“THE SITE IS UNDER RECONSTRUCTION WE APOLOGIZE FOR THE TEMPORARY INCONVENIENCE”
Anomalies are understood as deviations from the structure and/or function inherent in a given biological species, resulting from a violation of the development of the organism.The reasons leading to the development of anomalies are the impact on the fetus during pregnancy and embryogenesis of unfavorable environmental factors, infections, chemicals, and medications. Such factors are increased levels of radioactive radiation, hyperinsolation, hyperthermia, chemical products, rubella, and cytostatics.
Disturbances in the development of the colon during embryogenesis can affect all processes of its formation.
In this regard, according to the classification of G.I. Vorobyov et al (1989), there are:
- abnormalities of the intramural nervous system:
- congenital angiodysplasia of the colon:
- congenital elongation of the colon:
- congenital disorder of the position and fixation of the large intestine:
- colon duplication;
- a combination of various anomalies;
In more than 80% of cases, a combination of various types of anomalies is observed.
Anomalies of the development and position of the large intestine are distinguished by origin:
I. Congenital growth disorder of the colon.
If at the stage of embryo development the growth of the intestinal wall stops as a result of any reason, then congenital shortening or absence of any part of the colon occurs. As a rule, such an anomaly is combined with others, primarily rotational ones.
The formation of an unusually long colon due to excess growth is called dolichocolon. Most often, elongation is observed in the sigmoid colon. In such cases they talk about dolichosigma.
II. Colon position and mobility
is determined by such factors as its relationship to the peritoneal integument, the length and shape of the mesentery, the presence of fixing ligaments and adhesions in the abdominal cavity. The most common and clinically significant disorders of colon fixation are right-sided and left-sided coloptosis, total coloptosis, pathological mobility of the right parts of the colon. The greatest clinical significance is the pathological mobility of the right parts of the colon. This condition predisposes to cecal volvulus, ileocecal intussusception, and the development of pain. Abnormal mobility of the right half of the colon due to the presence of a common mesentery. The mobile right half of the colon in some people may not manifest itself in any way throughout their lives. Therefore, in an anatomical sense, this type of violation of fixation of the right half of the colon gives clinical manifestations and becomes a source of severe complications and should be considered as an independent disease. The main symptoms are abdominal pain, usually localized in the right iliac region. The pain is often constant, dull, sometimes paroxysmal, and often radiates to the sacrum, back and lower limb. Persistent chronic constipation is also a common symptom of this suffering, which appears to be associated with secondary changes in the motility of the right half of the colon. A typical example of the disease is flatulence, sometimes accompanied by splashing noise in the right iliac region.
III. Rotational anomalies.
If the growth of the intestinal tube during embryogenesis proceeded normally, but its rotation and fixation to the posterior wall of the abdomen at one of the stages were impaired, then this pathological condition leads to the occurrence of rotational anomalies. Lack of rotation is a rare condition, combined with severe anomalies of other organs and therefore incompatible with fetal life. This is why patients with a lack of intestinal rotation are not encountered in adult clinical practice. With incomplete rotation, or the so-called incomplete rotation, the essence of the anomaly lies in stopping the rotation of the intestinal tube at one of its stages.
Incomplete rotation (incomplete rotation of the intestine) is the main type of rotational anomalies found in adult patients.
IV. If the process of recanalization of the intestinal tube is disrupted
Colonic atresia may develop, which leads to acute intestinal obstruction in the newborn, and therefore similar anomalies do not occur in adults. Other abnormalities, such as intraluminal septa or strictures, may be detected throughout a person's life. A rare condition in coloproctological practice is colon duplication, which is most often localized in the rectum.
V. Embryonic cords and adhesions
may be presented in various variants, and their clinical manifestations will be determined by the localization and severity of symptoms of intestinal obstruction.
Diagnostics.
The most informative method for diagnosing anomalies in the development and position of the colon is x-ray. A contrast barium enema study allows you to immediately determine the position of the colon in the abdominal cavity, its shape, and mobility when conducting the study with the patient standing and lying down.
Treatment.
If the anomaly has an uncomplicated course and there is no mention of previous attacks of intestinal obstruction in the medical history, then clinical manifestations such as constipation and the development of pain require conservative measures. If persistent comprehensive conservative measures are ineffective, surgical intervention may be undertaken.
