Surgeries for pancreatic cancer can be performed to radically remove the tumor, or palliatively, to reduce the volume of tumor tissue and/or eliminate life-threatening complications.
- Pain due to malignant tumors of the pancreas
- Types of surgical intervention for malignant tumors of the pancreas
- Recovery
- Forecast
In most cases, malignant pancreatic tumors are diagnosed at late stages, so radical surgery is possible in approximately 15% of patients. It is worth noting that such operations are lengthy, voluminous, traumatic and are associated with a high risk of complications both in the intraoperative and postoperative periods. At the same time, this is the only method of radical treatment that can extend the patient’s life by several years.
When choosing treatment tactics, doctors rely on the NCCN criteria for pancreatic cancer resectability, which define resectable, unresectable and borderline tumors.
Pancreatic tumor resectability status:
- the tumor does not affect the superior mesenteric artery;
- the celiac trunk and hepatic artery are intact;
- The superior mesenteric vein and portal vein are patent.
State of borderline operability of the tumor:
- the superior mesenteric vein is infiltrated by the tumor to less than half of its circumference, or there is contact of the tumor foci with the wall of the vessel;
- the sheath of the hepatic artery is infiltrated over a short distance. In this case, the operating doctor must be prepared for resection of the vessel followed by plastic surgery;
- it is possible that a short segment of the superior mesenteric vein or portal vein may be involved in the tumor process, while the wall of the vessel above and below the site of infiltration should be absolutely unchanged.
Signs of unresectable tumor:
- the circumference of the superior mesenteric artery is infiltrated by more than half;
- tumor infiltration of the celiac trunk, in which there is no possibility of performing reconstructive plastic surgery after removal of the affected segment of the vessel;
- complete occlusion of the superior mesenteric vein and/or portal vein.
It should be borne in mind that borderline resectable tumors are a very relative term. Previously, it was believed that the involvement of vascular formations in the process was an obstacle to surgical treatment. Modern surgical capabilities make it possible to remove the tumor and restore the integrity of the vascular reservoirs using allogeneic grafts. The possibility of performing such operations depends on the skills of the operating surgeon and the technical equipment of the clinic, therefore patients with signs of borderline resectability are recommended to be referred to higher-level medical institutions to obtain a second expert opinion and re-evaluate resectability.
Medical indications
Many victims of destabilized pancreatic function do not agree to undergo partial excision - resection until the very end, believing that the resulting disability will ruin their life. Doctors insist that modern pharmacology, coupled with a competent approach to the recovery period, works almost miracles. If the victim adheres to a certain set of rules of behavior and nutrition, then after the operation he will come to his senses quickly and will again be able to work and do what he loves.
Many people are frightened by the fact that diabetes mellitus is among the possible side effects of surgery. But, according to statistics, this complication occurs only in 50% of clinical cases.
Before referring a person for resection, the doctor will definitely do everything to avoid radical measures. This even applies to situations where the patient is diagnosed with a neoplasm. First, the treating specialist must make sure whether it is benign or malignant. For this purpose, auxiliary diagnostic formats are used, such as computed tomography with contrast or biopsy. The latter allows you to determine the exact type of tumor found. Pancreatectomy also helps determine the type of treatment.
If the treatment program with standard medications did not produce the expected results, or was rejected from the very beginning due to insufficient productivity, then resection is prescribed. Before her, the victim is sent to undergo a series of tests:
- electrocardiogram;
- radiography;
- coagulogram;
- blood tests, including biochemical;
- ultrasound examination of the abdominal cavity;
- endoscopy.
Having received the results of all the listed examinations, the expert takes note of the current complaints of the applicant, his medical history and other data from the medical card, including hereditary disposition. Based on the information collected, a person may be prescribed a partial resection, which is a mandatory measure if:
- exacerbation of chronic pancreatitis;
- mechanical injury;
- destruction of the integrity of the organ, which is associated with rupture and crushing;
- neoplasms of a malignant nature such as carcinoma;
- cyst formation;
- the presence of a fistula;
- necrotic tissue pathologies.
