrician prescribes special solutions3. All recommendations on how and what to feed the baby are given to parents by the attending physician. - Diet therapy.
For mild cases of the disease, fasting for more than 4 hours is not recommended1. The child should, as before, receive food in accordance with his age1. In case of severe dehydration, in the first 2-4 hours, while rehydration is carried out, nutrition is temporarily stopped and then resumed in a gentle manner1. - Drug therapy.
Medicines for the treatment of rotavirus infection should be selected by a doctor, taking into account the baby’s age, symptoms and severity of the disease.
The specialist may prescribe:
- enterosorbents
3, which bind and remove viruses and toxins from the body resulting from their vital activity and digestive disorders7; - probiotics
3, containing live microorganisms beneficial to the body1; - antiviral drugs
3 acting on the causative agent of the disease; - immunomodulatory drugs
3, stimulating the body's defenses in the fight against infection3.
As part of complex therapy for rotavirus infection in children from 6 months to 18 years, Anaferon® for children can be used in the form of lozenges 8. Anaferon® for children has antiviral and immunostimulating activity8,9. Due to the content of antibodies to human interferon gamma, the drug reduces the concentration of viruses in affected tissues, activates immune cells, and increases the production of antibodies8.
Also, in the treatment of rotavirus gastroenetritis, doctors may prescribe enzyme preparations that facilitate digestion7.
Up to contents