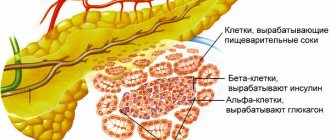
Hirschsprung's disease is a developmental anomaly of the colon, characterized by the absence of ganglia of the intramural nerve plexuses of the intestinal wall and manifested by a characteristic symptom complex of megacolons.
These changes consist mainly of the absence of ganglia of the musculo-intestinal and submucosal plexuses.
The cause of congenital underdevelopment of the intramural nervous apparatus of the colon (aganliosis) with the development of secondary megacolon is not completely clear. Mutations of 4 genes play a leading role in the mechanism of development of the disease; there is also a theory according to which aganglionosis develops as a result of impaired differentiation of nerve cells that have already reached the intestinal wall. Various factors can affect cell maturation, such as hypoxia, exposure to chemical agents, increased radiation, and viral infection. The combination of genetic disorders with the pathological influence of external and internal environmental factors determines the nature of the damage not only to the intramural nervous system.
Based on the prevalence of the aganglionic zone, the following variants of Hirschsprung's disease are distinguished:
- nadanal
- rectal
- rectosigmoid
- left-handed
- subtotal
- total.
Characteristic of Hirschsprung's disease is the obligatory spread of aganliosis in the distal direction to the internal sphincter. Cases of segmental aganliosis are extremely rare.
Clinic.
The earliest and main manifestation of the disease is difficulty in emptying the colon, up to the complete absence of independent stool.
The occurrence of other symptoms (abdominal pain, nausea, lack of apatite, weight loss) depends on the duration of chronic intestinal obstruction and measures to eliminate it. Often, conventional conservative measures (cleansing enemas) are ineffective. Gradually, fecal stones form in the expanded sections, reaching in some cases a diameter of 20-25-30 cm. The dilated, atonic intestine is a place of constant accumulation of gases, therefore flatulence is one of the most constant symptoms of Hirschsprung's disease in adults. Flatulence and expansion of the colon gradually lead to deformation of the abdomen and chest. The abdomen is significantly increased in size, the costal angle is turned as in pulmonary emphysema. Palpation of the abdomen reveals an accumulation of feces, especially pronounced in the left sections and the sigmoid colon. In some patients, against the background of a long-term absence of stool, uncontrollable diarrhea suddenly appears, often accompanied by a collaptoid state.
Diagnosis of Hirschsprung's disease in adults
is based on a thorough study of the anamnesis, clinical symptoms, results of radiological and functional research methods.
X-ray contrast examination of the colon (irrigoscopy) is the main method for diagnosing Hirschsprung's disease. The presence in the images of a zone of narrowing in the distal colon with suprastenotic dilatation is the hallmark of the anomaly.
Anorectal manometry is of great importance in diagnosis, determining the state of the rectoanal inhibitory reflex - the absence of the rectoanal reflex, which is characteristic of Hirschsprung's disease. The recto-anal reflex during manometry was induced by irritating the rectum with a balloon in which air was injected.
Diagnostic criteria for Hirschsprung's disease in adults include:
- constipation from early childhood,
- the presence of a narrowing zone in the distal parts of the colon with suprastenotic expansion on irrigograms,
- absence of rectoanal reflex during manometry,
- positive reaction of the rectal mucosa to acetylcholine esterase,
- absence of ganglia of the intramural nervous system according to morphological studies.
A reliable method for diagnosing the disease is to identify the aganlionic zone in the colon - histochemical determination of acetylcholinesterase in the mucous membrane. It is based on the phenomenon of excessive accumulation of the enzyme in the mucous membrane of the aganglionic segment of the colon. To conduct the study, pieces of the rectal mucosa were taken from levels 5 and 10.15 cm from the anus using a rectoscope and biopsy forceps.
In doubtful cases, in the absence of characteristic complaints, the presence of an unclear x-ray picture, a weakened reaction of the internal sphincter to rectal distension, a weakly positive reaction to AChE, for a more accurate diagnosis of Hirschsprung's disease and other anomalies of the development of the intramural nervous system of the colon, it is advisable to use a biopsy modification developed at the State Research Center walls of the rectum according to Swenson. The essence of the surgical technique is starting at a distance of 6 cm, proximal to the dentate line, in the distal direction from the wall of the rectum, all its layers are captured, and a strip of tissue 6 cm long and 1 cm wide is excised. Histological examination of a rectal biopsy, including the physiological zone hypoganglionosis and the upstream area with potentially normal nerve plexuses, allows us to give a more complete and objective assessment of the state of the nervous apparatus of the rectum. In the absence of ganglia throughout the entire length of the study specimen, a diagnosis of colon is established. The identification of rare individual ganglia, both in the distal and proximal parts of the specimen, indicates colon hypogangliosis.