Sometimes the reason for transfer to the inpatient gastroenterology department for surgery is some rare acquired or congenital disease, which is more related to atypical manifestations.
Forecast
Radical surgery for a malignant pancreatic tumor is the only way to completely eliminate cancer. If relapses occur, a decision is made on the choice of further treatment tactics. This may be chemotherapy, radiotherapy, hormonal treatment and other methods.
Euroonco doctors have extensive experience in treating patients suffering from pancreatic cancer. Despite the rather aggressive form of the disease, patients diagnosed with pancreatic cancer can always be helped. In some cases, it is possible to achieve an increase in life expectancy, in others - pain relief and improved quality of life.
Book a consultation 24 hours a day
+7+7+78
Classification of resections
There are several varieties of this format of surgical intervention, which differ in the procedure, the amount of material excised, as well as the characteristics of the localization of the lesion.
Modern classification implies the following divisions:
- distal;
- corpocaudal;
- removal of the head and tail.
The distal variation involves partial removal of the tail and part of the body of the gland on the left side. The corpocaudal version is aimed at freeing the patient from a cancerous tumor. It is usually localized both inside the pancreas itself and in its caudal compartment. Due to anatomical features, surgeons remove the spleen along with the pancreas. Such a complex intervention is called splenectomy.
Separately, situations are considered when the detected tumor turns out to be inoperable. Then we have to use palliative treatment. This means that the technique is not characterized by complete removal of the problem area using radical measures.
Regardless of which course of surgery is chosen, it should only be carried out by a qualified specialist in conjunction with a professional medical team. It is especially difficult if the victim is scheduled for a Frey operation or a combined gastrectomy, which involves many hours of work to save the person.
Every doctor tries to preserve healthy pancreatic tissue as much as possible so that they continue to perform their direct duties. But sometimes this is quite difficult due to the need to adhere to the rules of lymph node dissection. We are talking about the simultaneous removal of fiber along with the vascular network and lymph nodes located near the problem area.
No less difficult in practice are laparotomy or total resection, which involves excision of the entire organ, often together with neighboring ones. Typically, part of the stomach, as well as the spleen and duodenum, are included under the scalpel.
Disability due to pancreatitis
To find out whether pancreatitis is classified as a disability group, the patient will need to undergo a medical and social examination (MSE). Only a commission consisting of appropriate specialists has the authority to decide whether to assign a person a disability status and all related benefits.
The responsibilities of the attending physician include issuing a patient referral for examination if the following aspects are present:
- second or third degree chronic form of the disease;
- the occurrence of frequent bleeding;
- the presence of deep vein thrombosis with a disorder of the functional activity of the pelvic organs and legs;
- conditions after surgery accompanied by moderate or severe digestive dysfunction;
- postoperative status, complicated by the appearance of a long-term non-healing external fistula.
The decision to grant disability for pancreatitis is made after the MSA
For MSA, the patient will need to obtain from the attending physician a list of necessary documents, based on the results of which the commission will draw conclusions regarding the establishment of the disability group. At the same time, the patient must have in his hands: a medical card, an extract from the hospital, the results of all examinations, etc.
Head resection
In medical practice, resection of the head part is considered one of the most popular options for intervention on the pancreas. This is explained by the fact that for some reason a tumor or cyst is most often localized there.
To increase the chances of a successful early recovery, the surgical procedure is divided into several stages:
- removal of the affected area;
- excision of affected adjacent areas from adjacent internal organs;
- restoration of the integrity of the working ducts;
- reconstruction of the digestive canal;
- restoration of gallbladder functionality.
To get to the gland, which is far hidden in the abdominal cavity, doctors use general anesthesia. But here you should pay close attention to those people who have not experienced anesthesia before. They should first conduct an allergy test to avoid the risk of anaphylactic shock.
In order to free up his viewing angle, the expert uses special equipment - a laparoscope, and the operation itself is labeled laparoscopic.
Using a high-precision device, it will be possible to study the condition of the organs, as well as examine the intended area for surgery. At the very beginning, the specialist is obliged to block the vessels that feed the pancreas. Then the main phase is carried out, and everything ends with the reconstruction of the digestive system.