Differential diagnosis
Hirschsprung's disease must first be performed with other forms or types of megacolon.
Treatment.
The goal of treating patients with Hirschsprung's disease is to normalize the evacuation of colon contents. This goal can only be achieved by removing or switching off the aganlionic zone, if the overlying parts of the colon are not in a state of decompensation.
In recent years, multi-stage surgical treatment has been used. Stage 1 resection of the sigmoid colon according to Mikulicz, subtotal resection of the colon includes: colostomy, ileostomy, resection of the sigmoid colon according to Hartmann, according to Lahey. When compensation is achieved for the enlarged sections of the colon, the second stage of treatment ranges from 6 to 1.5 years, reconstructive operations are performed, the Duhamel operation is modified by the State Scientific Center for Clinical Hospital.
Anomalies and malformations
Abnormalities of the position (dystopia) of the colon occur due to disorders of intrauterine development. There is an abnormal location of the entire intestine in the left or only in the right half of the abdominal cavity. The length of all sections of the colon (dolichocolon) or its individual sections (dolichosigma - lengthening of the sigmoid section) may increase. This is accompanied by constipation, flatulence, and abdominal pain. Doubling (duplication) of a section or the entire colon is very rare.
Hirschsprung's disease (aganglionic megacolon)
Hirschsprung's disease (N. Hirschsprung, 1887) is a malformation of the left half of the colon. The disease is a congenital pathology and is hereditary in nature (occurs in 1 in 5,000 children born). Boys get sick 5 times more often than girls. About 5% of children with Hirschsprung disease have Down syndrome. If the aganglionic portion of the intestine is small and localized in the rectum, then symptoms of the disease may appear in adulthood. This type of disease is called "adult Hirschsprung disease."
It is characterized by the absence of parasympathetic innervation of the intestinal wall in a certain area of the colon. A section of the intestine devoid of nerve ganglia is constantly contracted spastically and does not peristalt; as a result, the upstream sections of the intestine, which have normal innervation, expand and hypertrophy, which leads to the development of megacolons.
The severity of the disease depends on the extent of the aganglionic portion of the colon. Violation of the passage of intestinal contents is determined by the clinical manifestations of the disease, the main symptoms of which are constipation, bloating, pain, and rumbling in the abdomen. Complications. Hirschsprung's disease can be complicated by intestinal obstruction, inflammation and ulceration of the mucous membrane in the dilated parts of the colon, intestinal perforation, and bleeding.
Treatment. Conservative treatment is only a preparatory stage for surgery.
Idiopathic megacolon
In people suffering from chronic constipation, an X-ray examination reveals an elongated and dilated sigmoid colon (dolichosigma) or an expansion of the descending or entire colon (megadolichocolon), which, in the absence of a narrowing zone, excludes Hirschsprung's disease. This type of disease is called "idiopathic megacolon."
Treatment. In most cases, conservative.
Congenital defects of the colon
With aplasia of the cecum and appendix, the continuity of the gastrointestinal tract is usually preserved, but the characteristic expansion of the intestinal tube, which normally appears at the 6th week of intrauterine life, is absent. TTP - until the 7th week.
Hypoplasia of the colon below the splenic angle is an integral part of the syndrome, manifested by functional intestinal obstruction; no innervation disorders are detected. It should be differentiated from the long-segmented type of Hirschsprung's disease.
Atresia and stenosis of the colon make up from 1.8 to 10% of all cases of atresia and intestinal stenosis, their population frequency is 1 case per 20,000-40,000 births. About half of all observations occur in the ascending colon, where atresia in the form of free blind ends is more common; in general, type 1 atresia accounts for 23.5%, type II -34.3%, type III -4 1.1% of all colon occlusions. Atresias and stenoses in half of the cases are located distal to the splenic angle of the thick ligament. Being a component of multiple defects, in 90% of cases they are combined with developmental disorders of the genitourinary system, in 22.5% - with anomalies of the musculoskeletal system and heart. Atresias and stenoses of the colon have been observed in trisomy 20 and caudal regression syndrome. Atresia of the sigmoid colon was found in 2 half-siblings and a maternal uncle.
Colon duplications, in contrast to small intestinal duplications, are often combined with other congenital defects, may have communication with the urogenital system and are rarely accompanied by heterotopia in their gastric-type mucosal wall.
Duplications of the cecum and appendix, as well as isolated duplications of the appendix, have been described. The latter are of three types:
- shoot in the form of a double-barreled shotgun; usually the only defect, observed in 1/3 of all cases of appendix duplication described in the literature;
- “bird type” with the presence of two normally developed processes located symmetrically on both sides of the cecum, is combined with other defects.
- the most common type, in which one process is located in the usual place, and the other, as a rule, is rudimentary. TTP - before the 3rd month of pregnancy.
Focal aplasia of the muscular lining of the colon is the most common localization of this congenital defect. No patterns in the location of defects in relation to the mesentery were identified in TTP until the 9th week of intrauterine development.
Hyperplasia (congenital gigantism) - expansion and lengthening of the large intestine. There are several variants of this defect.
Dolichosigma is a congenital elongation of the colon without elements of its expansion. The elongated sigmoid colon, as a rule, forms 2-3 or more additional loops. In children, elongation of the sigmoid colon is usually accompanied by its expansion, sometimes reaching 10-20 cm, and the formation of megadolichosigma.
Dolichocolon is an elongation of the large intestine due to excessive growth in length of the transverse colon, descending and sigmoid colons. In cases of megadolichocolon, the elongation is accompanied by a uniform expansion of the lumen of the colon and hypertrophy of its wall. . Histological examination of these types of expansion and elongation of the colon reveals focal ulcerations of the mucous membrane, edema, vasodilatation and sclerosis of the submucosal and muscular layers, dystrophic changes in the cells of the intermuscular plexus (Auerbach plexus). These types of defects must be differentiated from secondary expansion of the colon due to congenital stenosis of the anus or its cicatricial narrowing after undergoing proctoplasty, as well as congenital aganglionosis of the colon - Hirschsprung's disease.
Treatment is conservative; if unsuccessful, surgical treatment.
Acute intestinal obstruction accounts for 3.8% of all emergency diseases of the abdominal organs [1]. Mortality rate in acute intestinal obstruction remains stable - 8-13% [2, 3]. Among the wide variety of diseases of the abdominal organs, anomalies in the development of the colon are not the least important. Some of them occur for a long time without clinical manifestations [4]. The most common anomalies of the colon are the common mesentery of the cecum and ileum, megadolichosigma, which can cause the development of acute intestinal obstruction. The left-sided position of the large intestine or the high position of the cecum, a common mesentery for the small and large intestine are characteristic of animals. They pose a danger to humans and occur in 2.4% of cases [4]. In addition to the fixation of the colon by the mesenteries, special anatomical formations are found individually in the ligamentous apparatus, macroscopically representing translucent veil-like “adhesions”, “films”, etc. Histological examination of them does not reveal traces of inflammation, there is a normal structure of lymphatic and blood vessels, muscle the walls of the adjacent intestine or neighboring organ. Thus, these membranous formations are formed in the embryonic period during the process of growth, rotation and fixation of the intestine and are found in 1.4% of cases [4]. Many authors interpreted large membranous formations as internal hernias arising as a result of uneven rotation of the intestine in the second period of development [3]. C. Gardner (1934) described a case of strangulation of the entire small intestine in such a hernial sac [5].
Being a finding during surgery, anomalies in the development of the colon create difficulties in choosing treatment tactics. Often in such situations the anomaly is not corrected.
In this article we present a clinical case demonstrating the features of the clinical manifestations of acute intestinal obstruction caused by an anomaly in the development of the large intestine, and surgical tactics.
Patient G.
, 53 years old, was admitted to the surgical department for emergency indications on 02/27/12 at 23:20 for emergency indications 3 hours after the onset of the disease. Upon admission, the patient complained of spastic pain in the right half of the abdomen, nausea, vomiting, and general weakness. She took the drug espumizan on her own at home. The pain persisted and even intensified. From the life history it is known that in 2007, an endoscopic examination of the patient revealed an esophageal ulcer; in 1983, a tubectomy was performed on the right. The allergic history is unremarkable.