To do this, it is necessary to articulate the pancreas with the intestines and stomach, for which anastomoses are used. This means that some organs will be connected to each other so that they “learn” to do the work of those that had to be removed.
Functions of the pancreas
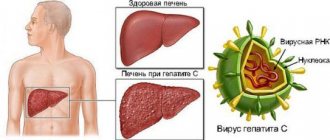
The main function of the pancreas is to produce enzymes to ensure the functioning of the digestive system.
They influence the breakdown of proteins, carbohydrates and fats, as well as the formation of the so-called bolus of food, which passes further along the digestive tract. Without the normal functioning of this gland, the process of assimilation of food and metabolism will be disrupted. The cause of organ dysfunction can be bad habits, alcohol consumption, or too fatty foods. As a result, the most common disease can occur - pancreatitis. In the absence of inflammation, neoplasms and cysts, a stable state can be achieved by following a special diet. In other cases, surgery is required.
However, experts themselves recommend this method of treatment in the most extreme cases. After all, the pancreas is an extremely delicate organ and it is quite difficult to predict the consequences of the operation. Even if the operation is successful, this does not guarantee re-inflammation of the organ. Prolonged inflammation and acute pancreatitis of the pancreas can transform into cancer of the organ.
When should the tail be removed?
To increase the chances of a successful outcome, tail resection is almost always accompanied by removal of the spleen. To reduce the load on the body, you first need to ligate an entire group of vessels. Only after this a sphincter is applied to the tail element and the affected section of the pancreas is intersected.
According to the protocol, the next phase is the application of a special surgical thread called a ligature. It is applied on the formed stump - the place where the tail is cut. At the same time, it is necessary to monitor the prevention of excessive bleeding, which is done by ligating the vessels.
After partial pancreatotomy, possible negative consequences practically disappear. This means that the risks of subsequent development of diabetes mellitus tend to zero. The final step involves drainage with closure of the abdominal cavity.
Other radical operations
Other types of surgical interventions are used less frequently.
Distal pancreatosplenectomy is performed if the tumor appears in the tail of the pancreas. The doctor removes this part of the organ, as well as the spleen. These operations are rarely used. First, cancer develops less frequently in the tail of the pancreas. Secondly, it is detected later because it does not cause jaundice. As a result, neoplasms are detected at a late stage, when radical surgical intervention is impossible.
A total pancreatectomy involves removing the entire pancreas. After such an operation, the patient is forced to receive replacement therapy with insulin and pancreatic enzymes for life. Surgical intervention is used only if the tumor does not extend beyond the pancreas, affects different parts of the organ and does not grow into large vessels.
Minimally invasive surgeries
- Remote consultation
- We will select the best treatment for you
Call me back!
Relevance of pancreatic body resection
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
Removal of the gland body is sometimes a forced measure, which should not be resisted for the sake of maintaining overall normal health. Unlike the tail and head parts, the body is cut along the line of the lower edge. This means that the posterior side of the peritoneum is taken as the starting point.
This is followed by a bypass from below the pancreas to carefully free it from the built-up fiber. Only after this can we move on to studying the vessels and spleen. As soon as the sphincter is applied, it is allowed to cross the corresponding section of the organ.
To protect the mesenteric vessels, the surgeon will definitely use a Kocher probe. And if there was heavy bleeding during the process, then it is intercepted with the help of so-called mosquitoes, and then completely bandaged.
The distal part is required for resection, after which the doctor cuts a flap from the omentum to cover the proximal segment. This means that the cut out soft fabric should cover the piece located closer to the center. The result is a subtotal operation, when only the problematic part is excised.
For the success of transverse resection, a purse-string suture is used, which perfectly covers even an extensive wound surface.
Rehabilitation process after pancreatectomy
Even in the absence of complications, the rehabilitation process after removal of the pancreas takes a long period of time, but the prognosis is favorable. After the operation, a strict diet, large amounts of medication and insulin injections are prescribed.
It will take a lot of time for the body to recover. The patient will be tormented by painful sensations for a long time. However, they can be minimized by taking painkillers. The moral support of family and friends may be much more important for the patient.