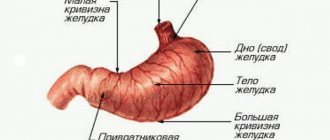
Upon admission, the patient's general condition was assessed as moderate. The skin is clean, somewhat pale. The patient has a correct physique and satisfactory nutrition. Breathing in the lungs is vesicular, carried out in all parts, there is no wheezing, the respiratory rate is 18 per minute. Heart sounds are sonorous, the rhythm is correct, pulse is 76 per minute, blood pressure is 130/80 mm Hg. The tongue is dry, covered with a white-yellow coating. The abdomen is symmetrical, participates in the act of breathing, soft, painful in the epigastrium and right hypochondrium. Intestinal peristalsis is heard. There are no symptoms of peritoneal irritation. General blood test: Hb 145 g/l, l. 4.0·109/l, p. 1%, p. — 63%, mon. 8%, lymph. 28%, ESR 7 mm/h. Biochemical blood test: glucose 7.8 µmol/l, ALT 16.2 U/l, AST 22 U/l, creatinine 52 µmol/l, total bilirubin 29.3 mmol/l, direct bilirubin 7.0 mmol/l, alpha amylase 89.7 units/l, general urinalysis without features, urine diastasis 420.4 units/l. The ECG shows sinus rhythm, horizontal position of the electrical axis of the heart, metabolic changes in the myocardium of the anterior wall of the left ventricle. FGDS data: erosive reflux esophagitis, erosive gastritis. Ultrasound of the abdominal organs: the left lobe of the liver is 43 mm, the right lobe of the liver is 120 mm, the echostructure is homogeneous, the vessels and ducts are not dilated, the common bile duct is 4 mm, the portal vein is 11 mm. Radiologically, a single Kloiber cup is not clearly visible in the right half of the abdomen. After infusion therapy (solutions of electrolytes and glucose in a volume of 3 l), taking antispasmodics, cerucal, the patient noted an improvement, which was manifested by a decrease in abdominal pain, relief of nausea and vomiting. There was an independent scanty chair.
On March 30, against the background of complex therapy, the patient's abdominal pain intensified again, nausea and vomiting of stagnant intestinal contents appeared. After preoperative preparation, the patient was operated on. A midline laparotomy was performed. In the abdominal cavity there is a serous effusion up to 1 liter. The greater omentum is soldered to the anterior abdominal wall, the adhesions are sharply dissected. During the audit, it was established that the entire large intestine was located in the left half of the abdomen, fixed in the form of a double-barreled shotgun, which did not cause disruption of passage through the intestine. The small intestine is located on the right, there is a common mesentery with the large intestine, which was regarded as an incomplete rotation of the large intestine, corresponding to the fifth month of embryogenesis. The stomach and small intestine are swollen to 4-5 cm in diameter, the wall of the small intestine is infiltrated. 100 cm from the ileocecal angle, a loop of the small intestine is located under a membranous formation that creates a pocket of the right iliac fossa measuring 10.0x7.0 cm, where it is pinched. The underlying sections of the small and large intestine are collapsed. A 60 cm loop of small intestine was freed from adhesions and declared viable. During further revision, the membranous formation constituting the anterior wall of the pocket was excised to the serous membrane of the duodenum, small intestine, and parietal peritoneum. Nasointestinal intubation of the small intestine was performed with removal of 1 liter of intestinal contents. The abdominal cavity is drained through a counter-aperture.
Postoperative diagnosis: anomaly of intestinal development, incomplete rotation of the colon, strangulated internal hernia, strangulated small intestinal obstruction, adhesive disease, diffuse serous peritonitis. The postoperative period proceeded without complications. The nasointestinal tube was removed on the 3rd day. Independent stool appeared on the 4th day. The patient was discharged after recovery in satisfactory condition on the 8th day after surgery. Examined a month later: abdominal pain is not bothersome, stool is regular, regular, the postoperative scar is without any features.
The above clinical observation indicates that the cause of acute intestinal obstruction may be an abnormality of intestinal development, which often manifests itself in adulthood. The clinical picture of acute intestinal obstruction may be blurred. In this observation, there was a combination of two types of anomalies in the development of the colon - incomplete rotation of the colon and the presence of a membranous formation. A thorough examination of the abdominal cavity during surgery made it possible to choose adequate treatment tactics.
The authors declare no conflict of interest.